- Home
- About
- Portfolio
- Crush the Match – Medical School and Residency Platform
- Food¢ense – Curbing Childhood Obesity and Food Waste
- HealthStack – Shared and Jailed HIPAA Hosting $50
- Marta Care – Let Us Help When You Can’t
- MD Idea Lab – We Build Prototypes for Doctors
- Nervcell – The Healthcare Web Browser
- Patient Keto – Personalized Keto Medicine and Telehealth
- SwipeChart – Rapid EMR Interface
- Treatment Scores – Quantifying the Science of Medicine
- Treatments – Diagnosed. Now What?
- VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
- Home
- Warp Core Health
- Blog
- Metabolic Health
Category: Metabolic Health
Sameglutides vs. Physician-Guided Diet for Metabolic Syndrome: A Comprehensive Comparison
- April 10, 2024
- Stephen Fitzmeyer, MD
- No Comments
Introduction:
Metabolic Syndrome is a complex health condition that encompasses a range of risk factors, including obesity, high blood sugar, high blood pressure, and abnormal cholesterol levels. In recent years, medications like Sameglutides, such as Wagovy and Ozempic, have gained popularity for their ability to manage certain aspects of Metabolic Syndrome. However, are these medications a long-term solution, or is there a better approach? Let’s delve into the comparison between Sameglutides and a physician-guided low-carb, high-fat diet for managing Metabolic Syndrome.
Short-Term Benefits of Sameglutides:
Sameglutides like Wagovy and Ozempic belong to a class of medications known as GLP-1 receptor agonists. They work by stimulating insulin production, reducing appetite, and promoting weight loss. These drugs can indeed provide short-term benefits by lowering blood sugar levels, aiding weight loss, and improving some cardiovascular risk factors.
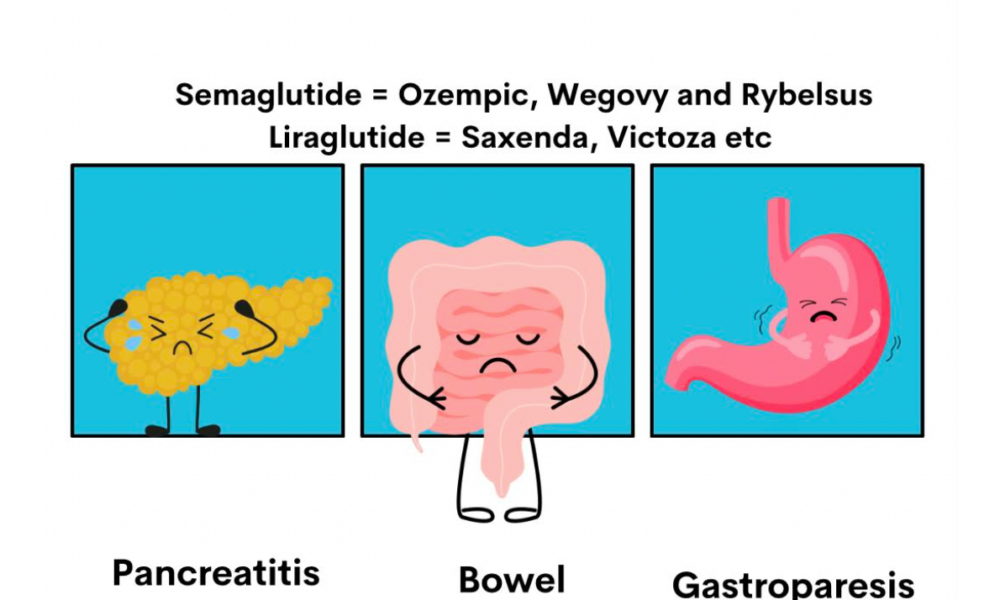
Limitations of Sameglutides:
Despite their effectiveness in the short term, Sameglutides have limitations. They are not a cure for Metabolic Syndrome and may only address specific symptoms. Moreover, they come with potential side effects such as nausea, vomiting, diarrhea, and an increased risk of pancreatitis.
The Role of a Physician-Guided Low-Carb, High-Fat Diet:
A physician-guided low-carb, high-fat diet offers a holistic approach to managing Metabolic Syndrome. By focusing on dietary changes tailored to individual needs, this approach addresses the root causes of the condition. A low-carb, high-fat diet helps regulate blood sugar levels, improve lipid profiles, and promote sustainable weight loss. It also reduces inflammation and supports overall metabolic health.
Comparing Long-Term Outcomes:
When comparing long-term outcomes, a physician-guided low-carb, high-fat diet has several advantages over Sameglutides. While medications may provide immediate relief, they do not address lifestyle factors that contribute to Metabolic Syndrome. In contrast, a personalized dietary approach promotes long-lasting changes in metabolic health, reduces medication reliance, and lowers the risk of complications associated with Metabolic Syndrome.
Conclusion:
Sameglutides like Wagovy and Ozempic can be beneficial in the short term for managing certain aspects of Metabolic Syndrome. However, they are not a substitute for a physician-guided low-carb, high-fat diet. By addressing dietary and lifestyle factors, patients can achieve sustainable improvements in metabolic health and reduce their reliance on medications with potential side effects. Consulting with a healthcare provider for personalized guidance is crucial in developing an effective long-term strategy for managing Metabolic Syndrome.
A Comprehensive Approach to Alleviating Migraines, Anxiety, and Tremors: Integrating Nutritional Psychiatry, a Low-Carb/Carnivore Diet, and Intermittent Fasting
- July 11, 2023
- Stephen Fitzmeyer, MD
- No Comments
Introduction:
Living with migraines, anxiety, and tremors can be challenging, impacting both physical and mental well-being. Fortunately, emerging research suggests that a comprehensive approach combining nutritional psychiatry, a low-carb/carnivore diet, and intermittent fasting may offer relief from these symptoms. In this blog post, we will explore the principles behind this integrative approach and provide practical tips for incorporating it into your lifestyle.
Understanding the Foundations:
Nutritional Psychiatry:
Nutritional psychiatry focuses on the connection between diet and mental health. Consuming nutrient-dense foods rich in antioxidants, omega-3 fatty acids, and essential vitamins and minerals can help reduce inflammation, support neurotransmitter balance, and enhance overall brain health.
Low-Carb/Carnivore Diet:
A low-carb or carnivore diet emphasizes the reduction or elimination of carbohydrates while prioritizing animal-based proteins and healthy fats. By minimizing carbohydrate intake, this diet aims to stabilize blood sugar levels, reduce inflammation, and optimize brain function.
Intermittent Fasting:
Intermittent fasting involves cycling between periods of eating and fasting. This approach promotes metabolic flexibility and may enhance cellular repair mechanisms, reduce inflammation, and support overall well-being. A common approach is to have an eating window during specific hours of the day and fast for the remaining period.
The Integration Process:
Embrace Whole, Nutrient-Dense Foods:
Incorporate a variety of colorful fruits and vegetables, lean proteins, healthy fats, and nuts/seeds into your diet. Prioritize grass-fed meats, wild-caught fish, leafy greens, and low-carb vegetables to provide essential nutrients for brain health.
