- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Blog
Follow our blog and stay up to date.
Jax Code Academy Leads the Revolution: Integrating Generative AI and Prompt Engineering in Coding Bootcamps
At Jax Code Academy, we’re not just teaching web development; we’re shaping the future of digital innovation. Our revamped curriculum goes beyond the basics, empowering students with the skills to harness the power of generative AI and prompt engineering in building full-stack applications quickly and efficiently. By combining a strong foundation in essential technologies with cutting-edge AI capabilities, our graduates emerge as leaders in the new AI landscape, commanding high salaries and unlocking diverse career opportunities.
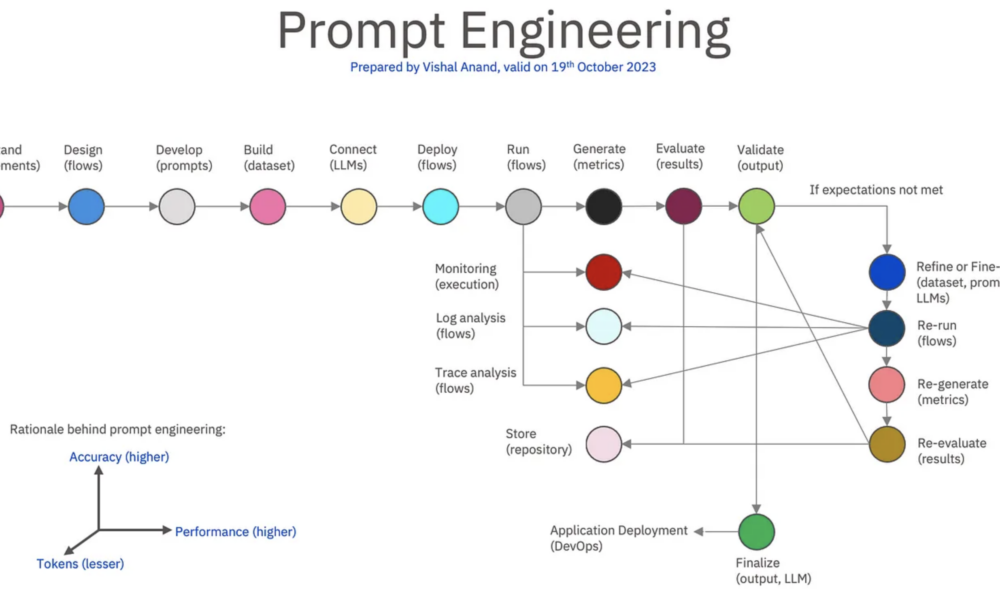
Understanding Generative AI and Prompt Engineering
Generative AI refers to AI models that can generate new content, such as images, text, or code, based on input data and patterns they’ve learned. Prompt engineering involves crafting precise prompts or instructions to steer generative AI models’ outputs towards desired outcomes. Together, these fields enable the creation of AI-powered systems that can produce creative, innovative, and customized content autonomously.
Why Generative AI and Prompt Engineering Are Hot Fields
Creativity Meets Code: Generative AI and prompt engineering blend technical skills with creativity, offering a unique space for individuals who enjoy both coding and artistic expression.
Industry Applications: These fields have applications across industries, from generating art and music to designing websites, writing content, and even developing software code.
Demand for Innovation: Businesses are increasingly leveraging generative AI to automate tasks, personalize user experiences, and drive innovation, creating a high demand for skilled professionals in this space.
Examples of High Salaries
Generative AI Engineers: In tech hubs like Silicon Valley, generative AI engineers with strong coding backgrounds can command salaries ranging from $120,000 to $180,000 per year, depending on experience and expertise.
Prompt Engineering Specialists: Professionals specializing in prompt engineering techniques, such as fine-tuning AI models for specific tasks, can earn between $100,000 to $150,000 annually, with potential for higher earnings in senior roles.
AI Research Scientists: Those leading research and development efforts in generative AI and prompt engineering can fetch salaries exceeding $200,000 per year, especially in top-tier tech companies and research institutions.
Freelance Opportunities: Freelancers and consultants in these fields often charge premium rates, with hourly fees ranging from $100 to $300 or more, depending on project complexity and client requirements.
Building Applications Faster and Leading in the AI Landscape
With a strong foundation in essential technologies and a deep understanding of generative AI and prompt engineering principles, our graduates are equipped to build full-stack applications faster than ever before. They leverage AI-powered tools and frameworks to streamline development workflows, reduce manual coding efforts, and iterate rapidly, ultimately delivering high-quality solutions in record time.
