- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Blog
Follow our blog and stay up to date.
CAC: The Ultimate Test for Assessing Health and Why You Need One Now!
By Stephen Fitzmeyer, MD
Introduction
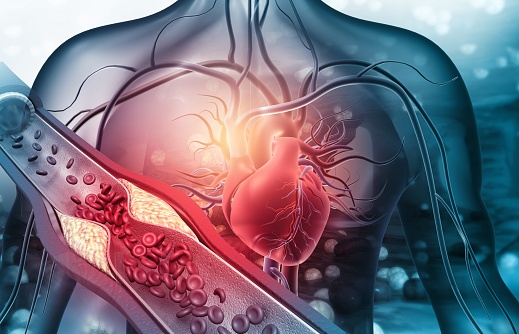
In the realm of healthcare, staying proactive and prioritizing preventive measures is key to maintaining optimal health. The Coronary Artery Calcium (CAC) scoring test has recently emerged as a groundbreaking tool in health assessment, providing invaluable insights into cardiovascular health. This article highlights the significance of CAC as the ultimate test for assessing health and emphasizes why individuals should consider getting one now to safeguard their well-being. Additionally, we’ll explore how patients can easily obtain a CAC scan for themselves.
Understanding CAC Scoring
The Coronary Artery Calcium (CAC) scoring test employs non-invasive computed tomography (CT) scans to detect the presence and extent of calcified plaque in the coronary arteries. By quantifying the amount of calcium present, it calculates a CAC score, effectively gauging the overall burden of atherosclerosis in the arteries. This score serves as a crucial predictor of cardiovascular disease (CVD), empowering individuals to take preventive action.
The Urgency of CAC as a Health Indicator
- Early Detection of Silent Risks: CAC scoring enables early detection of potential cardiovascular issues, even before symptoms manifest. By identifying calcified plaque deposits, healthcare professionals can determine an individual’s risk of experiencing a heart attack or developing coronary artery disease (CAD). Seeking a CAC test now can help unveil hidden risks and prompt timely interventions to prevent disease progression.
- Personalized Risk Assessment: Unlike traditional risk assessment tools, CAC scoring provides a precise evaluation of atherosclerosis. Through quantitative analysis, it offers a more accurate estimation of an individual’s risk of developing CVD. Obtaining a CAC score now empowers healthcare providers to devise personalized treatment plans tailored to an individual’s level of risk, enabling timely interventions and better health outcomes.
- Empowerment for Lifestyle Changes: CAC scoring serves as a powerful motivator for individuals to adopt healthier lifestyles. Witnessing the presence and extent of calcified plaque acts as a visual reminder of the importance of positive changes in diet, exercise, and stress management. By getting a CAC test now, you can proactively take charge of your health, making informed decisions and fostering long-term adherence to beneficial lifestyle modifications.
- Preventive Measures for Long-Term Health: CAC scoring facilitates proactive preventive measures by categorizing individuals into different risk groups based on their CAC scores. This allows healthcare providers to implement appropriate treatments and interventions to reduce the risk of CVD. Taking action now, based on your CAC score, can significantly improve your long-term cardiovascular health and well-being.
How to Obtain a CAC Scan
To obtain a CAC scan, you can follow these steps:
- Consult Your Healthcare Provider: Schedule an appointment with your healthcare provider to discuss your interest in getting a CAC scan. They will evaluate your medical history, risk factors, and overall health to determine if a CAC scan is appropriate for you.
- Referral and Imaging Facility: If your healthcare provider determines that a CAC scan is necessary, they will provide you with a referral to an imaging facility or radiology center equipped to perform the scan.
- Schedule the Scan: Contact the recommended imaging facility and schedule your CAC scan appointment. They will provide you with any necessary instructions, such as fasting requirements or medication restrictions before the test.
- The CAC Scan Procedure: During the CAC scan, you will lie on a table that moves through a CT scanner. The scan is quick and painless, typically taking only a few minutes to complete.
- Results and Follow-up: Once the scan is complete, the radiologist will analyze the images and calculate your CAC score. Your healthcare provider will then review the results with you. They will explain the implications of your CAC score, discuss any necessary lifestyle modifications or medical interventions, and develop a personalized plan to mitigate your cardiovascular risk.