Eliminate Seed Oils:
Eliminate seed oils such as soybean, sunflower, safflower, and corn oil from your diet. These oils are high in omega-6 fatty acids, which can promote inflammation. Instead, opt for healthier alternatives like olive oil, coconut oil, lard, ghee, beef tallow, and grass-fed butter.
Mindful Meal Planning:
Work with a healthcare professional or registered dietitian to develop a personalized meal plan. Focus on high-quality animal proteins, healthy fats, and non-starchy vegetables. Experiment with delicious recipes that align with your dietary preferences and restrictions.
Implement Intermittent Fasting:
Start with a 12-hour fasting window overnight and gradually increase to 16 or 18 hours, as tolerated. During the eating window, prioritize nutrient-dense meals to ensure adequate nutrition. Stay hydrated with water and herbal tea throughout the fasting period.
Prioritize Sleep and Stress Management:
Adequate sleep and stress management are vital components of overall well-being. Establish a consistent sleep routine and incorporate stress-reducing techniques like mindfulness, meditation, or yoga into your daily routine.
Regular Exercise:
Engage in regular physical activity to support overall health and well-being. Moderate-intensity exercises like aerobic activities and strength training can improve mood, reduce stress, and enhance brain function.
Conclusion:
Taking a comprehensive approach to managing migraines, anxiety, and tremors through nutritional psychiatry, a low-carb/carnivore diet, and intermittent fasting offers a promising strategy for symptom alleviation. However, it’s crucial to remember that individual needs may vary, and it’s essential to consult with a healthcare professional or registered dietitian before making significant dietary changes.
By embracing whole, nutrient-dense foods, eliminating seed oils, and implementing intermittent fasting, you can optimize your brain health and potentially find relief from these debilitating conditions. Prioritize self-care, practice mindful eating, and seek professional guidance to ensure a safe and effective journey towards better health and well-being.
Remember, always consult with your healthcare provider before making any changes to your diet or treatment plan.
References:
Smith R, et al. (2020). The role of nutrition in mental health: Breaking the vicious cycle of poor mental health and unhealthy diets. International Journal of Environmental Research and Public Health, 17(24), 9094. doi: 10.3390/ijerph17249094.
Paoli A, et al. (2019). Beyond weight loss: A review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. European Journal of Clinical Nutrition, 73(3), 324-333. doi: 10.1038/s41430-018-0341-9.
Patterson RE, et al. (2015). Intermittent fasting and human metabolic health. Journal of the Academy of Nutrition and Dietetics, 115(8), 1203-1212. doi: 10.1016/j.jand.2015.02.018.
Exploring the Potential Benefits of MCT Oil for Health and Wellness
- July 4, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
MCT oil, short for medium-chain triglyceride oil, has gained considerable attention in recent years for its potential health benefits. Derived from coconut or palm kernel oil, MCT oil is composed of medium-chain fatty acids that are easily absorbed and rapidly converted into energy by the body. In this article, we will explore the various benefits associated with MCT oil and its potential impact on weight management, energy levels, cognitive function, gut health, nutrient absorption, and certain medical conditions.
Weight Management:
MCT oil has been the subject of studies investigating its role in weight loss and weight management. Due to its unique properties, MCT oil can increase feelings of fullness and potentially reduce calorie intake, aiding in weight management efforts. Incorporating MCT oil into a balanced diet may provide individuals with a sustainable approach to shedding excess pounds.
Energy Boost:
One of the notable advantages of MCT oil is its ability to serve as a quick source of energy. Unlike long-chain fatty acids, which take longer to break down, MCT oil is rapidly converted into energy by the body. This characteristic makes it a favored choice for athletes and individuals engaging in high-intensity workouts, as it can provide an immediate energy boost to fuel performance.
Mental Clarity and Cognitive Function:
The consumption of MCT oil can lead to elevated levels of ketones in the body. Ketones are an alternative energy source for the brain, and they have been associated with improved mental clarity, focus, and cognitive function. This makes MCT oil particularly intriguing for individuals following ketogenic diets or seeking to enhance their mental performance.
Nutrient Absorption:
MCT oil has been found to enhance the absorption of fat-soluble vitamins and minerals. By incorporating MCT oil into meals, the body’s ability to absorb essential nutrients such as vitamin E, vitamin D, calcium, and magnesium may be improved. This can be especially beneficial for individuals with nutrient deficiencies or compromised nutrient absorption.
Gut Health:
The antimicrobial properties of MCT oil have shown potential in promoting a healthy gut microbiome. Research suggests that MCT oil can help reduce harmful bacteria while encouraging the growth of beneficial bacteria in the digestive system. A balanced gut microbiome is crucial for overall gut health, digestion, and immune function.
Increased Ketone Production:
MCT oil is frequently used in ketogenic diets due to its ability to enhance the production of ketones in the body. Ketones are produced when the body breaks down fat for energy and can provide metabolic benefits such as enhanced fat burning. This makes MCT oil a valuable addition to the diet of those aiming to achieve and maintain a state of ketosis.
Management of Certain Medical Conditions:
Emerging research indicates that MCT oil may have a positive impact on certain medical conditions. Studies have explored its potential use in managing epilepsy, Alzheimer’s disease, and autism. While more research is needed to fully understand its effects and appropriate usage, MCT oil shows promise as a potential adjunct therapy for these conditions.
Conclusion:
MCT oil offers a range of potential health benefits, including weight management, increased energy, improved cognitive function, gut health promotion, enhanced nutrient absorption, and potential therapeutic applications in certain medical conditions. However, it is essential to remember that individual responses may vary, and consulting with a healthcare professional before incorporating MCT oil into your routine is advised. Additionally, moderation is key, as excessive consumption of MCT oil may lead to digestive issues or an increase in calorie intake. With the right approach, MCT oil can be a valuable addition to a balanced and healthy lifestyle.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Achieving Stroke Prevention Goals through Medical Management: The Role of a Ketogenic Diet and Intermittent Fasting in Correcting Metabolic Syndrome
- July 3, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Title: The Role of a Ketogenic Diet and Intermittent Fasting in Correcting Metabolic Syndrome and Achieving Stroke Prevention Goals: A Review of Relevant Studies
Introduction:
Metabolic syndrome is a cluster of conditions that increase the risk of developing stroke and other cardiovascular diseases. It is characterized by a combination of dyslipidemia, insulin resistance, hypertension, and obesity. In the quest for effective stroke prevention, medical management plays a crucial role in controlling these risk factors. This article explores how a ketogenic diet and intermittent fasting can be valuable strategies in achieving the goals of medical management by correcting metabolic syndrome.
Dyslipidemia and High-Potency Statin:
Dyslipidemia, characterized by elevated levels of cholesterol and triglycerides, is a significant risk factor for stroke. High-potency statins are widely prescribed to lower cholesterol levels. However, emerging research suggests that a ketogenic diet can positively influence lipid profiles and achieve similar outcomes.
