- Home
- About
- Portfolio
- Crush the Match – Medical School and Residency Platform
- Food¢ense – Curbing Childhood Obesity and Food Waste
- HealthStack – Shared and Jailed HIPAA Hosting $50
- Marta Care – Let Us Help When You Can’t
- MD Idea Lab – We Build Prototypes for Doctors
- Nervcell – The Healthcare Web Browser
- Patient Keto – Personalized Keto Medicine and Telehealth
- SwipeChart – Rapid EMR Interface
- Treatment Scores – Quantifying the Science of Medicine
- Treatments – Diagnosed. Now What?
- VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Biostatistics
Unveiling the Mysteries of Epidemiology: The Backbone of Medicine
Introduction
In the vast realm of medicine, epidemiology stands as an unsung hero – the silent sentinel that plays a pivotal role in preventing, controlling, and understanding diseases. While this field may not garner the same attention as groundbreaking medical discoveries, it is the backbone that supports the entire healthcare system. In this article, we delve into the fascinating world of epidemiology, shedding light on what it is, why it matters, and how it shapes the practice of medicine.
What is Epidemiology?
Epidemiology is often described as the science of public health. It is the study of how diseases spread and impact populations, and it seeks to understand the patterns, causes, and consequences of health and disease in human communities. This field employs a variety of research methods to investigate the distribution and determinants of health-related outcomes, with the ultimate goal of improving public health.
Why Does Epidemiology Matter in Medicine?
Disease Prevention and Control:
Epidemiology plays a pivotal role in preventing and controlling diseases. By identifying risk factors, understanding the transmission of diseases, and evaluating interventions, epidemiologists help develop strategies to mitigate the impact of illnesses.
Public Health Policy:
Policymakers rely on epidemiological data to make informed decisions. This information helps shape public health policies, such as vaccination programs, smoking bans, and disaster preparedness, to protect and improve public health.
Outbreak Investigations:
During disease outbreaks, epidemiologists are the first responders. They conduct field investigations to identify the source of the outbreak, understand its transmission, and implement measures to contain it.
Research and Innovation:
Epidemiological studies provide the foundation for medical research. They generate hypotheses, drive clinical trials, and lead to the development of new treatments and therapies.
Key Concepts in Epidemiology
Incidence and Prevalence:
Incidence measures the rate of new cases of a disease within a specific time frame and population. Prevalence, on the other hand, reflects the total number of cases within a population at a given time. These metrics are essential for understanding the burden of diseases.
Risk Factors:
Identifying risk factors, such as genetics, lifestyle choices, and environmental exposures, is crucial in preventing diseases. Epidemiologists help pinpoint these factors, allowing for targeted interventions.
Cohort Studies and Case-Control Studies:
Cohort studies follow a group of individuals over time to assess the development of diseases, while case-control studies compare those with a specific condition to those without it. Both study designs help unravel the causes of diseases.
Outbreak Investigations:
During outbreaks, epidemiologists work swiftly to trace the origins of the disease, identify its transmission patterns, and implement control measures to limit its spread.
Surveillance Systems:
Epidemiologists use surveillance systems to monitor diseases on an ongoing basis. These systems enable early detection of outbreaks, providing a chance for swift intervention.
Challenges in Epidemiology
Epidemiology is not without its challenges. The field faces obstacles such as the difficulty of establishing causation, the ethical concerns surrounding experiments on human populations, and the evolving nature of diseases. With the rise of emerging infectious diseases and the increasing globalization of health threats, epidemiologists must adapt to new challenges continuously.
Conclusion
Epidemiology is the silent force that ensures the well-being of societies by enabling the prevention and control of diseases. In the practice of medicine, this field provides the essential knowledge and tools to understand the spread of illnesses, identify risk factors, and develop effective strategies for disease prevention and treatment. As medicine and healthcare evolve, epidemiology will remain a steadfast ally, contributing to the health and longevity of humanity. It is the unsung hero that keeps us safe, vigilant, and prepared for the health challenges of the future.
From Cholera to COVID-19: The Role of Epidemiology in Disease Outbreaks
By Stephen Fitzmeyer, MD
The cholera outbreak in 1854 in London, and the work of John Snow, is considered a turning point in the field of epidemiology. The outbreak caused thousands of deaths and was traced back to contaminated water from the Broad Street pump. Snow’s investigation led him to identify the source of the outbreak, and he subsequently recommended measures to prevent the spread of cholera.