Conclusion
The Coronary Artery Calcium (CAC) scoring test is a powerful tool for assessing cardiovascular health and preventing future complications. By identifying silent risks, providing personalized risk assessment, motivating lifestyle changes, and enabling proactive preventive measures, CAC scoring empowers individuals to take control of their well-being. To obtain a CAC scan, consult your healthcare provider, obtain a referral to an imaging facility, schedule the scan, and discuss the results and follow-up plan with your healthcare provider. Take the proactive step towards optimizing your health and consider getting a CAC scan now. Your heart and overall well-being will thank you for it.
CAC Score
After undergoing a CAC scan, you will receive a CAC score that falls within a specific range. Here are the general ranges and their corresponding meanings:
- CAC Score of 0: A CAC score of 0 indicates the absence of detectable calcified plaque in the coronary arteries. This suggests a very low risk of cardiovascular events, and individuals in this range often have a favorable prognosis.
- CAC Score of 1-99: A CAC score between 1 and 99 indicates the presence of mild calcification in the coronary arteries. This range signifies a low to moderate risk of cardiovascular disease, and it is an opportunity for individuals to implement preventive measures to reduce the progression of plaque formation.
- CAC Score of 100-399: A CAC score between 100 and 399 represents the presence of moderate calcification in the coronary arteries. This range suggests a significant risk of cardiovascular disease, and it necessitates more aggressive preventive strategies and medical interventions to reduce the risk of future complications.
- CAC Score of 400 or Higher: A CAC score of 400 or higher indicates extensive calcification in the coronary arteries. This range represents a high risk of cardiovascular disease, including heart attacks and strokes. It necessitates immediate and intensive medical interventions, including lifestyle modifications and potential medication therapies, to mitigate the risk and prevent further progression.
By understanding the range of CAC scores and their implications, individuals can work closely with their healthcare providers to develop a personalized plan that addresses their specific risk level.
To obtain a CAC scan, consult your healthcare provider, obtain a referral to an imaging facility, schedule the scan, and discuss the results and follow-up plan with your healthcare provider. Take the proactive step towards optimizing your health and consider getting a CAC scan now. Your heart and overall well-being will thank you for it.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
From Cholera to COVID-19: The Role of Epidemiology in Disease Outbreaks
By Stephen Fitzmeyer, MD
The cholera outbreak in 1854 in London, and the work of John Snow, is considered a turning point in the field of epidemiology. The outbreak caused thousands of deaths and was traced back to contaminated water from the Broad Street pump. Snow’s investigation led him to identify the source of the outbreak, and he subsequently recommended measures to prevent the spread of cholera.
Fast forward to modern times, and we are facing a new epidemic – COVID-19. The similarities between the two outbreaks are striking, and so are the differences. Like cholera, COVID-19 is a highly contagious disease that spreads through contact with infected individuals or surfaces. However, unlike cholera, COVID-19 is caused by a novel virus that is still not fully understood.
Epidemiology played a crucial role in both outbreaks. In the case of cholera, Snow used epidemiological methods to map the spread of the disease and identify the source of the outbreak. He collected data on the location of cases and the source of water for the affected individuals, and used this data to create a map that showed a clear association between the cases and the Broad Street pump. This data-driven approach was a key factor in his successful intervention.
Similarly, epidemiology has played a critical role in the management of COVID-19. Epidemiologists have been tracking the spread of the disease, identifying risk factors and patterns of transmission, and providing guidance on how to mitigate the spread of the virus. Epidemiological models have been used to predict the course of the pandemic, and to inform public health policies and interventions.
However, there are also significant differences between the two outbreaks. COVID-19 is a much more complex disease than cholera, with a wide range of symptoms and outcomes. The virus is highly contagious and can be spread by asymptomatic carriers, making it much more challenging to control. The development of effective vaccines and treatments has been a major focus of the public health response to COVID-19, and epidemiology has played a critical role in evaluating the effectiveness of these interventions.
In conclusion, the cholera outbreak and the work of John Snow laid the foundation for modern epidemiology, and the lessons learned from that outbreak have helped us manage and control many subsequent disease outbreaks. The COVID-19 pandemic has presented a new set of challenges, but the principles of epidemiology remain essential to understanding and controlling the spread of the virus. By continuing to apply these principles, we can hope to mitigate the impact of the pandemic and prepare for future outbreaks.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Healing Power of Algorithms: Unleashing the Potential of Artificial Intelligence in Medicine
Introduction
Artificial Intelligence (AI) has emerged as a game-changer in the field of medicine, offering new horizons for diagnosis, treatment, and healthcare management. With the ability to process vast datasets and perform complex tasks at speeds unimaginable for humans, AI is poised to revolutionize the healthcare industry. In this article, we explore the tremendous potential of artificial intelligence in medicine and its transformative impact on patient care.