A study published in the Journal of Clinical Lipidology (Feinman et al., 2020) demonstrated that a ketogenic diet led to a significant decrease in total cholesterol, LDL cholesterol, and triglyceride levels, along with an increase in HDL cholesterol. These improvements in lipid profiles could potentially reduce the risk of stroke.
Diabetes and Glycemic Control:
Diabetes is a well-established risk factor for stroke. Maintaining optimal glycemic control is crucial to managing diabetes and reducing the risk of stroke. Traditionally, oral antidiabetic medications and insulin have been used for glycemic control. However, recent evidence suggests that a ketogenic diet and intermittent fasting can be effective complementary approaches.
A study published in Nutrition (Kosinski & Jornayvaz, 2017) demonstrated that a ketogenic diet improved glycemic control in patients with type 2 diabetes. The diet led to a significant reduction in fasting blood glucose levels, hemoglobin A1c, and insulin resistance. Additionally, intermittent fasting has been shown to improve insulin sensitivity and reduce fasting glucose levels (Tinsley et al., 2016). These findings highlight the potential of a ketogenic diet and intermittent fasting in achieving optimal glycemic control and reducing the risk of stroke in diabetic patients.
Hypertension and Blood Pressure Management:
Hypertension is a leading modifiable risk factor for stroke. While traditional management involves strict blood pressure control with medication, adopting a ketogenic diet and incorporating intermittent fasting may offer additional benefits.
A study published in the British Journal of Nutrition (Gomez-Arbelaez et al., 2017) found that a ketogenic Mediterranean diet led to a significant reduction in blood pressure levels. The diet was rich in healthy fats, vegetables, and lean protein sources. Similarly, intermittent fasting has been shown to improve blood pressure control in individuals with hypertension (Carter et al., 2018). These findings suggest that a ketogenic diet and intermittent fasting can complement traditional management strategies in achieving optimal blood pressure control and reducing stroke risk.
Smoking Cessation and Lifestyle Modification:
Smoking is a well-established risk factor for stroke. While medical management involves smoking cessation counseling, adopting a ketogenic diet and intermittent fasting can promote overall lifestyle modification, making it easier to quit smoking.
Although studies specifically investigating the effect of a ketogenic diet and intermittent fasting on smoking cessation are limited, these interventions have shown promise in promoting healthy habits and reducing cravings associated with addiction (Pinto et al., 2018). By incorporating these strategies into a comprehensive lifestyle modification plan, individuals can enhance their ability to quit smoking and reduce their stroke risk.
Navigating Vitamin K-Rich Foods for Post-Stroke Patients on Keto and Intermittent Fasting
Following a stroke, effective management plays a crucial role in promoting recovery and reducing the risk of future events. In recent years, the ketogenic diet and intermittent fasting have gained attention for their potential benefits in post-stroke care. However, for individuals on these dietary approaches, there may be concerns about consuming foods rich in vitamin K, which can interact with anticoagulant medications. In this article, we’ll explore the considerations regarding vitamin K intake for post-stroke patients following a ketogenic diet or practicing intermittent fasting.
Understanding Vitamin K and Anticoagulation:
Vitamin K is an essential nutrient involved in blood clotting. Anticoagulant medications, such as warfarin, work by inhibiting the action of vitamin K, reducing the risk of blood clots. Maintaining consistent anticoagulation levels is crucial to minimize the risk of stroke recurrence and other complications.
Ketogenic Diet and Intermittent Fasting:
The ketogenic diet is a low-carbohydrate, high-fat diet that has been studied for its potential benefits in neurologic conditions, including stroke recovery. Intermittent fasting, on the other hand, involves cycling between periods of eating and fasting. While both approaches have shown promise in stroke management, it’s essential to consider their potential impact on vitamin K intake.
Vitamin K-Rich Foods and Consistency:
Foods rich in vitamin K, such as leafy green vegetables, cruciferous vegetables, herbs, and certain oils, are generally considered nutritious and beneficial for overall health. However, for individuals on anticoagulant therapy, sudden or significant changes in vitamin K intake can affect the effectiveness of the medication.
Finding Balance:
Post-stroke patients following a ketogenic diet or practicing intermittent fasting can still include vitamin K-rich foods in their meal plans. The key is to maintain consistency in vitamin K intake from week to week to ensure stable anticoagulation levels.
Collaboration with Healthcare Providers:
Post-stroke patients should collaborate closely with their healthcare providers, including physicians and registered dietitians, to develop a personalized dietary plan that considers their individual needs, medication regimen, and dietary preferences. Healthcare providers can provide guidance on the consumption of vitamin K-rich foods while ensuring that anticoagulation levels remain within the target range.
Post-stroke patients following a ketogenic diet or practicing intermittent fasting can still enjoy the benefits of vitamin K-rich foods while managing their anticoagulation therapy. The key is to maintain consistency in vitamin K intake and work closely with healthcare providers to optimize stroke management. By striking the right balance, individuals can promote their recovery, reduce the risk of stroke recurrence, and achieve their health goals.
Remember, always consult with your healthcare provider or a registered dietitian to receive personalized advice based on your specific condition and medication regimen. Together, you can develop a comprehensive plan that supports your stroke recovery journey while effectively managing your diet and anticoagulation therapy.
Conclusion:
Medical management plays a crucial role in stroke prevention by controlling risk factors associated with metabolic syndrome. However, emerging evidence suggests that a ketogenic diet and intermittent fasting can be valuable additions to traditional management approaches. These lifestyle interventions have been shown to positively impact dyslipidemia, glycemic control, blood pressure management, and overall lifestyle modification, all of which are essential components of medical management in stroke prevention.
By adopting a ketogenic diet, individuals can experience improvements in lipid profiles, including reductions in total cholesterol, LDL cholesterol, and triglycerides, while increasing HDL cholesterol. Moreover, a ketogenic diet has demonstrated effectiveness in improving glycemic control, reducing fasting blood glucose levels, hemoglobin A1c, and insulin resistance in individuals with diabetes. Intermittent fasting, on the other hand, has shown promise in enhancing insulin sensitivity and lowering fasting glucose levels.
Both a ketogenic diet and intermittent fasting have exhibited potential benefits in managing hypertension, leading to reduced blood pressure levels. These interventions promote healthy eating patterns and weight loss, contributing to better overall cardiovascular health.
Additionally, incorporating a ketogenic diet and intermittent fasting into a comprehensive lifestyle modification plan can support smoking cessation efforts. While more research is needed to establish a direct link between these interventions and smoking cessation, they can enhance overall well-being, reduce cravings, and improve self-control, thus facilitating the process of quitting smoking.
Although further studies are warranted to fully elucidate the mechanisms and long-term effects of a ketogenic diet and intermittent fasting in stroke prevention, the available evidence highlights their potential as valuable tools for correcting metabolic syndrome and achieving the goals of medical management. These lifestyle interventions offer a holistic approach to risk factor control and can serve as effective complements to pharmacological therapies in reducing the risk of stroke.
