- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
- Home
- Warp Core Health
- Blog
- Metabolic Syndrome
Category: Metabolic Syndrome
How AI and Informatics Are Transforming Healthcare
- December 7, 2024
- Stephen Fitzmeyer, MD
- No Comments
In today’s digital age, Artificial Intelligence (AI) is transforming healthcare in ways that were once the stuff of science fiction. From diagnosing diseases to streamlining administrative tasks, AI has become an essential tool in modern medicine. A key player in this transformation is the integration of informatics and advanced AI models like large and small language models. Let’s break down how these innovations are shaping the future of healthcare.
What is Informatics in Healthcare?
Informatics is simply the study of how data is collected, stored, and used to improve healthcare. Think of it as the “brain” behind the systems that organize patient information, track treatments, and ensure smooth communication between doctors, nurses, and patients. It’s the reason your electronic medical records (EMRs) are accessible at the click of a button and why you can get reminders for appointments or medications.
But informatics isn’t just about making life easier for healthcare providers—it’s also about improving patient outcomes. When paired with AI, it becomes a powerful tool for decision-making, helping clinicians make faster and more accurate diagnoses.
Large and Small Language Models: AI That Understands You
Language models are AI systems trained to understand and generate human language. You’ve likely interacted with one already—chatbots, virtual assistants like Siri, or even autocomplete on your phone use this technology.
Large Language Models (LLMs):
These are AI systems trained on vast amounts of text data, making them capable of answering complex questions, summarizing medical records, or even suggesting potential diagnoses. Models like OpenAI’s GPT are examples of LLMs. In healthcare, LLMs can:
- Analyze large sets of data to identify trends.
- Assist doctors by generating patient notes or treatment summaries.
- Translate medical jargon into language patients can easily understand.
Small Language Models:
While they are less complex, small language models are equally important. They are faster, require less computing power, and are easier to deploy in specific applications, such as creating personalized patient reminders or automating appointment scheduling.
How AI and Informatics Work Together in Healthcare
Here’s where the magic happens. By combining the organizational power of informatics with the conversational skills of language models, healthcare systems can:
- Enhance Patient Care: Imagine a system that scans millions of similar cases to recommend the best treatment for your unique condition. AI can do this in seconds, giving doctors valuable insights.
- Reduce Burnout: Administrative tasks often take up much of a healthcare provider’s day. AI-powered tools can handle documentation, freeing up time for patient interaction.
- Improve Accessibility: Language models can provide round-the-clock support through chatbots, answering common medical questions or helping patients book appointments without the need for human intervention.
- Support Early Detection: AI can analyze subtle changes in patient data to flag potential health issues early—whether it’s predicting a heart attack or identifying signs of diabetes from lab results.
A Real-World Example: Telemedicine with AI
Telemedicine has skyrocketed in popularity, especially since the pandemic. By integrating language models, telemedicine platforms can provide instant support. For example:
- A patient enters their symptoms into a virtual chatbot.
- The AI suggests possible conditions and whether they should consult a doctor immediately.
- It then schedules the appointment and provides a summary for the doctor.
The Future of AI in Healthcare
While AI holds tremendous potential, it’s not without challenges. Ensuring patient privacy, addressing biases in AI models, and maintaining the “human touch” in medicine are crucial considerations. However, the collaboration between informatics and AI is already paving the way for a smarter, more efficient, and patient-focused healthcare system.
Conclusion: A Healthier Future with AI
Informatics and AI, powered by large and small language models, are more than buzzwords—they are the tools transforming healthcare. By harnessing their potential, we can improve patient outcomes, reduce provider stress, and make healthcare more accessible to all. Whether it’s a chatbot that answers your late-night health questions or an AI system that helps your doctor diagnose you faster, the future of medicine is here—and it’s powered by technology.
So next time you hear about AI in healthcare, remember: it’s not replacing doctors, but it’s making their work smarter and your care better.
Rethinking Cardiovascular Health: Beyond LDL as a Marker for Disease
- November 12, 2024
- Dr. Stephen Fitzmeyer, Dr. Sharon Lojun
- No Comments
Fellow physicians,
For decades, we’ve relied on LDL as the primary marker for assessing cardiovascular disease (CVD) risk. However, recent research and patient outcomes are prompting us to reconsider this approach. Cardiovascular health is multifaceted, and addressing root causes rather than singular markers like LDL can guide us to better patient outcomes, particularly in our current environment of rising metabolic and liver disease.