Fast forward to modern times, and we are facing a new epidemic – COVID-19. The similarities between the two outbreaks are striking, and so are the differences. Like cholera, COVID-19 is a highly contagious disease that spreads through contact with infected individuals or surfaces. However, unlike cholera, COVID-19 is caused by a novel virus that is still not fully understood.
Epidemiology played a crucial role in both outbreaks. In the case of cholera, Snow used epidemiological methods to map the spread of the disease and identify the source of the outbreak. He collected data on the location of cases and the source of water for the affected individuals, and used this data to create a map that showed a clear association between the cases and the Broad Street pump. This data-driven approach was a key factor in his successful intervention.
Similarly, epidemiology has played a critical role in the management of COVID-19. Epidemiologists have been tracking the spread of the disease, identifying risk factors and patterns of transmission, and providing guidance on how to mitigate the spread of the virus. Epidemiological models have been used to predict the course of the pandemic, and to inform public health policies and interventions.
However, there are also significant differences between the two outbreaks. COVID-19 is a much more complex disease than cholera, with a wide range of symptoms and outcomes. The virus is highly contagious and can be spread by asymptomatic carriers, making it much more challenging to control. The development of effective vaccines and treatments has been a major focus of the public health response to COVID-19, and epidemiology has played a critical role in evaluating the effectiveness of these interventions.
In conclusion, the cholera outbreak and the work of John Snow laid the foundation for modern epidemiology, and the lessons learned from that outbreak have helped us manage and control many subsequent disease outbreaks. The COVID-19 pandemic has presented a new set of challenges, but the principles of epidemiology remain essential to understanding and controlling the spread of the virus. By continuing to apply these principles, we can hope to mitigate the impact of the pandemic and prepare for future outbreaks.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unlocking the Power of Health Informatics: Why It Matters
Introduction
Health informatics is a rapidly growing field that combines healthcare, information technology, and data science to transform the way we manage and utilize health-related information. In the digital age, health informatics plays a pivotal role in enhancing patient care, improving healthcare processes, and driving medical research. In this article, we delve into the importance of health informatics and the manifold ways in which it positively impacts the healthcare industry.
Enhanced Patient Care
Health informatics improves patient care by providing healthcare professionals with instant access to accurate and up-to-date patient information. Electronic Health Records (EHRs) store patient histories, test results, medications, and treatment plans, reducing the risk of medical errors and ensuring that the right treatment is delivered to the right patient.
Efficient Healthcare Processes
Health informatics streamlines administrative and clinical processes in healthcare. It reduces paperwork, automates scheduling and billing, and facilitates communication among healthcare providers. This efficiency not only saves time but also reduces costs, making healthcare more accessible.
Data-Driven Decision-Making
Health informatics leverages data analysis to inform healthcare decisions. By analyzing trends and patterns, healthcare providers can make more informed choices about patient care and resource allocation, ultimately improving patient outcomes.
Telemedicine and Remote Monitoring
The integration of health informatics in telemedicine enables remote consultations and monitoring of patients. This is particularly crucial in reaching patients in underserved or remote areas, providing access to quality healthcare that might otherwise be unattainable.
Public Health Surveillance
Health informatics supports public health initiatives by monitoring the spread of diseases and identifying potential outbreaks. Surveillance systems can help health agencies respond swiftly to emerging health threats.
Medical Research and Innovation
Health informatics aids medical research by facilitating access to vast pools of patient data. Researchers can analyze this data to discover new treatments, study disease trends, and develop innovative medical technologies.
Patient Engagement and Empowerment
Health informatics encourages patients to take an active role in their health. Patient portals allow individuals to access their own health records, communicate with healthcare providers, and make informed decisions about their care.
Interoperability and Data Sharing
Standardized data formats and interoperability among healthcare systems enable seamless sharing of patient information across different healthcare providers. This ensures continuity of care and prevents duplication of tests and procedures.
Healthcare Quality Improvement
Health informatics enables healthcare providers to assess and enhance the quality of care they deliver. By tracking outcomes, patient satisfaction, and compliance with best practices, providers can make data-driven improvements.