Armed with a comprehensive code base and advanced AI skills, our graduates are poised to lead in the new AI landscape. They understand not just how to code but also how to leverage AI to solve complex problems, drive innovation, and stay ahead of industry trends. Whether it’s developing intelligent chatbots, predictive analytics platforms, or personalized user experiences, our alumni are at the forefront of digital transformation.
The Jax Code Academy Advantage
At Jax Code Academy, we believe in empowering the next generation of tech leaders. Our curriculum is designed to be dynamic, responsive, and future-proof, ensuring that our students are always ahead of the curve. By teaching generative AI and prompt engineering alongside essential web development skills, we’re not just preparing graduates for today’s challenges but also equipping them to thrive in a rapidly evolving tech landscape.
Join us at Jax Code Academy and unlock your potential to innovate, create, and lead in the exciting intersection of web development, generative AI, and prompt engineering. Together, we’ll shape the future of digital experiences, one line of code at a time.
How Coding Bootcamps Help Computer Science Majors Find Jobs Amid Graduation Struggles
In the dynamic landscape of the tech industry, the demand for skilled professionals continues to rise. However, many college graduates with computer science degrees face a common challenge: they possess a strong theoretical foundation but lack practical, hands-on experience crucial for success in the real world. This disconnect between academic knowledge and industry demands can be a significant barrier to securing employment in a competitive job market.
Jax Code Academy’s Impact:
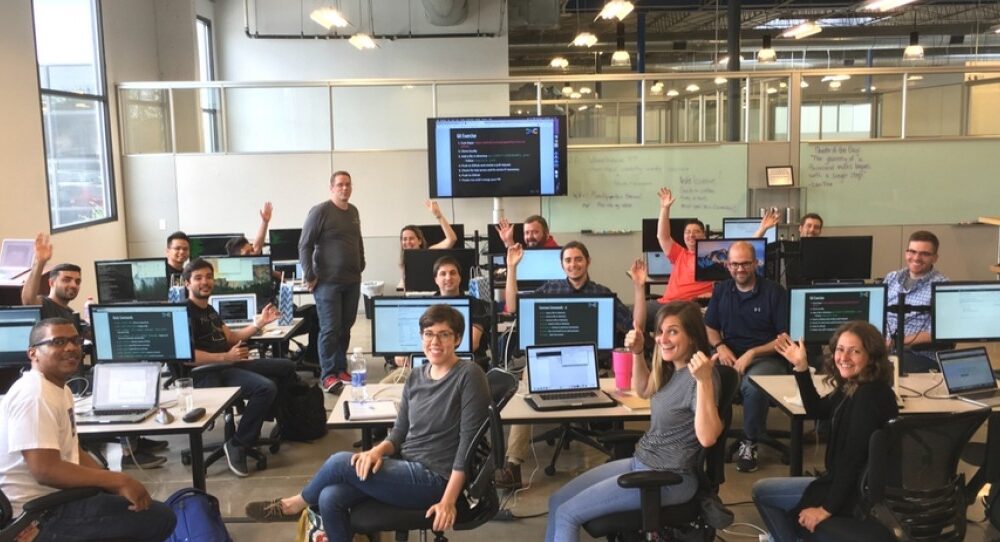
Enter Jax Code Academy in Jacksonville, Florida, a beacon of hope for aspiring tech professionals. This renowned coding bootcamp has revolutionized the way college computer science majors transition into tech careers. The academy’s intensive and industry-aligned curriculum is designed to equip students with the practical skills and project-based experience that employers value most.
Transformational Success Stories:
The success stories emanating from Jax Code Academy are nothing short of inspiring. College computer science majors, once struggling to find jobs due to their lack of practical experience, have transformed into employed tech professionals after completing the academy’s program. These individuals have secured roles in software development, web development, data analysis, and other tech domains, showcasing the effectiveness of practical, skills-focused education.
Confidence and Competence:
The transformation experienced by Jax Code Academy graduates goes beyond acquiring technical skills; it instills confidence and competence. Armed with hands-on experience, problem-solving abilities, and a deep understanding of industry tools and practices, these alumni enter job interviews with a level of preparedness and self-assurance that sets them apart from their peers.
Closing the Skills Gap:
Coding bootcamps like Jax Code Academy play a pivotal role in closing the skills gap in the tech industry. They provide a fast-track route for individuals with theoretical knowledge but limited practical experience to transition into high-demand tech roles. Employers recognize the value of this bridge between education and industry demands, leading to a high job acquisition rate among bootcamp graduates.