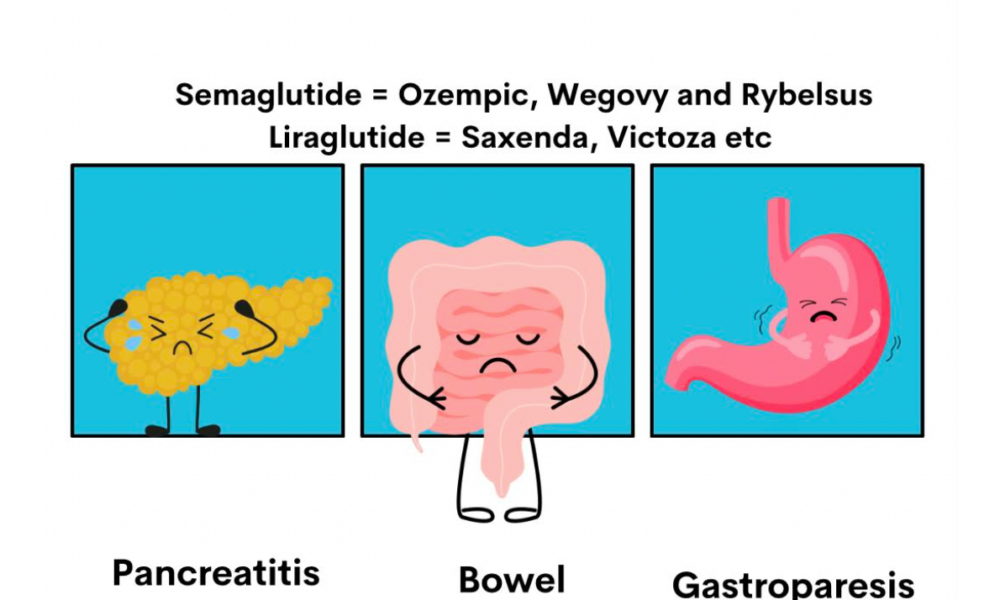
1. GLP-1 Medications: A Bridge, Not a Solution
While medications like Rybelsus (a GLP-1 receptor agonist) offer short-term weight-loss benefits, they come with limitations. Long-term use is costly and can bring side effects such as nausea, diarrhea, and gallbladder issues. Our patients may be drawn to the “quick fix,” but as we know, sustainable health often demands a lifestyle overhaul.
GLP-1s should be viewed as a temporary tool—a way to kick-start weight loss and motivate patients while emphasizing that lifestyle adjustments provide a sustainable path. Ideally, these medications serve as a bridge to instill healthier habits rather than a permanent solution.
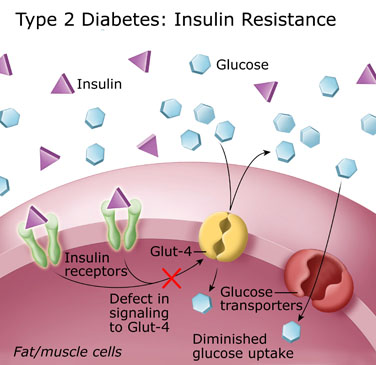
2. The Real Culprit: Insulin Resistance and NAFLD
While elevated LDL is traditionally seen as a red flag for CVD, the underlying issue for many patients is actually insulin resistance. Insulin resistance is at the heart of metabolic syndrome, which drives non-alcoholic fatty liver disease (NAFLD)—a condition increasingly common, even among adolescents.
By focusing on insulin resistance rather than LDL alone, we tackle the metabolic issues that lead to NAFLD. Evidence shows that low-carb diets like keto can reverse fatty liver by lowering triglycerides and reducing liver fat, often leading to improved liver enzyme levels and overall liver health.
3. Better Metrics for Cardiovascular Health: TG/HDL Ratio and LDL Particle Size
Assessing cardiovascular risk requires a broader perspective. Rather than fixating on LDL, consider the triglyceride-to-HDL (TG/HDL) ratio—a stronger indicator of metabolic health. A lower TG/HDL ratio typically correlates with better heart health. Studies have shown that keto and low-carb diets improve this ratio by raising HDL and lowering triglycerides.
Additionally, while LDL levels may not change dramatically on a low-carb diet, LDL particles often shift to a larger, safer size, further reducing cardiovascular risk. These changes are more predictive of positive outcomes than LDL levels alone.
Moving Forward: An Integrated Approach to Patient Health
Incorporating GLP-1s can help patients get started, but it’s lifestyle modifications that will sustain them. Addressing insulin resistance with targeted lifestyle changes like low-carb eating can help reverse NAFLD, improve metabolic health, and reduce the risk of CVD.
Our role is to guide patients not only toward initial success but also to long-term, sustainable health. By shifting the focus from LDL to insulin resistance, we can empower them to achieve better outcomes and transform their health for the future.