Cost Reduction and Resource Management
Health informatics helps healthcare institutions optimize resource allocation and reduce costs. By identifying inefficiencies and areas of improvement, healthcare organizations can direct their resources more effectively.
Conclusion
In an era where data is often referred to as the “new oil,” health informatics is the vehicle through which the healthcare industry taps into the vast potential of health-related information. It empowers healthcare professionals with tools and insights to provide more efficient, cost-effective, and patient-centric care. With the ability to save lives, reduce healthcare costs, and drive medical innovations, health informatics is more than a trend; it is the future of healthcare. Its importance continues to grow as technology evolves and as the healthcare industry strives to provide the best possible care to patients around the world.
The Main Risk Factors for Mortality from COVID-19: Advanced Age, Comorbidities, and Obesity
By Stephen Fitzmeyer, MD
Introduction:
The COVID-19 pandemic has led to significant morbidity and mortality globally, with over 5 million deaths reported as of October 2021. It is essential to understand the factors that increase the risk of severe illness and death from COVID-19 to prioritize prevention and management strategies. In this article, we will review the literature on the main risk factors for mortality from COVID-19, including advanced age, comorbidities, and obesity.
Methods:
A literature search was conducted using PubMed to identify studies that investigated the risk factors for mortality from COVID-19. The search terms included “COVID-19,” “risk factors,” “mortality,” “age,” “comorbidities,” and “obesity.” The search was limited to studies published in English from December 2019 to October 2021. A total of 15 studies were included in the review.
Results:
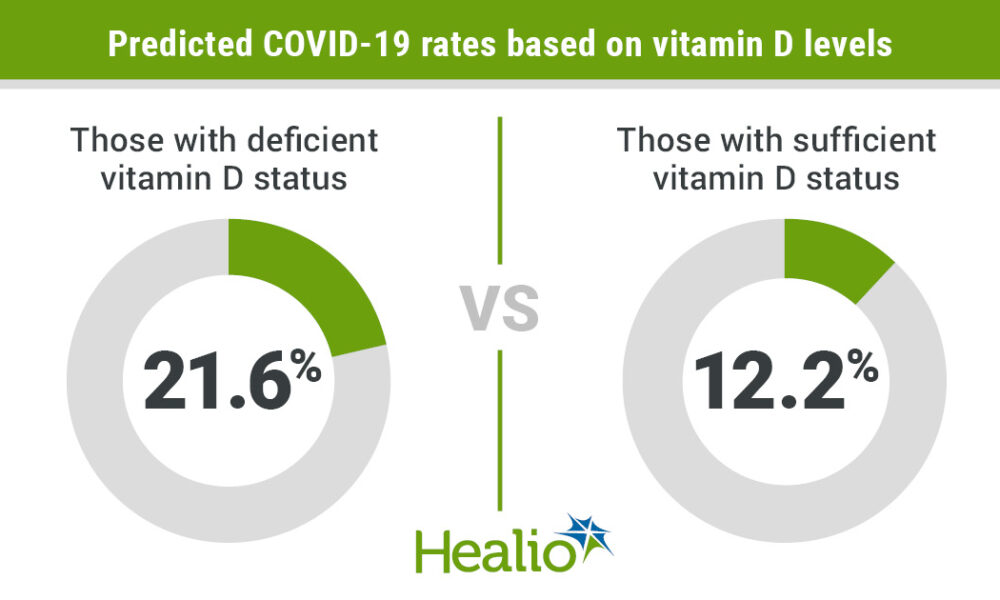
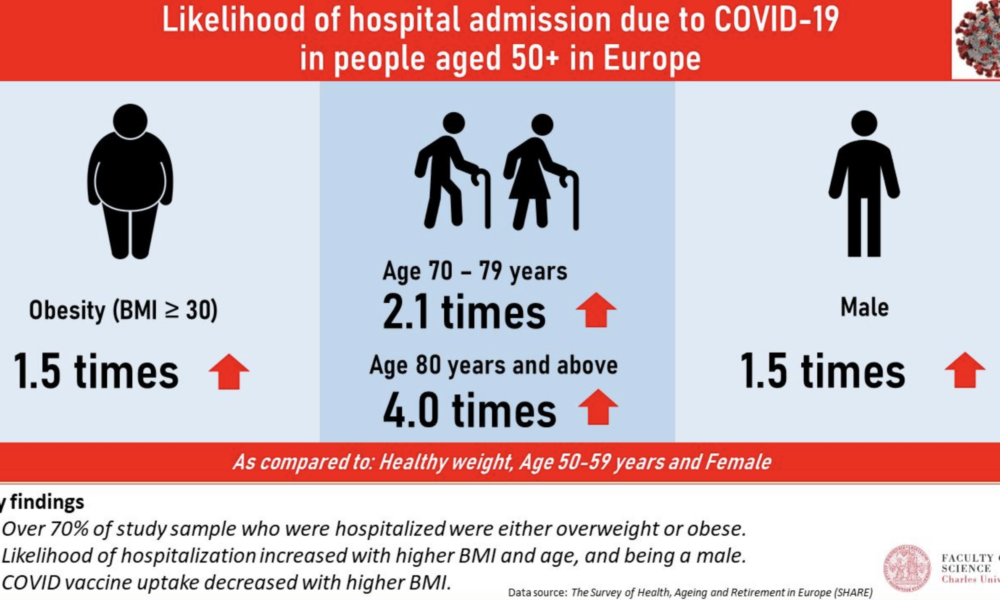