In conclusion, a ketogenic diet and intermittent fasting show promise in correcting metabolic syndrome and addressing the risk factors associated with stroke. Incorporating these lifestyle interventions into medical management strategies can improve dyslipidemia, glycemic control, blood pressure management, and overall health, ultimately reducing the risk of stroke and promoting better long-term outcomes. However, it is important to consult with healthcare professionals before making any significant dietary or fasting changes, as individualized guidance and monitoring are essential for optimal results.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Why Your Doctor Should Start Paying Attention to Your Uric Acid Levels
- July 1, 2023
- Stephen Fitzmeyer, MD
- No Comments
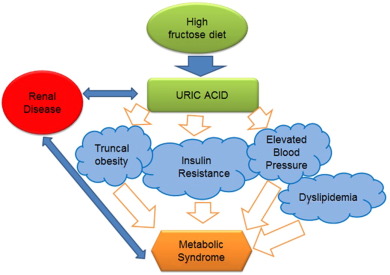
Uric acid, a natural waste product created during the breakdown of purines in the body, has long been associated with a painful condition known as gout. However, recent research has shown that elevated uric acid levels can have broader health implications beyond gout, indicating the importance of monitoring and managing uric acid levels in routine medical care. This article explores the reasons why your doctor should start paying attention to your uric acid levels and how adopting a ketogenic diet can help lower uric acid levels and promote metabolic health.
Gout Prevention and Management: Gout is a form of arthritis characterized by sudden, severe joint pain, swelling, and redness. It occurs when uric acid crystals accumulate in the joints, leading to inflammation. Monitoring uric acid levels can help identify individuals at risk of developing gout and enable early intervention. By proactively managing uric acid levels through lifestyle modifications and medications, doctors can help prevent recurrent gout attacks and minimize joint damage.
Uric Acid as an Independent Risk Factor: Elevated uric acid levels have been linked to various health conditions independent of gout. Research suggests that high uric acid levels may contribute to the development of hypertension, cardiovascular disease, chronic kidney disease, and metabolic syndrome. By monitoring and managing uric acid levels, doctors can potentially identify individuals at increased risk for these conditions and implement preventive measures accordingly.
Kidney Health Assessment: The kidneys play a vital role in filtering and excreting uric acid from the body. Persistently high uric acid levels can strain the kidneys and increase the risk of kidney stones and kidney disease. Monitoring uric acid levels can serve as an indicator of kidney function and help doctors assess overall kidney health. Identifying and addressing elevated uric acid levels can potentially slow down the progression of kidney disease and reduce the risk of related complications.
Uncovering Underlying Health Conditions: High uric acid levels may indicate an underlying health condition such as metabolic disorders, insulin resistance, or certain types of cancer. Identifying and treating these conditions in their early stages can significantly improve outcomes. Regular monitoring of uric acid levels can provide doctors with a valuable diagnostic clue, prompting further investigations and ensuring timely intervention.
Lifestyle Modification and Patient Education: Monitoring uric acid levels can empower doctors to educate their patients about lifestyle modifications that can help maintain healthy levels. By discussing dietary choices, weight management, alcohol consumption, and the importance of staying hydrated, doctors can assist individuals in making informed decisions and adopting healthier habits to control uric acid levels.
Ketogenic Diet and Uric Acid Levels: Recent studies have indicated that adopting a ketogenic diet, which is low in carbohydrates and high in healthy fats, can contribute to lowering uric acid levels and improving metabolic health. The ketogenic diet promotes weight loss, reduces insulin resistance, and enhances the body’s ability to burn fat for fuel. These metabolic changes can lead to a decrease in uric acid production and improved uric acid clearance from the body.
By recommending a ketogenic diet to patients with elevated uric acid levels, doctors can potentially help them achieve metabolic health and reduce the risk of developing gout, hypertension, cardiovascular disease, and other metabolic disorders. However, it’s important to note that dietary changes should be tailored to individual needs and medical history, and consultation with a healthcare professional is crucial before starting any new dietary regimen.
In conclusion, monitoring uric acid levels goes beyond the management of gout. With growing evidence linking elevated uric acid levels to various health conditions, it is essential for doctors to pay attention to their patients’ uric acid levels during routine medical care. By doing so, doctors can prevent and manage gout, identify individuals at risk for other health conditions,
assess kidney health, uncover underlying medical issues, and promote overall metabolic health. Adopting a ketogenic diet, in conjunction with regular monitoring of uric acid levels, can be a valuable tool in achieving these goals.
It is important to emphasize that any dietary changes, including the adoption of a ketogenic diet, should be done under the guidance of a healthcare professional. They can assess the individual’s medical history, evaluate potential risks and benefits, and provide personalized recommendations. Additionally, it’s crucial to consider the overall nutritional balance and adequacy of the diet to ensure that all essential nutrients are obtained.
In summary, by recognizing the broader health implications of elevated uric acid levels and monitoring them regularly, doctors can play a crucial role in preventing and managing gout, identifying underlying health conditions, and promoting optimal metabolic health. Alongside other lifestyle modifications, such as dietary changes, adopting a ketogenic diet can be a valuable approach to lower uric acid levels and improve overall health outcomes. Working in partnership with a healthcare professional, individuals can take proactive steps toward achieving better health and well-being.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unlocking the Power of Fat: Understanding Brown Fat, White Fat, and Ketones in Metabolism
- June 30, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
The human body is a complex machine that relies on various mechanisms to maintain energy balance and regulate metabolism. In recent years, significant research has been conducted to understand the different types of fat and their roles in energy storage, thermogenesis, and overall metabolic health. Additionally, the impact of ketones, particularly beta-hydroxybutyrate (BHB), on uncoupling and thermogenesis in white fat has emerged as a fascinating area of study. This article aims to delve into the fascinating world of brown fat, white fat, and the influence of ketones on fat metabolism.