Explaining How Glucose and Ketones Become ATP: Why Ketosis and Fat Adaptation Boost Health
- November 9, 2024
- Stephen Fitzmeyer, MD
- No Comments
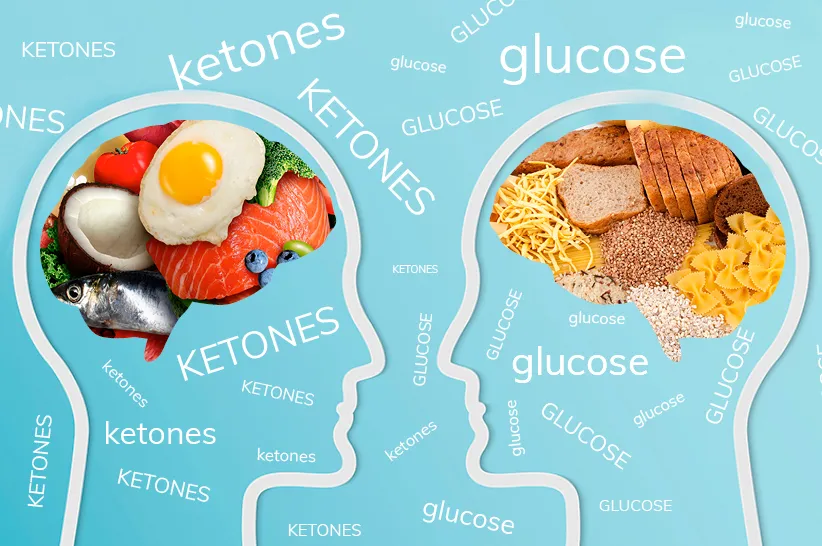
Fuel Sources
When it comes to energy, the body has two primary fuel sources: glucose and ketones. While glucose is often the default source, especially on a typical high-carb diet, ketones become the primary fuel under low-carb or fasting conditions. Ketosis, the metabolic state where the body produces ketones from fat, isn’t just about an alternative fuel source; it also offers several health benefits, including weight loss, improved metabolic health, reduced cardiovascular disease risk, and fat adaptation. Let’s dive into how glucose and ketones each produce ATP and why ketosis is a preferred metabolic state for overall health.
ATP: The Body’s Essential Energy Currency
ATP (adenosine triphosphate) fuels virtually every function in our bodies, from muscle contractions to cognitive activities. The body produces ATP by metabolizing nutrients through complex biochemical pathways, using glucose and ketones as primary fuels. Interestingly, ketones produce more ATP per molecule than glucose, making them an efficient energy source, especially beneficial during ketosis.
Pathway 1: Converting Glucose to ATP
Under normal dietary conditions, glucose is the body’s main energy source. Here’s how glucose becomes ATP through a process called cellular respiration:
Step 1: Glycolysis
- Breakdown of Glucose: In the cytoplasm, glucose is split into two molecules of pyruvate.
- Initial ATP Yield: Glycolysis yields 2 ATP per glucose molecule and produces NADH (an electron carrier for later stages).
Step 2: Pyruvate to Acetyl-CoA
- Conversion in the Mitochondria: Pyruvate enters the mitochondria and is converted to acetyl-CoA, releasing CO₂ and generating more NADH.
Step 3: Citric Acid Cycle (Krebs Cycle)
- Energy Harvesting: Acetyl-CoA enters the citric acid cycle, where it is broken down to produce NADH and FADH₂, which fuel ATP production in the next step.
Step 4: Electron Transport Chain (ETC)
- Main ATP Production: NADH and FADH₂ donate electrons to the ETC, which powers ATP synthase to produce ATP as protons flow back across the mitochondrial membrane.
ATP Yield: Glucose metabolism produces approximately 30-32 ATP per molecule, though it also creates byproducts that can contribute to oxidative stress.
Pathway 2: Converting Ketones to ATP – A More Efficient Pathway
When carbohydrate intake is low, the body shifts to using fat for fuel, producing ketones in the liver. Ketones offer several advantages over glucose, not least of which is their higher energy yield.
Step 1: Ketogenesis in the Liver
- Fat Conversion to Ketones: In the liver, fatty acids are converted into ketones (mainly beta-hydroxybutyrate and acetoacetate) through ketogenesis.
- Transport to Tissues: These ketones are released into the bloodstream and delivered to cells for energy.
Step 2: Ketone Conversion to Acetyl-CoA
- Entry into the Mitochondria: Once inside the cell, ketones are converted back to acetyl-CoA, entering the mitochondria to power the next steps in ATP production.
Step 3: Citric Acid Cycle and Electron Transport Chain
- High ATP Yield: Ketones enter the citric acid cycle, generating NADH and FADH₂, which support the electron transport chain.
Why Ketones Produce More ATP: Ketones, specifically beta-hydroxybutyrate and acetoacetate, produce ATP efficiently but with unique metabolic advantages. When fully oxidized, beta-hydroxybutyrate yields approximately 21.5 ATP per molecule, and acetoacetate provides about 19 ATP, giving a combined total of about 40.5 ATP per pair of ketone molecules. In comparison, one molecule of glucose goes through glycolysis, the citric acid cycle, and the electron transport chain to produce around 30-32 ATP in total. Though glucose produces a comparable amount of ATP, ketones offer metabolic stability, lower oxidative stress, and more efficient energy production in low-carb states, making them an effective and sustainable fuel source, especially during fasting or ketogenic conditions.
Why Ketosis and Fat Adaptation Are Beneficial
The body’s ability to switch from glucose to ketones isn’t just a backup mechanism; it provides significant health benefits. This metabolic flexibility is key for weight loss, metabolic health, and cardiovascular protection. Here’s why ketosis, and the fat adaptation that comes with it, is so advantageous:
- Weight Loss: Ketosis and fat adaptation (when the body becomes efficient at using fat for fuel) are incredibly effective for weight loss. Since the body can tap into stored fat for energy, people in ketosis burn more fat while maintaining stable energy levels. Ketosis also suppresses hunger hormones, making it easier to stick to a calorie deficit.