Conclusion:
The success stories of college computer science majors finding jobs after attending coding bootcamps like Jax Code Academy highlight the transformative impact of practical, skills-focused education. These experiences showcase how coding bootcamps effectively bridge the gap between academic learning and industry requirements, empowering students to embark on lucrative tech careers with confidence, competence, and a clear pathway to success. Jax Code Academy stands as a testament to the potential of practical education in propelling individuals towards fulfilling and prosperous tech careers, boasting an impressive 100% job placement rate for its graduates.
Why Coding Bootcamps Excel Over Traditional College Education
In today’s fast-paced digital era, the demand for tech talent continues to soar, making coding skills a prized asset in the job market. While traditional college education has its merits, coding bootcamps emerge as a superior choice for those seeking a rapid, cost-effective, and job-focused path to success. Let’s explore why coding bootcamps reign supreme over the expensive and time-consuming route of college education.
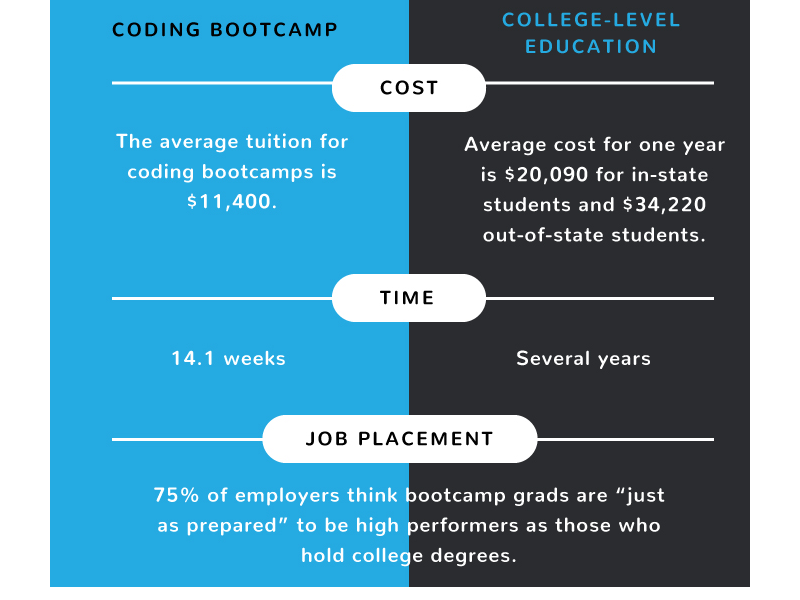
Cost-Effectiveness:
Coding bootcamps offer a budget-friendly alternative to the hefty tuition fees associated with college degrees. With bootcamp costs ranging from $5,000 to $20,000, sometimes even less, students can acquire high-demand tech skills without breaking the bank. In contrast, college tuition fees can skyrocket to tens of thousands of dollars per year, burdening students with significant debt post-graduation.
Time Efficiency:
Time is a precious commodity, and coding bootcamps understand the urgency of getting students job-ready swiftly. Bootcamp programs typically span 3 to 12 months, accelerating the learning curve and allowing graduates to enter the workforce much sooner than their college-educated counterparts. In contrast, a traditional college degree requires a minimum of 4 years, leading to delayed career starts and prolonged financial dependency.
Job Market Readiness:
Coding bootcamps are laser-focused on equipping students with practical, industry-relevant skills that employers crave. From coding languages like Python and JavaScript to project management and software development techniques, bootcamp graduates emerge as ready-to-hire assets. In contrast, college degrees may lack the real-world application and job-specific training demanded by today’s tech employers.
Flexibility and Customization:
Bootcamps offer flexibility in program lengths, formats (online or in-person), and specialization tracks, allowing students to tailor their education to match their career goals and timelines. This customization empowers learners to focus on the skills most relevant to their desired tech roles. On the other hand, college programs often come with rigid curriculum structures and prerequisites, limiting students’ ability to customize their learning experience.
Networking and Career Support:
Many coding bootcamps boast robust networking opportunities and career support services, connecting students with industry professionals, mentors, and job placement assistance. This network-driven approach enhances job placement rates and facilitates seamless transitions into tech careers. While colleges also offer networking resources, the sheer scale and bureaucracy of traditional institutions can sometimes dilute the effectiveness of these connections.