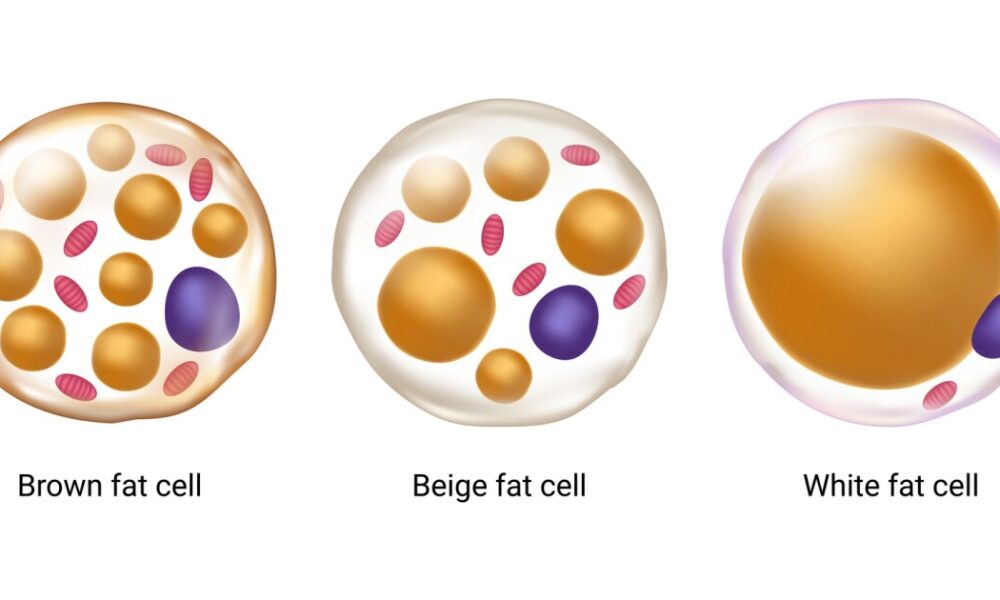
Brown Fat: The Furnace of Heat Generation
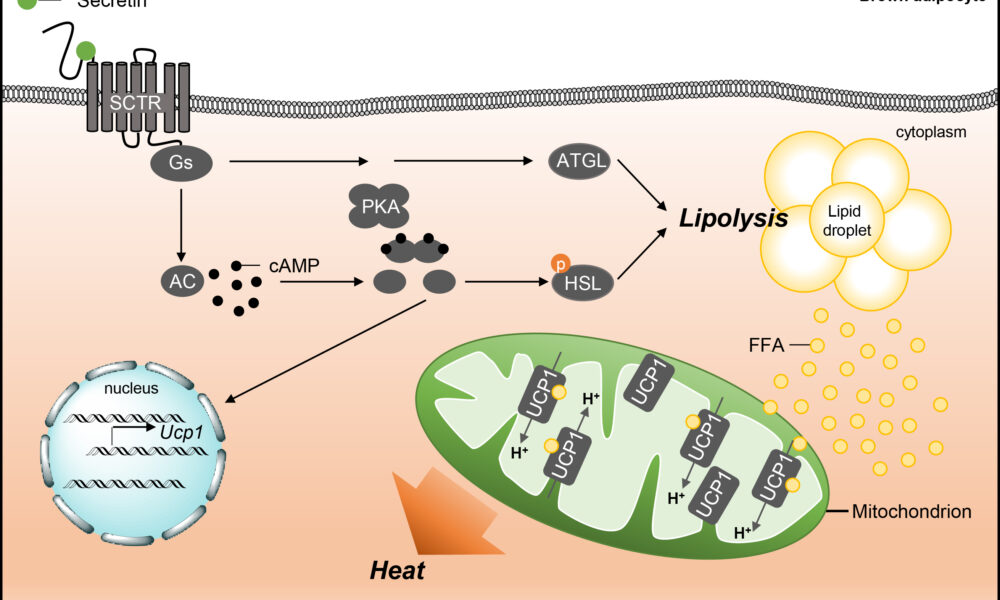
Brown fat, also known as brown adipose tissue (BAT), is a specialized form of fat that plays a crucial role in thermogenesis. Unlike white fat, which primarily stores energy, brown fat is densely populated with mitochondria that contain a unique protein called uncoupling protein 1 (UCP1). UCP1 enables the uncoupling of electron transport and ATP synthesis, diverting energy towards heat production. By activating brown fat, the body can generate heat and maintain body temperature, making it an important component in combating hypothermia and regulating energy expenditure.
White Fat: Beyond Energy Storage
White fat, or white adipose tissue (WAT), is the more abundant type of fat in the human body and is primarily associated with energy storage. White fat cells store excess energy in the form of triglycerides, which can be released when energy is needed. However, recent research has shown that white fat can exhibit properties similar to brown fat through a process called browning or beiging. Browning involves the activation of UCP1 in white fat cells, leading to increased thermogenesis and energy expenditure. This discovery has opened up new possibilities for harnessing the potential of white fat in weight management and metabolic health.
Ketones: Fueling the Metabolic Fire
Ketones, specifically beta-hydroxybutyrate (BHB), have garnered attention for their impact on fat metabolism and uncoupling in white fat. During periods of low carbohydrate availability, such as fasting or adherence to a ketogenic diet, the body produces ketones as an alternative fuel source. Ketones can enhance uncoupling in white fat by increasing UCP1 expression, improving mitochondrial function, and activating specific signaling pathways. This process promotes thermogenesis and energy expenditure in white fat cells, potentially contributing to weight loss and metabolic health benefits associated with ketogenic diets.
Metabolic Flexibility and Health Implications
Understanding the intricate interplay between brown fat, white fat, and ketones provides insights into metabolic flexibility and its impact on health. Activating brown fat and promoting browning of white fat can increase energy expenditure, potentially assisting in weight management and combating obesity. Additionally, the utilization of ketones as an alternative fuel source offers metabolic advantages, such as improved mitochondrial function and uncoupling in white fat, which may have implications for metabolic health and conditions such as diabetes and cardiovascular disease.
Conclusion:
The exploration of brown fat, white fat, and the influence of ketones on fat metabolism has unveiled exciting possibilities for understanding energy balance, thermogenesis, and metabolic health. The ability to activate brown fat, induce browning of white fat, and harness the power of ketones could provide new avenues for managing weight, improving metabolic health, and combating metabolic disorders. As research in this field continues to evolve, we are gaining a deeper understanding of the intricate mechanisms that govern our metabolism and pave the way for innovative strategies in promoting a healthier future.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Mitochondrial Metabolism: An Essential Regulator of Adipose Tissue, Metabolic Health, Inflammation, and Brain Function
- June 25, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Mitochondria, often referred to as the powerhouses of the cell, play a crucial role in various aspects of human physiology. Beyond their well-known role in energy production, emerging research has shed light on the intricate relationship between mitochondrial metabolism and adipose tissue development and function. Moreover, recent discoveries have highlighted the impact of mitochondrial metabolism on metabolic health, inflammation, and even brain function. Understanding these connections could pave the way for new therapeutic strategies in tackling obesity, metabolic disorders, and neurodegenerative diseases.
Adipose tissue, commonly known as fat, was once perceived as an inert energy storage depot. However, it is now recognized as a dynamic and metabolically active organ that influences whole-body homeostasis. Adipose tissue consists of two main types: white adipose tissue (WAT) and brown adipose tissue (BAT). WAT primarily stores energy in the form of triglycerides, while BAT dissipates energy through thermogenesis. Both types of adipose tissue are influenced by mitochondrial metabolism, albeit in different ways.
In WAT, mitochondrial metabolism has been found to regulate adipogenesis, the process by which precursor cells differentiate into mature adipocytes. Studies have shown that impaired mitochondrial function leads to dysfunctional adipocyte differentiation and altered adipose tissue development. Furthermore, mitochondrial dysfunction in WAT has been linked to insulin resistance, a hallmark of metabolic disorders such as obesity and type 2 diabetes.
On the other hand, BAT is enriched with mitochondria and possesses a high capacity for oxidative metabolism. Brown adipocytes express a protein called uncoupling protein 1 (UCP1), which uncouples oxidative phosphorylation from ATP synthesis, resulting in the generation of heat. This unique characteristic of BAT is essential for maintaining body temperature and regulating energy expenditure. Emerging evidence suggests that impaired mitochondrial metabolism in BAT contributes to obesity and metabolic dysfunction. Conversely, enhancing mitochondrial function in BAT has been proposed as a potential therapeutic strategy to combat obesity and associated metabolic disorders.