- Metabolic Syndrome Management: Ketosis helps combat metabolic syndrome by reducing insulin resistance. In ketosis, blood sugar levels are more stable, and the body becomes less reliant on insulin to manage glucose levels. This stability can reverse metabolic syndrome symptoms, which often include high blood pressure, high triglycerides, and abdominal obesity, reducing the risk of type 2 diabetes.
- Reduced Cardiovascular Disease Risk: Ketosis supports cardiovascular health by reducing triglyceride levels and increasing HDL (good) cholesterol. Additionally, ketones produce fewer reactive oxygen species (ROS), meaning less oxidative stress and inflammation, both of which contribute to heart disease. The anti-inflammatory effects of ketosis make it beneficial for long-term cardiovascular protection.
- Fat Adaptation for Enhanced Energy: Fat adaptation is the process where the body becomes efficient at using fat and ketones as its primary energy source. Once fat-adapted, the body can seamlessly access stored fat for sustained energy, which is especially useful for endurance activities and fasting. People who are fat-adapted experience stable energy without the spikes and crashes associated with glucose, making fat adaptation a valuable state for consistent physical and cognitive performance.
- Brain Health and Focus: Ketones readily cross the blood-brain barrier, providing a steady fuel for brain cells. Many people report improved mental clarity, focus, and cognitive endurance in ketosis due to the brain’s ability to efficiently use ketones as fuel, especially when blood sugar levels are low.
Embracing Metabolic Flexibility
By optimizing metabolic pathways to use both glucose and ketones efficiently, the body achieves metabolic flexibility, the ability to switch seamlessly between fuel sources. This flexibility promotes balanced energy levels, reduces cravings, and supports long-term health.
In Summary
- Glucose Pathway: The body breaks down glucose through glycolysis and the citric acid cycle, yielding around 30-32 ATP. However, glucose metabolism can lead to oxidative stress and relies on stable blood sugar levels for consistent energy.
- Ketone Pathway: Ketones are produced in the liver from fatty acids and yield more ATP per molecule than glucose. This efficiency, along with reduced byproducts, makes ketones a cleaner and more sustainable fuel, especially during ketosis and fat adaptation.
Ketosis not only provides a high-yield, steady energy source but also supports fat loss, metabolic syndrome improvement, and cardiovascular health. By fostering metabolic flexibility, ketosis allows the body to switch efficiently between glucose and ketones, supporting optimal energy levels and overall health.
This article emphasizes how ketones provide a cleaner, higher-yielding fuel source that supports fat loss, improved metabolic health, and cardiovascular protection. For those looking to optimize their health, embracing ketosis and fat adaptation offers a powerful way to achieve lasting vitality and metabolic balance.
Sameglutides vs. Physician-Guided Diet for Metabolic Syndrome: A Comprehensive Comparison
- September 4, 2024
- Stephen Fitzmeyer, MD
- No Comments
Introduction:
Metabolic Syndrome is a complex health condition that encompasses a range of risk factors, including obesity, high blood sugar, high blood pressure, and abnormal cholesterol levels. In recent years, medications like Sameglutides, such as Wagovy and Ozempic, have gained popularity for their ability to manage certain aspects of Metabolic Syndrome. However, are these medications a long-term solution, or is there a better approach? Let’s delve into the comparison between Sameglutides and a physician-guided low-carb, high-fat diet for managing Metabolic Syndrome.
Short-Term Benefits of Sameglutides:
Sameglutides like Wagovy and Ozempic belong to a class of medications known as GLP-1 receptor agonists. They work by stimulating insulin production, reducing appetite, and promoting weight loss. These drugs can indeed provide short-term benefits by lowering blood sugar levels, aiding weight loss, and improving some cardiovascular risk factors.
Limitations of Sameglutides:
Despite their effectiveness in the short term, Sameglutides have limitations. They are not a cure for Metabolic Syndrome and may only address specific symptoms. Moreover, they come with potential side effects such as nausea, vomiting, diarrhea, and an increased risk of pancreatitis.
The Role of a Physician-Guided Low-Carb, High-Fat Diet:
A physician-guided low-carb, high-fat diet offers a holistic approach to managing Metabolic Syndrome. By focusing on dietary changes tailored to individual needs, this approach addresses the root causes of the condition. A low-carb, high-fat diet helps regulate blood sugar levels, improve lipid profiles, and promote sustainable weight loss. It also reduces inflammation and supports overall metabolic health.
Comparing Long-Term Outcomes:
When comparing long-term outcomes, a physician-guided low-carb, high-fat diet has several advantages over Sameglutides. While medications may provide immediate relief, they do not address lifestyle factors that contribute to Metabolic Syndrome. In contrast, a personalized dietary approach promotes long-lasting changes in metabolic health, reduces medication reliance, and lowers the risk of complications associated with Metabolic Syndrome.