Conclusion:
Coding bootcamps stand as the epitome of efficiency, affordability, and job readiness in today’s competitive job market. By choosing a bootcamp over traditional college education, aspiring tech professionals can fast-track their careers, avoid overwhelming student debt, and embark on a path of success with practical, hands-on skills. In the race for success, coding bootcamps emerge as the clear frontrunner, offering a transformative educational experience that unlocks endless opportunities in the dynamic world of technology.
Unleashing Potential: How Coding Bootcamps Can Transform Your Life
In today’s rapidly evolving digital landscape, coding skills are increasingly becoming a gateway to lucrative and fulfilling careers. One of the most effective ways to acquire these skills is through coding bootcamps, intensive training programs designed to fast-track your journey into the world of programming and technology. Let’s explore how enrolling in a coding bootcamp can be a transformative step towards a better life.
Accelerated Learning: Coding bootcamps are structured to immerse you in a focused learning environment, often for a few months. This intensive approach allows you to absorb knowledge quickly and efficiently, compared to traditional academic programs that may take years to complete. By condensing the learning curve, bootcamps empower you to enter the job market sooner and start earning a competitive salary.
High-Demand Skills: In today’s job market, proficiency in coding languages such as Python, JavaScript, and Java is highly sought after by employers across various industries. By mastering these skills in a coding bootcamp, you position yourself as a valuable asset in fields like software development, web development, data analysis, and more. The demand for tech talent continues to grow, offering abundant job opportunities and career advancement prospects.
Career Flexibility: Coding skills provide a versatile foundation for diverse career paths. Whether you aspire to work for a tech giant, join a startup, freelance as a developer, or explore entrepreneurial ventures, coding proficiency opens doors to a wide range of possibilities. This flexibility empowers you to pursue career avenues that align with your interests, passions, and lifestyle preferences.
Competitive Salaries: Tech roles are known for offering competitive salaries and attractive perks. With the skills acquired from a coding bootcamp, you can command higher compensation packages and enjoy financial stability. Additionally, many tech companies provide opportunities for professional growth, including bonuses, stock options, and benefits that enhance your overall quality of life.
Continuous Learning Culture: Coding bootcamps instill a culture of lifelong learning and adaptation. Technology is constantly evolving, and staying updated with the latest trends and advancements is essential for sustained career success. Bootcamp graduates are equipped with the mindset and resources to embrace continuous learning, upskill as needed, and remain relevant in a dynamic industry.
Networking and Community: Bootcamps often foster a supportive and collaborative learning environment. You interact with peers, instructors, and industry professionals who share your passion for technology. This network not only enhances your learning experience but also opens doors to mentorship, job referrals, and valuable connections that can shape your career trajectory.
Conclusion:
Coding bootcamps represent a transformative opportunity to acquire in-demand skills, unlock career prospects, and embark on a fulfilling professional journey in the tech industry. By investing in your education and embracing the challenges of coding bootcamp, you pave the way for a better life filled with growth, success, and meaningful contributions to the digital world.
Fats: The Primary Fuel Source, with Sugars as a Backup – Supported by Biochemistry
Introduction:
The debate surrounding the optimal fuel source for the human body has garnered significant attention in recent years. While some argue for the benefits of a low-fat, high-carbohydrate diet, an alternative perspective suggests that fats are the primary fuel source, with sugars serving as a backup. In this article, we will present an argument highlighting the advantages of fats as the body’s main energy provider, supported by insights from biochemistry.