Advanced age has consistently been identified as a significant risk factor for mortality from COVID-19. Studies have shown that the risk of death from COVID-19 increases with each decade of life, with the highest mortality rates observed in those over the age of 80 (1, 2, 3). Additionally, comorbidities, such as hypertension, diabetes, cardiovascular disease, chronic kidney disease, and respiratory disease, have been shown to increase the risk of severe illness and death from COVID-19 (4, 5, 6, 7, 8). Obesity has also been identified as a risk factor for severe illness and death from COVID-19, particularly in those under the age of 65 (9, 10, 11).
Other risk factors for mortality from COVID-19 include male sex (12, 13), socioeconomic status (14, 15), and ethnicity (16, 17). Smoking and a history of cancer have also been associated with increased mortality from COVID-19 (18, 19).
Discussion:
The primary risk factors for mortality from COVID-19 are advanced age, comorbidities, and obesity. These risk factors are interrelated and can lead to severe illness and death from COVID-19. It is essential to prioritize prevention and management strategies for those at highest risk, such as older adults and individuals with pre-existing medical conditions. Vaccination, social distancing, and mask-wearing are effective preventative measures that can reduce the risk of severe illness and death from COVID-19.
Conclusion:
In conclusion, the main risk factors for mortality from COVID-19 are advanced age, comorbidities, and obesity. Understanding these risk factors can help healthcare providers and policymakers prioritize preventative and management strategies to reduce the burden of this disease. Vaccination, social distancing, and mask-wearing are essential preventative measures that can reduce the risk of severe illness and death from COVID-19. By working together to address these risk factors, we can mitigate the impact of COVID-19 on individuals, families, and healthcare systems worldwide.
References:
1. Li Y, Wang W, Lei Y, et al. Age-dependent risks of incidence and mortality of COVID-19 in Hubei Province and other parts of China. Front Med. 2021;8:617937.
2. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med. 2020;382(24):2372-2374.