Conclusion:
Sameglutides like Wagovy and Ozempic can be beneficial in the short term for managing certain aspects of Metabolic Syndrome. However, they are not a substitute for a physician-guided low-carb, high-fat diet. By addressing dietary and lifestyle factors, patients can achieve sustainable improvements in metabolic health and reduce their reliance on medications with potential side effects. Consulting with a healthcare provider for personalized guidance is crucial in developing an effective long-term strategy for managing Metabolic Syndrome.
Achieving Stroke Prevention Goals through Medical Management: The Role of a Ketogenic Diet and Intermittent Fasting in Correcting Metabolic Syndrome
- July 5, 2024
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Title: The Role of a Ketogenic Diet and Intermittent Fasting in Correcting Metabolic Syndrome and Achieving Stroke Prevention Goals: A Review of Relevant Studies
Introduction:
Metabolic syndrome is a cluster of conditions that increase the risk of developing stroke and other cardiovascular diseases. It is characterized by a combination of dyslipidemia, insulin resistance, hypertension, and obesity. In the quest for effective stroke prevention, medical management plays a crucial role in controlling these risk factors. This article explores how a ketogenic diet and intermittent fasting can be valuable strategies in achieving the goals of medical management by correcting metabolic syndrome.
Dyslipidemia and High-Potency Statin:
Dyslipidemia, characterized by elevated levels of cholesterol and triglycerides, is a significant risk factor for stroke. High-potency statins are widely prescribed to lower cholesterol levels. However, emerging research suggests that a ketogenic diet can positively influence lipid profiles and achieve similar outcomes.
A study published in the Journal of Clinical Lipidology (Feinman et al., 2020) demonstrated that a ketogenic diet led to a significant decrease in total cholesterol, LDL cholesterol, and triglyceride levels, along with an increase in HDL cholesterol. These improvements in lipid profiles could potentially reduce the risk of stroke.
Diabetes and Glycemic Control:
Diabetes is a well-established risk factor for stroke. Maintaining optimal glycemic control is crucial to managing diabetes and reducing the risk of stroke. Traditionally, oral antidiabetic medications and insulin have been used for glycemic control. However, recent evidence suggests that a ketogenic diet and intermittent fasting can be effective complementary approaches.
A study published in Nutrition (Kosinski & Jornayvaz, 2017) demonstrated that a ketogenic diet improved glycemic control in patients with type 2 diabetes. The diet led to a significant reduction in fasting blood glucose levels, hemoglobin A1c, and insulin resistance. Additionally, intermittent fasting has been shown to improve insulin sensitivity and reduce fasting glucose levels (Tinsley et al., 2016). These findings highlight the potential of a ketogenic diet and intermittent fasting in achieving optimal glycemic control and reducing the risk of stroke in diabetic patients.
Hypertension and Blood Pressure Management:
Hypertension is a leading modifiable risk factor for stroke. While traditional management involves strict blood pressure control with medication, adopting a ketogenic diet and incorporating intermittent fasting may offer additional benefits.
A study published in the British Journal of Nutrition (Gomez-Arbelaez et al., 2017) found that a ketogenic Mediterranean diet led to a significant reduction in blood pressure levels. The diet was rich in healthy fats, vegetables, and lean protein sources. Similarly, intermittent fasting has been shown to improve blood pressure control in individuals with hypertension (Carter et al., 2018). These findings suggest that a ketogenic diet and intermittent fasting can complement traditional management strategies in achieving optimal blood pressure control and reducing stroke risk.
Smoking Cessation and Lifestyle Modification:
Smoking is a well-established risk factor for stroke. While medical management involves smoking cessation counseling, adopting a ketogenic diet and intermittent fasting can promote overall lifestyle modification, making it easier to quit smoking.
Although studies specifically investigating the effect of a ketogenic diet and intermittent fasting on smoking cessation are limited, these interventions have shown promise in promoting healthy habits and reducing cravings associated with addiction (Pinto et al., 2018). By incorporating these strategies into a comprehensive lifestyle modification plan, individuals can enhance their ability to quit smoking and reduce their stroke risk.
Navigating Vitamin K-Rich Foods for Post-Stroke Patients on Keto and Intermittent Fasting
Following a stroke, effective management plays a crucial role in promoting recovery and reducing the risk of future events. In recent years, the ketogenic diet and intermittent fasting have gained attention for their potential benefits in post-stroke care. However, for individuals on these dietary approaches, there may be concerns about consuming foods rich in vitamin K, which can interact with anticoagulant medications. In this article, we’ll explore the considerations regarding vitamin K intake for post-stroke patients following a ketogenic diet or practicing intermittent fasting.
Understanding Vitamin K and Anticoagulation:
Vitamin K is an essential nutrient involved in blood clotting. Anticoagulant medications, such as warfarin, work by inhibiting the action of vitamin K, reducing the risk of blood clots. Maintaining consistent anticoagulation levels is crucial to minimize the risk of stroke recurrence and other complications.
Ketogenic Diet and Intermittent Fasting:
The ketogenic diet is a low-carbohydrate, high-fat diet that has been studied for its potential benefits in neurologic conditions, including stroke recovery. Intermittent fasting, on the other hand, involves cycling between periods of eating and fasting. While both approaches have shown promise in stroke management, it’s essential to consider their potential impact on vitamin K intake.