- Efficient Energy Release and Sustained Endurance:
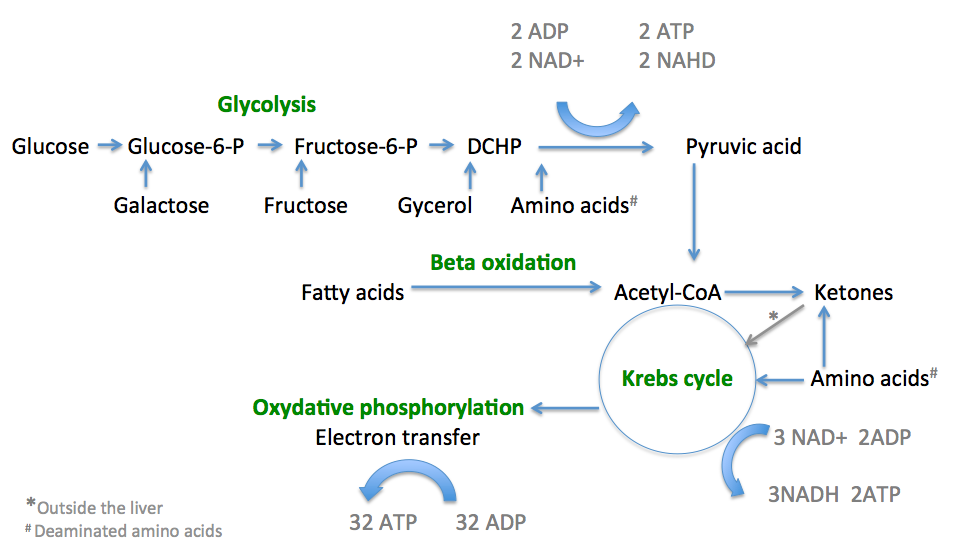
Biochemically, fats offer a highly efficient energy source. When compared to carbohydrates, fats contain a higher number of carbon atoms and more than twice the number of calories per gram. Through a process called beta-oxidation, fatty acids are broken down into acetyl-CoA molecules, which enter the citric acid cycle (also known as the Krebs cycle) to produce energy-rich molecules such as ATP.
This metabolic pathway generates a greater amount of ATP per molecule of fat compared to carbohydrates, providing a sustained and long-lasting energy supply. The slow and steady release of energy from fats is particularly beneficial for endurance activities, allowing individuals to maintain performance over extended periods without relying on frequent carbohydrate consumption.
- Stable Blood Sugar Levels and Reduced Insulin Response:
Biochemically, the consumption of fats has minimal impact on blood sugar levels. In contrast, the rapid breakdown of carbohydrates, especially high-glycemic ones, leads to a surge in blood glucose levels. In response, the pancreas releases insulin to facilitate the uptake of glucose into cells, resulting in a temporary increase in energy levels.
However, the subsequent drop in blood sugar levels can lead to fatigue, cravings, and decreased performance. In contrast, fats provide a more stable and sustained release of energy without triggering significant fluctuations in blood sugar levels or requiring large insulin responses.
- Metabolic Adaptation: Ketosis and Fat Adaptation:
Biochemistry also supports the argument that fats can be the primary fuel source through metabolic adaptations such as ketosis and fat adaptation. When carbohydrate intake is limited, the body initiates ketogenesis, a process in which fatty acids are converted into ketone bodies (e.g., acetoacetate, beta-hydroxybutyrate, acetone).
Ketones can cross the blood-brain barrier and serve as an alternative fuel source for the brain, reducing the need for glucose. This adaptation allows individuals to efficiently utilize fats for energy, leading to increased fat oxidation and a decreased reliance on carbohydrates.
Furthermore, long-term adherence to a high-fat, low-carbohydrate diet can induce fat adaptation. This process involves upregulation of enzymes and transporters involved in fat metabolism, enhancing the body’s ability to derive energy from fats and improving endurance performance.
Conclusion:
The biochemistry of fats strongly supports the argument that they can serve as the primary fuel source for the human body. Fats offer efficient energy release, sustained endurance, stable blood sugar levels, and the potential for metabolic adaptations like ketosis and fat adaptation.
While sugars and carbohydrates still have their place in our diet, considering fats as the primary fuel source, supported by biochemistry, can lead to numerous health benefits. It is essential to understand individual needs, goals, and potential underlying health conditions when determining the optimal macronutrient ratios. Ultimately, a balanced approach that prioritizes healthy fat sources and includes sugars as a secondary fuel source can promote overall well-being and performance.