Disease Diagnosis and Early Detection
AI algorithms are becoming proficient at identifying patterns and anomalies in medical images, such as X-rays, MRIs, and CT scans. This capacity can lead to earlier and more accurate diagnoses, ultimately improving patient outcomes. For instance, AI can detect early signs of diseases like cancer, heart conditions, and neurological disorders, allowing for timely intervention.
Personalized Treatment Plans
AI analyzes patient data, including genetic information, medical history, and lifestyle factors, to create personalized treatment plans. By tailoring therapies to individual patients, healthcare providers can optimize the effectiveness of treatment and minimize adverse effects.
Drug Discovery and Development
AI accelerates drug discovery by simulating complex molecular interactions and predicting potential drug candidates. This reduces the time and cost involved in bringing new drugs to market, offering hope for more effective treatments for various diseases.
Clinical Decision Support
AI provides healthcare professionals with real-time decision support by analyzing patient data, suggesting treatment options, and predicting outcomes. It can assist in making informed decisions, reducing medical errors, and ensuring the best possible care.
Healthcare Automation
AI-powered chatbots and virtual assistants are becoming increasingly common in healthcare. They can answer patient queries, schedule appointments, and provide information on medications and post-treatment care, thus freeing up healthcare professionals’ time.
Predictive Analytics and Population Health Management
AI can analyze patient data to identify at-risk populations, predict disease outbreaks, and improve preventive care. This is particularly valuable for public health initiatives and the management of chronic conditions.
Telemedicine and Remote Monitoring
AI enhances telemedicine by enabling remote monitoring of patients’ vital signs, medication adherence, and general well-being. This approach is especially beneficial for patients with chronic conditions who require continuous care.
Radiology and Pathology Assistance
AI can assist radiologists and pathologists in interpreting medical images by highlighting areas of concern, reducing the chance of oversight, and expediting diagnosis.
Natural Language Processing (NLP) for Medical Records
NLP technologies extract valuable information from unstructured medical records. This aids in clinical research, quality improvement, and more accurate coding for billing and insurance purposes.
Patient Engagement and Wellness
AI-driven health apps and wearables help patients manage their health by tracking vital signs, providing health tips, and sending medication reminders. They also encourage a proactive approach to wellness.
Conclusion
Artificial intelligence has the potential to reshape the landscape of medicine in profound ways. Its ability to analyze data, make predictions, and assist healthcare providers empowers medical professionals to deliver more accurate diagnoses and effective treatments, while also enhancing the patient experience. As AI continues to evolve and integrate into healthcare systems, it holds the promise of improving patient outcomes, reducing healthcare costs, and addressing some of the most pressing challenges in the medical field. The future of medicine is increasingly intelligent, and it is poised to benefit both healthcare providers and patients alike.
Satiety: The Key to Success on a Ketogenic Diet
Introduction:
Embarking on a ketogenic diet can be a transformative journey towards improved health and well-being. This low-carbohydrate, high-fat eating plan has gained popularity due to its potential for weight loss, enhanced metabolic health, and increased mental clarity. However, one often overlooked aspect that holds the key to success on a ketogenic diet is satiety—the feeling of fullness and satisfaction after a meal. In this article, we will explore the importance of satiety and how it plays a crucial role in achieving success on a ketogenic diet.
Understanding Satiety:
Satiety is more than just feeling full—it’s about feeling satisfied and nourished after a meal. Achieving satiety is essential because it helps to prevent overeating, control cravings, and maintain adherence to a ketogenic diet in the long term. When we feel satisfied after a meal, we are less likely to seek out unnecessary snacks or indulge in high-carbohydrate foods that can derail our progress.