Vitamin K-Rich Foods and Consistency:
Foods rich in vitamin K, such as leafy green vegetables, cruciferous vegetables, herbs, and certain oils, are generally considered nutritious and beneficial for overall health. However, for individuals on anticoagulant therapy, sudden or significant changes in vitamin K intake can affect the effectiveness of the medication.
Finding Balance:
Post-stroke patients following a ketogenic diet or practicing intermittent fasting can still include vitamin K-rich foods in their meal plans. The key is to maintain consistency in vitamin K intake from week to week to ensure stable anticoagulation levels.
Collaboration with Healthcare Providers:
Post-stroke patients should collaborate closely with their healthcare providers, including physicians and registered dietitians, to develop a personalized dietary plan that considers their individual needs, medication regimen, and dietary preferences. Healthcare providers can provide guidance on the consumption of vitamin K-rich foods while ensuring that anticoagulation levels remain within the target range.
Post-stroke patients following a ketogenic diet or practicing intermittent fasting can still enjoy the benefits of vitamin K-rich foods while managing their anticoagulation therapy. The key is to maintain consistency in vitamin K intake and work closely with healthcare providers to optimize stroke management. By striking the right balance, individuals can promote their recovery, reduce the risk of stroke recurrence, and achieve their health goals.
Remember, always consult with your healthcare provider or a registered dietitian to receive personalized advice based on your specific condition and medication regimen. Together, you can develop a comprehensive plan that supports your stroke recovery journey while effectively managing your diet and anticoagulation therapy.
Conclusion:
Medical management plays a crucial role in stroke prevention by controlling risk factors associated with metabolic syndrome. However, emerging evidence suggests that a ketogenic diet and intermittent fasting can be valuable additions to traditional management approaches. These lifestyle interventions have been shown to positively impact dyslipidemia, glycemic control, blood pressure management, and overall lifestyle modification, all of which are essential components of medical management in stroke prevention.
By adopting a ketogenic diet, individuals can experience improvements in lipid profiles, including reductions in total cholesterol, LDL cholesterol, and triglycerides, while increasing HDL cholesterol. Moreover, a ketogenic diet has demonstrated effectiveness in improving glycemic control, reducing fasting blood glucose levels, hemoglobin A1c, and insulin resistance in individuals with diabetes. Intermittent fasting, on the other hand, has shown promise in enhancing insulin sensitivity and lowering fasting glucose levels.
Both a ketogenic diet and intermittent fasting have exhibited potential benefits in managing hypertension, leading to reduced blood pressure levels. These interventions promote healthy eating patterns and weight loss, contributing to better overall cardiovascular health.
Additionally, incorporating a ketogenic diet and intermittent fasting into a comprehensive lifestyle modification plan can support smoking cessation efforts. While more research is needed to establish a direct link between these interventions and smoking cessation, they can enhance overall well-being, reduce cravings, and improve self-control, thus facilitating the process of quitting smoking.
Although further studies are warranted to fully elucidate the mechanisms and long-term effects of a ketogenic diet and intermittent fasting in stroke prevention, the available evidence highlights their potential as valuable tools for correcting metabolic syndrome and achieving the goals of medical management. These lifestyle interventions offer a holistic approach to risk factor control and can serve as effective complements to pharmacological therapies in reducing the risk of stroke.
In conclusion, a ketogenic diet and intermittent fasting show promise in correcting metabolic syndrome and addressing the risk factors associated with stroke. Incorporating these lifestyle interventions into medical management strategies can improve dyslipidemia, glycemic control, blood pressure management, and overall health, ultimately reducing the risk of stroke and promoting better long-term outcomes. However, it is important to consult with healthcare professionals before making any significant dietary or fasting changes, as individualized guidance and monitoring are essential for optimal results.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Embracing the Power of Ketogenic Diet and Intermittent Fasting to Fix Metabolic Syndrome: Discovering the Benefits of Fats, Butter, and Bacon
- June 23, 2024
- Stephen Fitzmeyer, MD
- No Comments
Introduction: Metabolic Syndrome has become an alarming health concern worldwide, affecting millions of individuals. The good news is that there are effective strategies to address this condition and restore metabolic health. Two powerful approaches gaining recognition are the ketogenic diet and intermittent fasting (IF). Contrary to conventional beliefs, these methods emphasize the consumption of fats, including sources like butter and bacon. Let’s delve into how this unconventional approach can help fix Metabolic Syndrome and unlock the potential benefits of these often-misunderstood foods.
Understanding Metabolic Syndrome: Metabolic Syndrome refers to a cluster of health conditions, including obesity, high blood pressure, elevated blood sugar levels, abnormal cholesterol levels, and insulin resistance. These factors collectively increase the risk of heart disease, type 2 diabetes, and other chronic ailments. Addressing Metabolic Syndrome is crucial for improving overall health and reducing the risk of long-term complications.