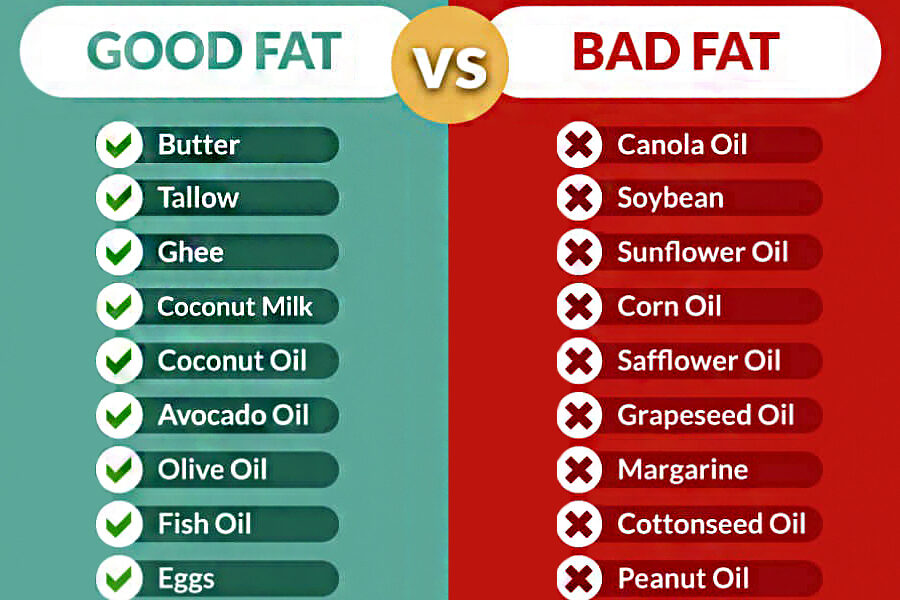
In addition, it is crucial to be aware of the distinction between good fats and bad fats when considering our dietary choices. Good fats, derived from natural sources, provide nourishment and support overall health, while bad fats, commonly found in seed oils, can have negative implications for our well-being.
Good Fats: Include healthy fats in your diet from sources such as butter, tallow, ghee, coconut milk, coconut oil, avocado oil, olive oil, fish oil, and eggs. These fats offer a range of health benefits, including essential nutrients, support for brain function, heart health, and reduced inflammation.
Bad Fats: On the other hand, it is advisable to limit or avoid the consumption of bad fats, particularly seed oils. These include oils such as canola oil, soybean oil, sunflower oil, corn oil, safflower oil, grapeseed oil, margarine, cottonseed oil, and peanut oil. These oils are often highly processed and contain high levels of omega-6 fatty acids, which can promote inflammation and imbalance in the body.
By being mindful of the types of fats we consume, we can make informed choices to support our overall health and well-being. Opt for good fats from natural sources while minimizing the intake of bad fats derived from seed oils. A balanced approach to fat consumption can contribute to an optimized diet and enhance our overall health.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Mitochondria: The Powerhouses that Prefer Fats over Sugars
Introduction:
Mitochondria, the tiny organelles found within our cells, play a crucial role in energy production. They are responsible for converting the food we consume into usable energy in the form of ATP (adenosine triphosphate). While both fats and sugars can serve as fuel sources for our mitochondria, growing evidence suggests that these cellular powerhouses have a preference for utilizing fats as their primary energy substrate. In this article, we will explore the reasons why mitochondria favor fats over sugars for efficient energy production.
- The Efficiency of Fat Oxidation:
Mitochondria exhibit a remarkable efficiency in oxidizing fats compared to sugars. When fatty acids enter the mitochondria, they undergo beta-oxidation, a process that breaks down long-chain fatty acids into smaller units called acetyl-CoA. This acetyl-CoA then enters the citric acid cycle, where it is further metabolized to produce energy-rich molecules such as NADH and FADH2. These molecules are critical for ATP synthesis through oxidative phosphorylation.
The process of fat oxidation generates a greater yield of ATP per molecule compared to the metabolism of sugars. Fats contain more carbon atoms and provide a dense source of energy, supplying a sustained and long-lasting fuel for our cells.
- Mitochondrial Adaptation to Fat Metabolism:
The mitochondria are highly adaptable organelles that can adjust their metabolic machinery based on the available fuel sources. When the body predominantly relies on fats for energy, such as during periods of fasting or a low-carbohydrate diet, mitochondria undergo a process called metabolic flexibility or metabolic switching. This adaptation enables the mitochondria to enhance their capacity to metabolize fats efficiently.
Through increased expression of enzymes and transporters involved in fat metabolism, mitochondria become better equipped to handle fatty acids, ensuring a continuous supply of energy. This adaptation leads to increased mitochondrial biogenesis, the formation of new mitochondria, and improved oxidative capacity, ultimately enhancing fat oxidation as the preferred fuel source.
- Reduced Oxidative Stress and Mitochondrial Health:
Mitochondria have a lower propensity to generate harmful byproducts, such as reactive oxygen species (ROS), during fat oxidation compared to sugar metabolism. When glucose is metabolized, it can result in a higher production of ROS, which can contribute to oxidative stress and damage to cellular components, including mitochondria themselves.
By primarily utilizing fats as a fuel source, mitochondria can reduce the generation of ROS and maintain a healthier environment. This helps to preserve mitochondrial function and integrity, supporting overall cellular health and longevity.