Mitochondrial metabolism not only influences adipose tissue development and function but also plays a pivotal role in metabolic health and inflammation. Dysfunctional mitochondria can lead to an imbalance in cellular energy metabolism, resulting in the accumulation of toxic metabolites and the generation of reactive oxygen species (ROS). Excessive ROS production contributes to oxidative stress and chronic low-grade inflammation, which are closely associated with obesity, insulin resistance, and cardiovascular diseases. Inflammation disrupts normal adipose tissue function and can further exacerbate metabolic dysfunction.
Furthermore, recent studies have highlighted the impact of mitochondrial metabolism on brain health and function. The brain is a highly energy-demanding organ, and mitochondrial dysfunction has been implicated in various neurodegenerative disorders, including Alzheimer’s and Parkinson’s diseases. Impaired mitochondrial function in the brain can lead to reduced energy production, compromised neuronal activity, and increased vulnerability to oxidative stress and inflammation. Therefore, maintaining mitochondrial health in the brain is crucial for preserving cognitive function and preventing neurodegeneration.
The intricate interplay between mitochondrial metabolism, adipose tissue development, metabolic health, inflammation, and brain function underscores the importance of understanding these relationships in a holistic manner. Targeting mitochondrial dysfunction may hold promise for therapeutic interventions aimed at improving metabolic health, combating obesity, and even mitigating neurodegenerative diseases.
In conclusion, mitochondrial metabolism is a key regulator of adipose tissue development and function. It influences both white and brown adipose tissues, impacting metabolic health, inflammation, and even brain function. Exploring the molecular mechanisms underlying these connections could provide valuable insights into the pathogenesis of obesity, metabolic disorders, and neurodegenerative diseases. Ultimately, this knowledge may open doors to novel therapeutic strategies that target mitochondrial function, empowering individuals to take control of their metabolic well-being and combat the growing burden of obesity and associated diseases. By promoting mitochondrial health and optimizing adipose tissue function, we may pave the way for a healthier future.
It is evident that mitochondria play a multifaceted role in our bodies, extending far beyond their traditional association with energy production. Their influence on adipose tissue development and function, metabolic health, inflammation, and brain function highlights their significance in maintaining overall physiological balance.
As researchers continue to delve into the intricate mechanisms that govern mitochondrial metabolism, new therapeutic avenues may emerge. Targeted interventions aimed at enhancing mitochondrial function could potentially revolutionize the treatment of metabolic disorders, including obesity, insulin resistance, and neurodegenerative diseases.
Moreover, advancements in our understanding of mitochondrial metabolism may lead to the identification of novel biomarkers for early detection and risk assessment of these conditions. This could enable personalized interventions and interventions at an earlier stage, with the potential to halt or reverse disease progression.
However, it is important to acknowledge that the complexities of mitochondrial metabolism and its interactions with various bodily systems require further investigation. Ongoing research is needed to unravel the underlying mechanisms and to validate the potential therapeutic strategies that target mitochondrial function.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Exonerating Salt: Metabolic Syndrome Unveiled as the Underlying Culprit of Hypertension
- June 24, 2023
- Dr. Stephen Fitzmeyer, Dr. Sharon Lojun
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
Hypertension, commonly known as high blood pressure, has long been associated with excessive salt intake. However, emerging research challenges this widely accepted belief, suggesting that hypertension is primarily a result of metabolic syndrome rather than a direct consequence of salt consumption. Metabolic syndrome, characterized by a cluster of metabolic abnormalities, including obesity, insulin resistance, and dyslipidemia, plays a pivotal role in salt retention and the development of hypertension. In this article, we will explore the misconceptions surrounding the salt hypothesis and delve into the intricate connection between metabolic syndrome and hypertension.
The Salt Paradox:
For decades, medical professionals and public health campaigns have emphasized reducing salt intake as a means to prevent and manage hypertension. However, the relationship between salt consumption and hypertension is not as straightforward as once believed. Numerous studies have failed to establish a consistent link between salt intake and blood pressure elevation. Furthermore, populations consuming low-salt diets have not demonstrated significant reductions in hypertension rates. This paradox raises questions about the true nature of the relationship between salt and hypertension.
Metabolic Syndrome: The Underlying Culprit:
Metabolic syndrome, a cluster of interconnected metabolic abnormalities, is now recognized as a significant contributor to hypertension. Obesity, insulin resistance, dyslipidemia, and chronic inflammation characteristic of metabolic syndrome disrupt the body’s delicate balance, leading to salt retention and the subsequent rise in blood pressure. Insulin resistance, a hallmark of metabolic syndrome, impairs sodium excretion by the kidneys, promoting salt retention and fluid accumulation. These metabolic derangements create a vicious cycle, perpetuating hypertension and further exacerbating the effects of salt retention.
Unveiling the Root Causes:
While salt intake may play a minor role in hypertension for a subset of individuals with salt sensitivity, it is crucial to focus on the underlying metabolic dysfunctions. Ultra-processed carbohydrates and fats, prevalent in modern diets, have been identified as primary culprits in the development of metabolic syndrome. These refined and heavily processed food products contribute to obesity, insulin resistance, and chronic inflammation, creating an environment conducive to hypertension and salt retention.
The Role of Lifestyle Interventions:
In addressing the underlying metabolic dysfunctions associated with hypertension, lifestyle interventions take center stage. A ketogenic diet, characterized by low carbohydrate intake and increased fat consumption, has shown promising results in improving metabolic health and blood pressure control. By shifting the body’s primary fuel source from carbohydrates to fats, a ketogenic diet improves insulin sensitivity, promotes weight loss, and mitigates chronic inflammation, thereby tackling the root causes of hypertension.
Intermittent fasting, an eating pattern that cycles between periods of fasting and feeding, has also demonstrated metabolic benefits. Beyond calorie restriction, intermittent fasting enhances insulin sensitivity, promotes autophagy, and regulates blood pressure, making it a valuable tool in the management of hypertension associated with metabolic syndrome.
Conclusion:
Contrary to the long-standing belief that salt intake is the primary driver of hypertension, the emerging evidence suggests that metabolic syndrome, with its associated metabolic dysfunctions, is the root cause of salt retention and subsequent development of hypertension. While salt sensitivity may play a role in some individuals, it is essential to address the broader metabolic context to effectively manage hypertension. Lifestyle interventions, such as adopting a ketogenic diet and incorporating intermittent fasting, offer promising strategies to reverse metabolic syndrome, improve metabolic health, and alleviate hypertension. By shifting the focus from salt intake to metabolic health, we can reframe our approach to hypertension management and pave the way for more effective prevention and treatment strategies.