The Power of a Ketogenic Diet: The ketogenic diet, or keto diet for short, is a low-carbohydrate, high-fat dietary approach that encourages the body to enter a state of ketosis. In this metabolic state, the body shifts its primary fuel source from carbohydrates to fats, leading to several benefits:
- Improved Insulin Sensitivity: By limiting carbohydrate intake, the keto diet helps regulate blood sugar levels and enhances insulin sensitivity, addressing one of the core issues of Metabolic Syndrome.
- Weight Loss and Metabolic Flexibility: The ketogenic diet promotes fat loss, especially visceral fat that surrounds vital organs. It also enhances metabolic flexibility, allowing the body to efficiently switch between utilizing carbohydrates and fats for energy.
- Reduced Inflammation: Chronic inflammation is a key driver of Metabolic Syndrome. The keto diet’s emphasis on anti-inflammatory foods can help reduce inflammation markers and improve overall metabolic health.
Harnessing the Power of Intermittent Fasting (IF): Intermittent Fasting, an eating pattern that cycles between fasting and eating windows, complements the ketogenic diet and offers additional benefits:
- Improved Insulin Sensitivity and Blood Sugar Control: Intermittent fasting enhances insulin sensitivity and promotes better blood sugar regulation, further addressing the underlying causes of Metabolic Syndrome.
- Enhanced Fat Burning: Fasting periods allow the body to deplete glycogen stores and tap into fat reserves for energy, promoting effective fat burning and weight loss.
- Autophagy and Cellular Repair: Intermittent fasting triggers autophagy, a natural cellular process that helps remove damaged cells and promote cellular repair and rejuvenation.
Why Fats, Butter, and Bacon Can Be Good for You: Contrary to conventional wisdom, not all fats are created equal. Healthy fats play a crucial role in fixing Metabolic Syndrome and promoting overall well-being:
- Satiety and Long-Lasting Energy: Fats provide a sense of satiety, reducing cravings and preventing overeating. They also offer a steady and long-lasting source of energy.
- Nutrient Absorption: Certain vitamins, such as vitamins A, D, E, and K, are fat-soluble, meaning they require dietary fats for optimal absorption. Including healthy fats like butter and bacon can help ensure proper nutrient utilization.
- Hormone Regulation: Fats are essential for hormone production and balance. They play a crucial role in regulating hormones involved in metabolism, satiety, and overall health.
Conclusion: Metabolic Syndrome can be effectively addressed through a combination of the ketogenic diet and intermittent fasting. Contrary to traditional beliefs, embracing healthy fats, including sources like butter and bacon, can provide essential nutrients, promote satiety, and support metabolic health.
By adopting a ketogenic diet and incorporating intermittent fasting into your lifestyle, you can take significant strides towards fixing Metabolic Syndrome and improving your overall well-being. Remember to prioritize healthy fats like butter and bacon, which provide essential nutrients, support hormone regulation, and contribute to a sense of satiety and long-lasting energy.
However, it’s important to note that before embarking on any dietary changes, it’s advisable to consult with a healthcare professional or registered dietitian. They can provide personalized guidance and ensure that the ketogenic diet and intermittent fasting are suitable for your specific health needs and goals.
By understanding the power of these approaches and reevaluating our perceptions of fats, we can pave the way for better metabolic health, reduced risk of chronic diseases, and a more fulfilling and energized life. So, embrace the transformative potential of the ketogenic diet and intermittent fasting, and unlock the benefits of fats, butter, and bacon for a healthier future.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
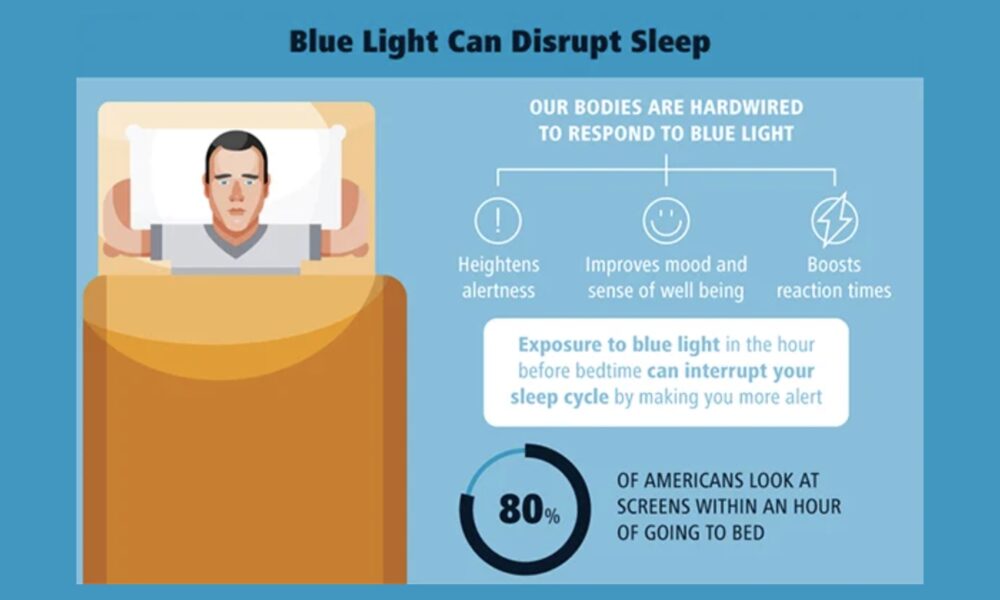
Reducing Blue Light Exposure: Effective Strategies for a Restful Night’s Sleep
- May 30, 2024
- Sharon Lojun, M.D., M.S.