Conclusion:
Mitochondria, the powerhouses of our cells, exhibit a clear preference for utilizing fats over sugars for energy production. The efficiency of fat oxidation, the adaptability of mitochondria to fat metabolism, and the reduced oxidative stress associated with fat utilization all contribute to this preference. By prioritizing fats as a fuel source through dietary choices or strategies like intermittent fasting or a low-carbohydrate diet, we can optimize mitochondrial function and support overall cellular health.
However, it’s important to highlight the remarkable benefits of a ketogenic diet in achieving optimal energy production and overall well-being. While carbohydrates have their role in providing quick bursts of energy and supporting specific bodily functions, a ketogenic diet, which prioritizes fats as the primary fuel source, can have profound effects on our health. By entering a state of ketosis, where the body relies on fat metabolism and produces ketones as an alternative energy source, individuals can experience enhanced fat burning, improved mental clarity, reduced inflammation, and stable energy levels throughout the day. Understanding individual needs and goals can guide the establishment of an optimal macronutrient ratio, allowing individuals to harness the power of ketosis and support their cellular powerhouses in achieving peak performance and well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
- Hoppel, C. (2003). The Role of Carnitine in Normal and Altered Fatty Acid Metabolism. American Journal of Kidney Diseases, 41(4), S4-S12. doi: 10.1016/s0272-6386(03)00003-5
- Kelley, D. E., & Mandarino, L. J. (2000). Fuel Selection in Human Skeletal Muscle in Insulin Resistance: A Replication. Diabetes, 49(5), 677-683. doi: 10.2337/diabetes.49.5.677
- Mootha, V. K., et al. (2003). PGC-1α-responsive Genes Involved in Oxidative Phosphorylation are Coordinately Downregulated in Human Diabetes. Nature Genetics, 34(3), 267-273. doi: 10.1038/ng1180
- Schooneman, M. G., et al. (2013). Fatty Acid Partitioning in the Energetics of the Liver: An Overview and Update. Biochimica et Biophysica Acta (BBA) – Molecular and Cell Biology of Lipids, 1831(12), 169-176. doi: 10.1016/j.bbalip.2013.03.013
- Storlien, L. H., et al. (2004). Adaptation of Muscle Mitochondria to Prolonged Exercise Training. Experimental Physiology, 89(1), 13-22. doi: 10.1113/expphysiol.2003.026203
- Veech, R. L. (2004). The Therapeutic Implications of Ketone Bodies: The Effects of Ketone Bodies in Pathological Conditions: Ketosis, Ketogenic Diet, Redox States, Insulin Resistance, and Mitochondrial Metabolism. Prostaglandins, Leukotrienes and Essential Fatty Acids, 70(3), 309-319. doi: 10.1016/j.plefa.2003.09.007
Unlocking the Power of Health Informatics: Why It Matters
Introduction
Health informatics is a rapidly growing field that combines healthcare, information technology, and data science to transform the way we manage and utilize health-related information. In the digital age, health informatics plays a pivotal role in enhancing patient care, improving healthcare processes, and driving medical research. In this article, we delve into the importance of health informatics and the manifold ways in which it positively impacts the healthcare industry.
Enhanced Patient Care
Health informatics improves patient care by providing healthcare professionals with instant access to accurate and up-to-date patient information. Electronic Health Records (EHRs) store patient histories, test results, medications, and treatment plans, reducing the risk of medical errors and ensuring that the right treatment is delivered to the right patient.
Efficient Healthcare Processes
Health informatics streamlines administrative and clinical processes in healthcare. It reduces paperwork, automates scheduling and billing, and facilitates communication among healthcare providers. This efficiency not only saves time but also reduces costs, making healthcare more accessible.
Data-Driven Decision-Making
Health informatics leverages data analysis to inform healthcare decisions. By analyzing trends and patterns, healthcare providers can make more informed choices about patient care and resource allocation, ultimately improving patient outcomes.
Telemedicine and Remote Monitoring
The integration of health informatics in telemedicine enables remote consultations and monitoring of patients. This is particularly crucial in reaching patients in underserved or remote areas, providing access to quality healthcare that might otherwise be unattainable.
Public Health Surveillance
Health informatics supports public health initiatives by monitoring the spread of diseases and identifying potential outbreaks. Surveillance systems can help health agencies respond swiftly to emerging health threats.