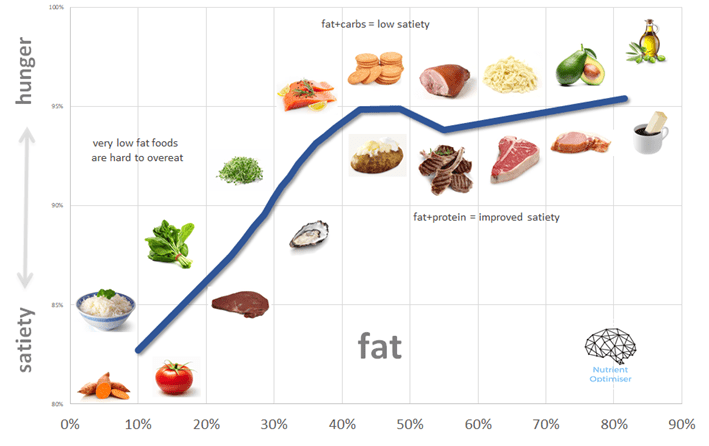
The Role of Macronutrients:
The macronutrient composition of a ketogenic diet plays a significant role in achieving satiety. Here’s how each macronutrient contributes to the feeling of fullness:
- Healthy Fats: Fats are a cornerstone of the ketogenic diet, and they play a crucial role in promoting satiety. Consuming an adequate amount of healthy fats, such as avocados, nuts, seeds, olive oil, and coconut oil, can help slow down digestion, increase feelings of fullness, and provide sustained energy throughout the day.
- Protein Power: Protein is another important macronutrient for satiety on a ketogenic diet. It is known for its ability to promote feelings of fullness and support muscle maintenance. Including high-quality sources of protein, such as fish, poultry, eggs, and tofu, in your meals can help curb cravings and keep you satisfied for longer periods.
- Fibrous Vegetables: Non-starchy vegetables, such as leafy greens, broccoli, cauliflower, and zucchini, are excellent sources of dietary fiber. Fiber adds bulk to meals, promoting a feeling of fullness while providing essential nutrients. Including an abundance of fibrous vegetables in your ketogenic meals can enhance satiety and support overall gut health.
Strategies for Enhancing Satiety on a Ketogenic Diet:
- Prioritize Whole Foods: Emphasize whole, unprocessed foods in your ketogenic diet. These nutrient-dense options provide more satiety compared to processed and refined foods.
- Mindful Eating: Slow down and savor each bite. Mindful eating practices, such as chewing slowly and paying attention to hunger and fullness cues, can help you tune into your body’s satiety signals.
- Balanced Meals: Aim to include a combination of healthy fats, protein, and fiber-rich vegetables in every meal. This balanced approach provides a wide range of nutrients and helps achieve satiety more effectively.
- Hydration: Stay adequately hydrated throughout the day. Sometimes, thirst can be mistaken for hunger, leading to unnecessary snacking. Drinking enough water can help prevent this confusion and support satiety.
- Meal Planning and Preparation: Plan your meals in advance and prepare them at home whenever possible. This allows you to control the quality of ingredients and portion sizes, ensuring that your meals are satisfying and aligned with your ketogenic goals.
Conclusion:
Achieving satiety is a fundamental aspect of success on a ketogenic diet. By prioritizing healthy fats, adequate protein, and fibrous vegetables, you can create meals that not only support ketosis but also promote feelings of fullness and satisfaction. Remember to listen to your body’s signals, practice mindful eating, and make informed choices when it comes to food selection and preparation.
Satiety is not only crucial for short-term satisfaction but also for long-term adherence to a ketogenic lifestyle. By feeling consistently satiated, you can avoid the pitfalls of unnecessary snacking, mindless eating, and the temptation to stray from your dietary goals. The ability to sustain your ketogenic diet with ease increases your chances of achieving your desired health outcomes, whether it’s weight loss, improved metabolic markers, or increased mental clarity.
It’s important to note that individual preferences and needs may vary when it comes to achieving satiety on a ketogenic diet. Experiment with different food combinations, portion sizes, and eating schedules to find what works best for you. Some individuals may find that smaller, more frequent meals work well, while others prefer larger, less frequent meals. Remember, there is no one-size-fits-all approach, and customization is key.