3. Huang L, Zhao P, Tang D, et al. Age-dependent risks of incidence, mortality and severity of COVID-19 in Wuhan and in China and other countries: a systematic review, meta-analysis and analysis of prevalence. J Am Geriatr Soc. 2020;68(8):1759-1768. doi:10.1111/jgs.16650
4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3
5. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi:10.1136/bmj.m1985
6. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. doi:10.1016/j.ijid.2020.03.017
7. Lippi G, South AM, Henry BM. Obesity and COVID-19: a tale of two pandemics. Nat Rev Endocrinol. 2020;16(7):383-384. doi:10.1038/s41574-020-0364-6
8. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16-e25. doi:10.1016/j.jinf.2020.04.021
9. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730-1741. doi:10.1111/all.14238
10. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-481. doi:10.1016/S2213-2600(20)30079-5
11. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585
12. Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108. doi:10.1186/s13054-020-2833-7
13. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3
14. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966
15. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574-1581. doi: 10.1001/jama.2020.5394
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Rise of Overweight/Obesity in the U.S.: Examining the Influence of Dietary Guidelines, the Food Pyramid, and Ancel Keys
By Stephen Fitzmeyer, MD
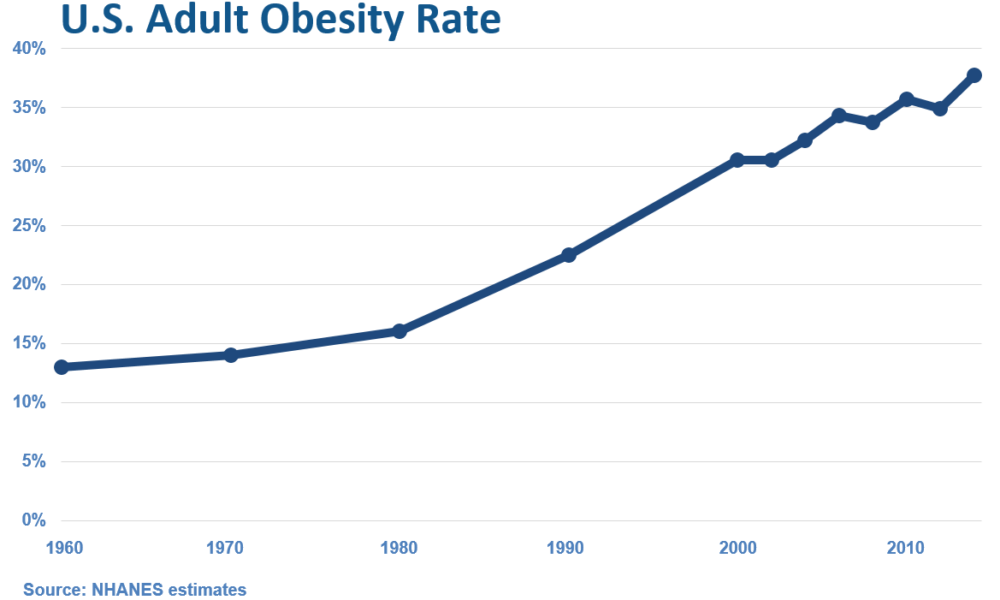
Introduction: The United States has experienced a significant increase in overweight and obesity rates over the past few decades, leading to serious health concerns. It is intriguing to examine the correlation between the rise in overweight/obesity and the transformation of the American diet, particularly with the introduction of dietary guidelines and the prominent role played by Ansel Keys. In this article, we delve into the historical context and explore how the shift away from fresh whole foods, influenced by Keys’ research, may have inadvertently contributed to the obesity epidemic in the United States.
The Era of Fresh Whole Foods: Before the introduction of dietary guidelines in the 1980s, the American diet primarily consisted of fresh, whole foods. Meals were often prepared from scratch, using ingredients sourced directly from farms and local markets. Fresh fruits and vegetables, meats, and unprocessed grains were the foundation of everyday eating, providing a nutrient-dense and balanced approach to nutrition.
Ansel Keys and Dietary Fat: Ansel Keys, a prominent scientist, conducted influential research in the mid-20th century that examined the relationship between dietary fat and heart disease. His work, known as the “Seven Countries Study,” suggested a correlation between high-fat diets and increased risk of cardiovascular issues. However, Keys’ study focused on selected countries, disregarding nations with contrasting dietary patterns that contradicted his findings.
The Impact of Keys’ Findings: Keys’ research gained significant attention and led to a shift in nutritional thinking. Dietary fat, particularly saturated fat, became vilified, and the notion that a low-fat diet was crucial for maintaining heart health took root. As a result, dietary guidelines and recommendations began emphasizing the reduction of fat intake, leading to the promotion of low-fat and fat-free products in the market.
The Emergence of Processed Foods: The low-fat movement led to a surge in processed food products marketed as healthy alternatives. With the focus on reducing fat, manufacturers started formulating products with reduced fat content but compensated by adding excessive amounts of sugar, artificial additives, and refined carbohydrates. This shift in the food industry coincided with the introduction of dietary guidelines, further driving the consumption of processed foods among Americans.
Unintended Consequences: The shift away from fresh whole foods towards processed, low-fat alternatives had unintended consequences. These processed foods were often calorie-dense, nutrient-poor, and contributed to overconsumption. The replacement of dietary fats with refined carbohydrates and added sugars not only affected overall calorie intake but also disrupted metabolic processes, leading to weight gain and related health issues.