Medical Research and Innovation
Health informatics aids medical research by facilitating access to vast pools of patient data. Researchers can analyze this data to discover new treatments, study disease trends, and develop innovative medical technologies.
Patient Engagement and Empowerment
Health informatics encourages patients to take an active role in their health. Patient portals allow individuals to access their own health records, communicate with healthcare providers, and make informed decisions about their care.
Interoperability and Data Sharing
Standardized data formats and interoperability among healthcare systems enable seamless sharing of patient information across different healthcare providers. This ensures continuity of care and prevents duplication of tests and procedures.
Healthcare Quality Improvement
Health informatics enables healthcare providers to assess and enhance the quality of care they deliver. By tracking outcomes, patient satisfaction, and compliance with best practices, providers can make data-driven improvements.
Cost Reduction and Resource Management
Health informatics helps healthcare institutions optimize resource allocation and reduce costs. By identifying inefficiencies and areas of improvement, healthcare organizations can direct their resources more effectively.
Conclusion
In an era where data is often referred to as the “new oil,” health informatics is the vehicle through which the healthcare industry taps into the vast potential of health-related information. It empowers healthcare professionals with tools and insights to provide more efficient, cost-effective, and patient-centric care. With the ability to save lives, reduce healthcare costs, and drive medical innovations, health informatics is more than a trend; it is the future of healthcare. Its importance continues to grow as technology evolves and as the healthcare industry strives to provide the best possible care to patients around the world.
Pillars of Excellence: Key Standards in the Healthcare Industry
Introduction
The healthcare industry is marked by its unwavering commitment to patient care, safety, and the pursuit of excellence. To maintain the highest standards in patient treatment, healthcare professionals adhere to a set of well-defined guidelines and standards. In this article, we explore the key standards in the healthcare industry that serve as the foundation for quality care and patient safety.
HIPAA (Health Insurance Portability and Accountability Act)
HIPAA, which we discussed in a previous article, is a cornerstone of healthcare standards. Its Privacy and Security Rules ensure the confidentiality, integrity, and availability of protected health information. HIPAA also facilitates secure electronic data exchange, safeguarding patient privacy.
Patient-Centered Care
Patient-centered care focuses on the individual’s needs, preferences, and values. It encourages active patient involvement in healthcare decisions, considering their physical and emotional well-being. Effective communication and shared decision-making are key components of this standard.
Clinical Practice Guidelines
Clinical practice guidelines are evidence-based recommendations for healthcare professionals to provide high-quality care for specific medical conditions. These guidelines are continually updated to reflect the latest research, ensuring that patients receive the best possible care.
Infection Control
Infection control standards are crucial for maintaining patient safety. Healthcare facilities strictly adhere to practices designed to prevent the spread of infections. Hand hygiene, sterilization, and sanitation procedures are key components of infection control.
Accreditation and Certification
Healthcare institutions often seek accreditation and certification from organizations like The Joint Commission, which set high standards for patient care and safety. Compliance with these standards demonstrates an organization’s commitment to quality healthcare delivery.
EHR (Electronic Health Record) Standards
With the transition to electronic health records, interoperability and data standards are essential. These standards ensure that patient information can be accurately and securely exchanged between healthcare systems, promoting continuity of care.
Patient Safety Goals
Organizations like the World Health Organization (WHO) establish patient safety goals that healthcare providers worldwide must strive to meet. These goals include improving medication safety, reducing healthcare-associated infections, and preventing patient falls.
Nursing Standards
Nursing practice is guided by standards set by organizations like the American Nurses Association (ANA). These standards define the responsibilities and expectations for nursing practice, ensuring the delivery of safe and effective care.
Mental Health Standards
Mental health standards ensure that patients with mental health conditions receive appropriate and compassionate care. These standards include the provision of crisis intervention and psychosocial support.
Ethical Standards
Ethical standards in healthcare encompass a wide range of principles, including patient confidentiality, informed consent, and truth-telling. These standards guide the behavior and decision-making of healthcare professionals, ensuring the highest ethical standards in patient care.
Conclusion
The healthcare industry’s commitment to excellence and patient well-being is evident in the multitude of standards and guidelines that govern its practice. These standards touch on various aspects of healthcare, from privacy and data security to patient safety and ethical conduct. Adherence to these standards is not just a requirement but a reflection of the industry’s dedication to providing the best possible care to patients, ensuring their safety, and upholding the highest standards of professionalism and ethics. In the ever-evolving landscape of healthcare, these standards remain the pillars of excellence that drive the industry forward.