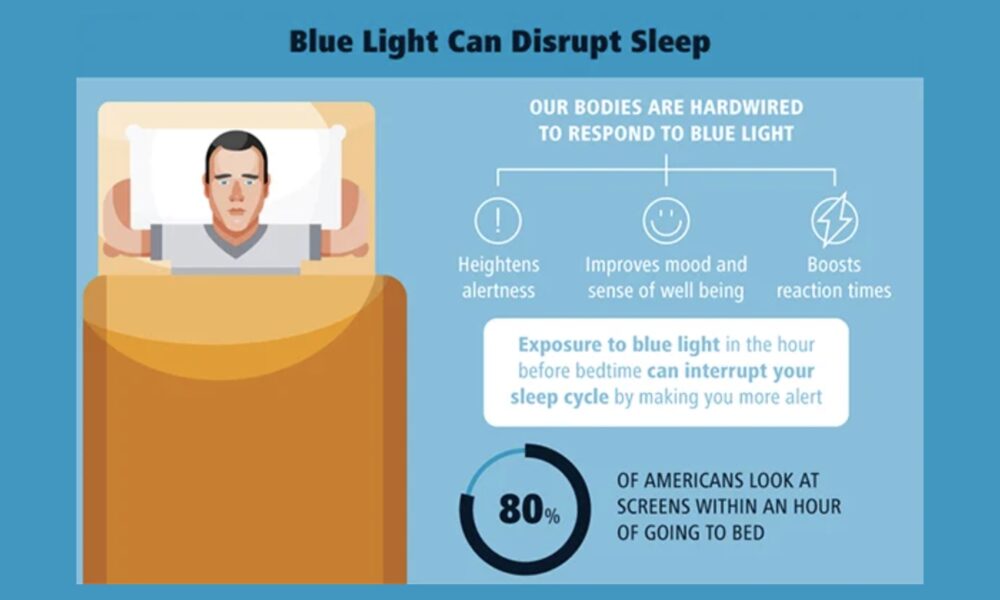
In addition to macronutrient composition and meal planning, factors like stress management, sleep quality, and physical activity also influence satiety. Addressing these lifestyle factors alongside your ketogenic diet can further enhance the feeling of fullness and overall well-being.
Ultimately, satiety is the secret ingredient to success on a ketogenic diet. By focusing on nutrient-dense, whole foods, maintaining a balanced macronutrient profile, and listening to your body’s cues, you can create a sustainable and enjoyable way of eating that supports your health and weight management goals. Embrace the power of satiety and let it guide you on your journey to a healthier, happier you.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Biochemical Pathway of Fat Metabolism: Unleashing Ketones as the Ultimate Fuel Source
Introduction:
The human body is a remarkable machine that possesses the ability to adapt and utilize various fuel sources to meet its energy needs. While carbohydrates have traditionally been considered the primary energy source, the biochemical pathway of fat metabolism unlocks a fascinating alternative: the production of ketones. In this article, we will delve into the intricate pathway of fat metabolism and explore how it leads to the production of ketones, making them a potent and efficient fuel source for our bodies.
The Basics of Fat Metabolism:
Fat metabolism, also known as lipolysis, is the process by which our bodies break down triglycerides stored in adipose tissue to release fatty acids. This process occurs primarily in the mitochondria, the energy powerhouses of our cells. Through a series of intricate biochemical reactions, fatty acids are converted into acetyl-CoA, which serves as a key precursor in the production of ketone bodies.
The Ketogenic Pathway:
Once fatty acids are converted to acetyl-CoA, they enter the biochemical pathway known as ketogenesis. Ketogenesis occurs predominantly in the liver mitochondria and involves the transformation of acetyl-CoA into ketone bodies. The primary ketone bodies produced are acetoacetate, beta-hydroxybutyrate, and acetone.
Acetoacetate is the first ketone body formed, which can be further converted into beta-hydroxybutyrate or spontaneously decarboxylated to produce acetone. Beta-hydroxybutyrate is the most abundant and readily used ketone body, providing an efficient and sustainable energy source for various tissues, including the brain.