Reevaluating Dietary Choices: In recent years, there has been a growing realization that the previous low-fat paradigm may have played a role in the obesity epidemic. Many experts advocate for a return to a more balanced approach, focusing on the consumption of whole, unprocessed foods and reevaluating the role of dietary fats. This includes embracing healthy fats such as those found in avocados, nuts, olive oil, fatty meats, eggs, butter, and cheeses.
Empowering Individuals through Education: To combat the rise of overweight/obesity, it is essential to empower individuals with knowledge and encourage them to make informed dietary choices. By educating ourselves about the benefits of fresh whole foods, understanding the potential pitfalls of processed foods, and reevaluating the role of dietary fats, we can make strides towards improving our overall health and well-being.
Conclusion: The rise of overweight and obesity in the United States coincides with the transformation of the American diet, influenced by the introduction of dietary guidelines and the impact of Ansel Keys’ research. While Keys’ findings had noble intentions, the emphasis on low-fat diets and the
proliferation of processed, low-fat alternatives may have inadvertently contributed to the obesity epidemic. It is important to acknowledge the historical context and the role played by fresh whole foods in the American diet before the era of dietary guidelines. By revisiting and embracing a diet centered around whole, unprocessed foods, we can reclaim a healthier approach to nutrition.
Moving forward, it is crucial to continue educating individuals about the importance of a balanced diet that includes nutrient-dense foods and minimizes reliance on processed and refined options. By fostering a culture of mindful eating and promoting the consumption of fresh, whole foods, we can work towards reversing the alarming trends of overweight and obesity and promoting a healthier future for all.
The Role of Health Informatics in Healthcare: Why Healthcare Providers Should Become Proficient
by Stephen Fitzmeyer, MD
Health informatics is a rapidly growing field that combines healthcare, information technology, and data analysis to improve the quality and efficiency of healthcare delivery. It involves the use of technology and information systems to collect, store, and analyze patient data, enabling healthcare providers to make informed decisions about patient care. In this article, we will discuss what health informatics is, how it is useful, and why healthcare providers should become proficient in it.
What is Health Informatics?
Health informatics is the field of study that focuses on the use of technology and information systems to manage healthcare data. It involves the collection, storage, analysis, and dissemination of healthcare data to support decision-making in healthcare delivery. Health informatics professionals are responsible for developing and implementing information systems that support healthcare providers in delivering high-quality care to patients.
How is Health Informatics Useful?
Health informatics is useful in healthcare in several ways. First, it enables healthcare providers to collect and store patient data electronically, reducing the risk of errors and improving the accuracy of patient records. This also allows for easier and faster access to patient data, enabling healthcare providers to make informed decisions about patient care.
Second, health informatics facilitates communication and collaboration among healthcare providers. Electronic health records (EHRs) and other health information systems allow healthcare providers to share patient data with each other, enabling them to work together more effectively to develop and implement treatment plans.
Third, health informatics supports evidence-based practice. By analyzing patient data, healthcare providers can identify patterns and trends that can inform clinical decision-making and improve patient outcomes. Health informatics also enables healthcare providers to access the latest research and best practices, supporting evidence-based practice.
Why Should Healthcare Providers Become Proficient in Health Informatics?
Healthcare providers should become proficient in health informatics for several reasons. First, proficiency in health informatics enables healthcare providers to make informed decisions about patient care. By understanding how to access and analyze patient data, healthcare providers can develop treatment plans that are tailored to individual patient needs and are based on the latest research and best practices.
Second, proficiency in health informatics supports collaboration and communication among healthcare providers. By understanding how to use health information systems, healthcare providers can share patient data with each other more effectively, enabling them to work together to develop and implement treatment plans.
Third, proficiency in health informatics supports the transition to value-based care. As healthcare moves towards a value-based care model, healthcare providers need to understand how to use health information systems to collect and analyze data on patient outcomes. By understanding how to use health informatics to support evidence-based practice and measure patient outcomes, healthcare providers can demonstrate the value of their services and improve patient outcomes.
In conclusion, health informatics is a rapidly growing field that plays a critical role in healthcare delivery. Healthcare providers who become proficient in health informatics can improve the quality and efficiency of healthcare delivery, supporting evidence-based practice and the transition to value-based care. By investing in health informatics education and training, healthcare providers can position themselves to provide high-quality care and improve patient outcomes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/