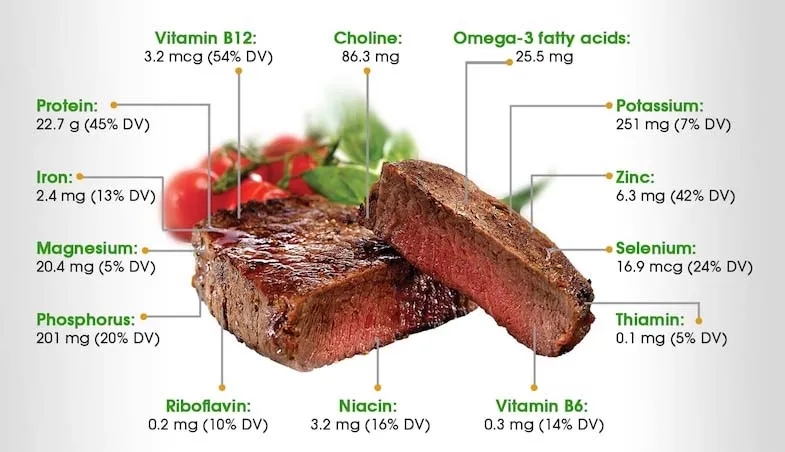
The Nutritional Powerhouse: Why Steak Triumphs Over Kale, Fruits, and Vegetables for Keto
- June 23, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
Following a ketogenic diet requires careful consideration of the perfect meal that meets all your nutritional needs. While kale, fruits, and vegetables are often lauded for their vitamin and mineral content, it is crucial to recognize the exceptional nutritional value that steak brings to the table. In this article, we will explore how steak, packed with specific vitamins and minerals, surpasses other food options for those adhering to a keto lifestyle.
Vitamin B12:
Steak, especially grass-fed beef, is an exceptional source of vitamin B12, crucial for energy production, brain health, and the formation of red blood cells. A 3-ounce serving of steak provides approximately 158% of the recommended daily intake (RDI) of vitamin B12, while kale, fruits, and vegetables fall short in this aspect.
Choline:
Choline is an essential nutrient important for brain function, liver health, and muscle movement. While kale and certain vegetables contain choline, steak surpasses them significantly. A 3-ounce serving of steak delivers around 32% of the RDI of choline, making it a superior choice for meeting your choline requirements.
Omega-3 Fatty Acids:
Omega-3 fatty acids are crucial for heart health, brain function, and reducing inflammation. While fatty fish like salmon are renowned for their omega-3 content, certain cuts of steak, particularly grass-fed beef, provide a respectable amount. A 3-ounce serving of steak offers approximately 84 milligrams of omega-3 fatty acids, making it a viable option for keto enthusiasts.
Protein:
A cornerstone of the ketogenic diet is consuming an adequate amount of protein while minimizing carbohydrate intake. Steak, with its high protein content, outshines kale, fruits, and vegetables. A 3-ounce serving of steak typically supplies around 22 grams of protein, making it an excellent choice for meeting protein needs.
Iron:
Iron is essential for transporting oxygen throughout the body and preventing anemia. Steak, particularly red meat, is an exceptional source of heme iron, which is more easily absorbed than non-heme iron found in plant-based sources. A 3-ounce serving of steak contains approximately 15% of the RDI of iron, offering a considerable advantage over kale, fruits, and vegetables.
Magnesium, Phosphorus, and Potassium:
Steak provides a notable amount of minerals crucial for various bodily functions. A 3-ounce serving of steak typically supplies around 8% of the RDI of magnesium, 20% of the RDI of phosphorus, and 7% of the RDI of potassium. These percentages surpass what kale, fruits, and vegetables offer in terms of these specific minerals.
Riboflavin, Niacin, B6, and Thiamine:
Steak contains an array of B vitamins necessary for energy production, brain health, and overall well-being. A 3-ounce serving of steak offers approximately 20% of the RDI of riboflavin, 36% of the RDI of niacin, 24% of the RDI of vitamin B6, and 11% of the RDI of thiamine. These percentages highlight the superiority of steak over kale, fruits, and vegetables in terms of these specific B vitamins.
Selenium and Zinc:
Steak is an excellent source of the minerals selenium and zinc, both of which are crucial for immune function and overall health. A 3-ounce serving of steak typically provides around 48% of the RDI of selenium and 36% of the RDI of zinc.
Conclusion:
In conclusion, when it comes to following a ketogenic diet, steak proves to be an exceptional choice that surpasses kale, fruits, and vegetables in terms of specific vitamins and minerals. Packed with vitamin B12, choline, omega-3 fatty acids, protein, iron, magnesium, phosphorus, riboflavin, niacin, B6, thiamine, selenium, zinc, and potassium, steak offers a comprehensive nutritional profile that aligns perfectly with the principles of a keto lifestyle.
By incorporating steak into your keto meal plan, you can ensure an abundant supply of these essential nutrients, supporting energy production, brain function, immune health, and muscle maintenance. The bioavailability of these vitamins and minerals in steak further enhances their utilization by the body, maximizing their benefits.
It is important to note that while fruits and certain vegetables may not be emphasized in a strict ketogenic diet due to their carbohydrate content, it is still essential to include non-starchy vegetables that are low in carbs, such as leafy greens, to ensure an adequate intake of fiber, micronutrients, and antioxidants.
As always, consulting with a healthcare professional or registered dietitian is recommended to personalize your keto diet plan and ensure it meets your individual needs and goals.
With the exceptional nutrient profile of steak, it can be a valuable addition to your ketogenic journey, providing not only delicious flavor but also a wide array of essential vitamins and minerals that support your overall health and well-being while maintaining ketosis.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
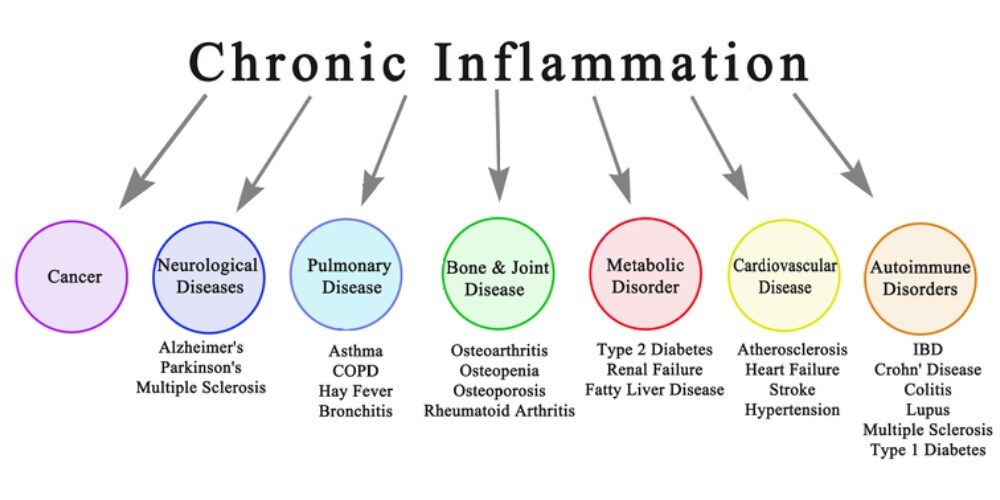
Are You One of the 88% of the the U.S. Adult Population suffering from Chronic Inflammation? Here’s what you should know to find out and fix it.