The Role of Ketones as a Primary Fuel Source:
Ketones offer several advantages as a primary fuel source for the body:
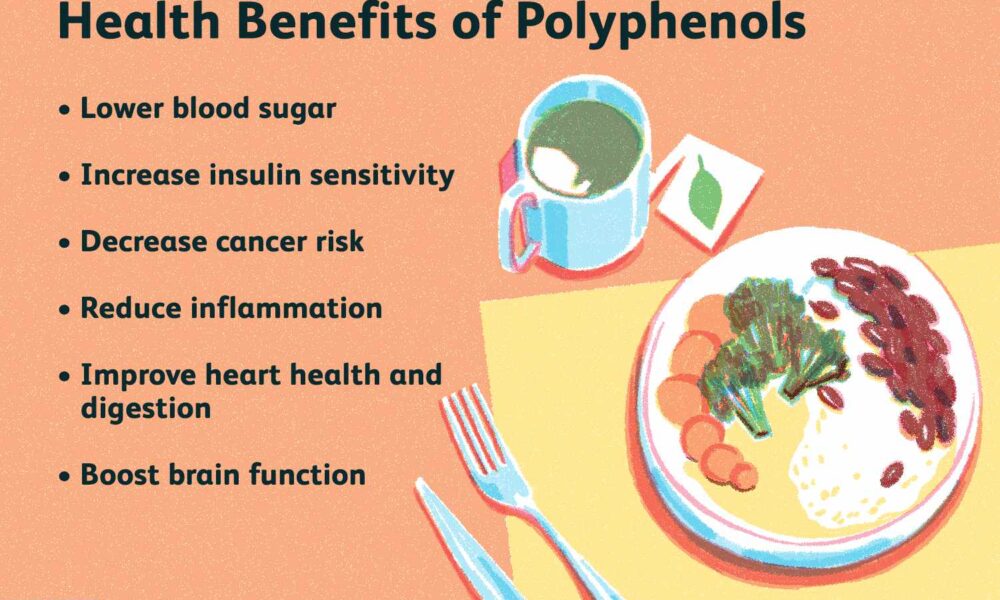
- Enhanced Energy Production: Ketones are metabolized more efficiently than glucose, producing a higher yield of ATP (adenosine triphosphate), the cellular energy currency. This increased energy output fuels the body’s cells and supports optimal physiological functions.
- Stable Blood Sugar Levels: Unlike carbohydrates, which can lead to blood sugar spikes and crashes, ketones provide a stable and steady source of energy. This stability helps prevent energy fluctuations, enhances mental clarity, and reduces cravings for quick-fix carbohydrates.
- Preservation of Lean Muscle Mass: When the body enters a state of ketosis, it becomes proficient at utilizing stored fat as its primary fuel source, sparing muscle protein from being broken down for energy. This preservation of lean muscle mass is vital for maintaining overall body composition and metabolic health.
- Neuroprotective Effects: The brain is highly dependent on a consistent energy supply. Ketones serve as an alternative fuel source for the brain when glucose availability is limited. This feature is particularly beneficial in conditions like Alzheimer’s disease, where brain glucose metabolism is impaired.
Conclusion:
The biochemical pathway of fat metabolism that leads to the production of ketones presents a remarkable alternative energy source for our bodies. By harnessing the power of ketones, we can tap into an efficient and sustainable fuel supply that offers numerous benefits, including enhanced energy production, stable blood sugar levels, muscle preservation, and potential neuroprotective effects.
Understanding the intricacies of fat metabolism and the production of ketones sheds light on the potential of adopting a ketogenic diet or incorporating intermittent fasting practices. These approaches can optimize fat metabolism, induce nutritional ketosis, and unlock the full potential of ketones as a primary fuel source.
It is important to note that individual responses to a ketogenic diet may vary, and consulting with a healthcare professional is essential, especially for those with underlying health conditions. With a deeper understanding of the biochemical pathway of fat metabolism and the power of ketones, we can make informed choices to support our metabolic health and overall well-being.
While a ketogenic diet can be a valuable tool for harnessing the benefits of ketones, it’s crucial to approach it with careful consideration. Adhering to a well-formulated ketogenic diet involves consuming adequate healthy fats, moderate protein, and minimal carbohydrates. Individual needs, goals, and potential underlying health conditions should be taken into account when adopting a ketogenic lifestyle.
Incorporating intermittent fasting (IF) alongside a ketogenic diet can further enhance the production and utilization of ketones. IF involves cycling between periods of eating and fasting, allowing the body to tap into its stored fat for energy. This combination of a ketogenic diet and IF can accelerate the transition into ketosis and amplify the metabolic benefits associated with ketone utilization.
However, it’s important to note that a ketogenic diet and IF may not be suitable for everyone. Pregnant or breastfeeding individuals, those with certain medical conditions, and individuals on specific medications should consult with their healthcare providers before making any significant dietary changes.
In conclusion, understanding the biochemical pathway of fat metabolism that leads to the production of ketones unveils the potential of ketones as a primary fuel source for our bodies. By adopting a well-formulated ketogenic diet and potentially incorporating intermittent fasting, we can tap into the benefits of ketones, including enhanced energy production, stable blood sugar levels, muscle preservation, and potential neuroprotective effects.
As with any dietary approach, it is important to listen to our bodies, prioritize nutrient-dense foods, and make informed choices based on individual needs and goals. Whether you choose to embrace a ketogenic diet or explore other nutritional strategies, the knowledge of fat metabolism and ketone production empowers us to optimize our health and unlock the potential of our bodies’ incredible metabolic machinery.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/