- June 16, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Introduction: Chronic inflammation is a silent yet powerful contributor to various health problems. It serves as a warning sign of underlying conditions such as metabolic syndrome, poor diet, and other chronic diseases. In this article, we aim to shed light on the detrimental effects of chronic inflammation and emphasize the significance of making positive lifestyle changes to prevent its progression and the onset of related health issues.
Chronic inflammation has been linked to the development of several chronic diseases, including cardiovascular disease, type 2 diabetes, autoimmune disorders, obesity, cancer, neurodegenerative diseases, and respiratory diseases. Understanding the significant impact of chronic inflammation on these chronic diseases highlights the urgency of addressing inflammation through lifestyle modifications.
Part 1: Chronic Inflammation and its Link to Metabolic Syndrome
Chronic inflammation is closely intertwined with metabolic syndrome, a cluster of conditions that includes obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels. This syndrome sets the stage for chronic inflammation, fueling a vicious cycle. As chronic inflammation persists, it further promotes the development of metabolic abnormalities, increasing the risk of cardiovascular disease, type 2 diabetes, and other chronic illnesses.
Part 2: The Role of Diet in Chronic Inflammation
A poor diet plays a significant role in chronic inflammation. Consuming processed foods high in refined carbohydrates, added sugars, unhealthy fats, and artificial additives triggers an inflammatory response within the body. Moreover, the excessive intake of omega-6 fatty acids found in seed oils, commonly used in processed foods, promotes an imbalance in the omega-6 to omega-3 ratio, further exacerbating inflammation. To reduce chronic inflammation, it is important to avoid seed oils such as soybean oil, corn oil, sunflower oil, and cottonseed oil, and instead opt for healthier alternatives like olive oil, avocado oil, and coconut oil.
Part 3: Inflammatory Markers to Assess Chronic Inflammation
If you suspect chronic inflammation, your physician may order specific blood tests to assess inflammatory markers in your body. These markers can provide valuable insights into the presence and extent of inflammation. Common inflammatory markers include:
- C-reactive Protein (CRP): Elevated CRP levels indicate systemic inflammation and can be indicative of various diseases.
- Erythrocyte Sedimentation Rate (ESR): ESR measures the rate at which red blood cells settle in a tube, which can be elevated during inflammation.
- Interleukin-6 (IL-6): IL-6 is a cytokine involved in the inflammatory response, and increased levels may indicate ongoing inflammation.
- Tumor Necrosis Factor-alpha (TNF-α): TNF-α is another cytokine associated with inflammation, and elevated levels are observed in chronic inflammatory conditions.
- Fasting Insulin: Insulin resistance, often associated with chronic inflammation, can be assessed through fasting insulin levels.
Part 4: Taking Control: Lifestyle Changes to Combat Chronic Inflammation
The good news is that chronic inflammation is not entirely beyond our control. By making positive lifestyle changes, we can reduce its impact and mitigate the risks associated with it. Here are some key steps to consider:
- Adopting a Healthy Diet: By adopting a high-fat, low-carb diet rich in healthy fats, adequate protein, and non-starchy vegetables, you can reduce chronic inflammation, enhance your overall well-being, and enjoy a healthier and more vibrant life. Emphasize foods such as fatty fish, grass-fed meats, eggs, nuts, seeds, avocados, olive oil, and non-starchy vegetables. Avoid processed foods, sugary beverages, and seed oils high in omega-6 fatty acids, as they contribute to inflammation.
- Regular Exercise: Engage in regular physical activity to combat obesity, improve insulin sensitivity, and reduce systemic inflammation.
- Stress Management: Chronic stress contributes to inflammation. Incorporate stress management techniques such as meditation, mindfulness, and relaxation exercises into your routine.
Conclusion: Chronic inflammation is a red flag indicating underlying health issues and the potential development of chronic diseases. Metabolic syndrome, poor diet, and other factors contribute to its persistence. By recognizing the role of chronic inflammation in these conditions, we can take proactive steps to address it through lifestyle modifications. Adopting a healthy diet, engaging in regular exercise, managing stress, and avoiding seed oils are crucial in combating chronic inflammation and reducing the risk of associated chronic diseases.
If you suspect chronic inflammation, it is essential to consult with your healthcare provider. They can order specific blood tests to assess inflammatory markers in your body, such as C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and fasting insulin. These tests provide valuable insights into the presence and extent of inflammation, helping your physician develop an appropriate treatment plan.
Don’t wait until chronic inflammation leads to more serious health complications. Take action now to protect your well-being and prevent the development of chronic diseases. Your health is your most valuable asset, and addressing chronic inflammation is a vital step in safeguarding it.
Remember, you are in control of your health. By making conscious choices and adopting a proactive approach, you can reduce chronic inflammation, improve your well-being, and lead a vibrant life. Prioritize your health, make informed choices, and embrace a lifestyle that promotes well-being. Understanding the connection between chronic inflammation, metabolic syndrome, poor diet, and chronic diseases empowers you to break free from this harmful cycle and achieve better health and vitality. Start today and enjoy the long-term benefits of a life free from chronic inflammation. Your body will thank you for it.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Recent Posts
- Jax Code Academy Leads the Revolution: Integrating Generative AI and Prompt Engineering in Coding Bootcamps
- How Coding Bootcamps Help Computer Science Majors Find Jobs Amid Graduation Struggles
- Why Coding Bootcamps Excel Over Traditional College Education
- Unleashing Potential: How Coding Bootcamps Can Transform Your Life
- Sameglutides vs. Physician-Guided Diet for Metabolic Syndrome: A Comprehensive Comparison
Categories
- ApoB
- Artificial Intelligence
- Autophagy
- Biochemistry
- Biomedical Informatics
- Biostatistics
- Blood Glucose
- CAC
- Carbs
- CCD
- CDA
- Clinical Informatics
- Coding Bootcamp
- Coronary Artery Disease
- COVID-19
- Cybersecurity
- Data Science
- Diabetes
- Diet
- EHS
- EMR
- Epidemiology
- Evidence Based Medicine
- Fats
- FHIR
- Fiber
- Generative AI
- Global Health
- Health Administration
- Health Informatics
- Health IT
- HIPAA
- HL7
- Hyperglycemia
- Hypoglycemia
- ICD 10
- Intermittent Fasting
- Ketogenic Diet
- Machine Learning
- Macronutrients
- MCT Oil
- Metabolic Health
- Metabolic Syndrome
- Minerals
- Mitochondria
- MySQL
- Neurology
- Nutritional Ketosis
- Nutritional Neurology
- Nutritional Psychiatry
- PHP
- PHR
- Programming
- Prompt Engineering
- Proteins
- Prototypes
- Public Health
- Python
- Recipes
- Sleep Health
- Stroke
- Uric Acid
- Vegan and Vegetarians
- Vitamin D
- Vitamin K2
- Vitamins