- No Comments
In today’s digital era, our constant exposure to screens emitting blue light has raised concerns about its potential impact on sleep quality. Fortunately, there are several practical solutions available to minimize blue light exposure and promote a more restful night’s sleep. In this article, we will explore various strategies supported by research to help you reduce blue light exposure.
- Device Settings and Filters: Many electronic devices offer settings that allow you to reduce the amount of blue light emitted. By adjusting the display settings on your smartphone, tablet, or computer, you can decrease the intensity of blue light. Some devices even provide a “night mode” or “blue light filter” option, which can automatically adjust the color temperature of the screen to reduce blue light emission. Additionally, you can consider installing external screen filters or privacy screens that block or filter out blue light, providing an extra layer of protection.
- Blue Light Blocking Glasses: Blue light blocking glasses have gained popularity as a convenient solution to minimize blue light exposure. These glasses are designed to filter out or block a significant portion of blue light wavelengths, reducing its impact on your eyes and sleep patterns. Wearing blue light blocking glasses, especially in the evening hours when exposure to screens is common, can help mitigate the disruptive effects of blue light on your circadian rhythm. Clip-on versions, like the one you mentioned, offer a practical and versatile option for those who don’t want to give up screen time entirely.
- Environmental Modifications: Making changes to your sleep environment can also help reduce blue light exposure. Consider investing in blackout curtains or shades that effectively block external sources of light, including streetlights or ambient light pollution. By creating a dark and sleep-conducive atmosphere in your bedroom, you can minimize unnecessary exposure to blue light during nighttime hours.
- Time Management: While it may be challenging to completely eliminate screen time before bed, establishing a buffer period between screen use and sleep can significantly reduce the disruptive effects of blue light. Aim to limit screen time, especially in the two to three hours leading up to bedtime. During this time, engage in relaxing activities that promote winding down, such as reading a book, practicing mindfulness or meditation, or listening to calming music. This transition period allows your body to adjust and prepare for restful sleep.
It’s important to note that the effectiveness of these strategies may vary from person to person. Experimenting with different approaches and finding what works best for you is key. Additionally, it’s always advisable to consult with healthcare professionals or sleep specialists for personalized advice tailored to your specific needs and circumstances.
By implementing these solutions and reducing blue light exposure, you can support your natural sleep-wake cycle and enhance the quality of your sleep. Prioritizing good sleep hygiene, alongside other healthy lifestyle practices, is crucial for overall well-being and optimal functioning during waking hours.
In summary, reducing blue light exposure is a vital step in promoting restful sleep. Whether through adjusting device settings, using external filters or blue light blocking glasses, modifying your sleep environment, or managing your screen time effectively, incorporating these strategies into your daily routine can have a positive impact on your sleep quality and overall health. Remember, small changes can make a big difference when it comes to ensuring a good night’s sleep.
Author: Sharon Lojun, M.D., M.S.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
References
- Settings on Devices: Cain, N., & Gradisar, M. (2010). Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Medicine, 11(8), 735-742. doi: 10.1016/j.sleep.2010.02.006
- External Screen Filters: Figueiro, M. G., & Rea, M. S. (2012). The effects of red and blue lights on circadian variations in cortisol, alpha amylase, and melatonin. International Journal of Endocrinology, 2012, 1-9. doi: 10.1155/2012/461739
- Glasses: Chellappa, S. L., Steiner, R., Blattner, P., & Oelhafen, P. (2017). Got rhythm?—Better sleep with customized light and sleep therapy. Journal of Biological Rhythms, 32(4), 322-330. doi: 10.1177/0748730417713572
- Curtains: Bedrosian, T. A., & Nelson, R. J. (2013). Timing of light exposure affects mood and brain circuits. Translational Psychiatry, 3(3), e249. doi: 10.1038/tp.2013.27
Exploring the Role of Prebiotics, Probiotics, and Postbiotics in a Keto Diet
- May 15, 2024
- Stephen Fitzmeyer, MD
- No Comments
Introduction: The ketogenic diet, known for its low-carbohydrate and high-fat approach, has gained popularity for weight loss and metabolic benefits. While specific keto foods do not naturally contain probiotics, incorporating fermented foods into the diet can provide probiotic benefits. Additionally, understanding the concepts of prebiotics and postbiotics can further enhance gut health and overall well-being. In this article, we will delve into the significance of prebiotics, probiotics, and postbiotics within the context of a ketogenic diet.
Probiotic Sources in a Keto Diet: Fermented vegetables, such as sauerkraut and kimchi, can be included in a ketogenic diet to introduce beneficial bacteria. Look for options without added sugars or high-carb ingredients. Some low-carb, unsweetened, full-fat yogurts containing live and active cultures, like Lactobacillus acidophilus and Bifidobacterium strains, can also be suitable. Kefir, whether made from milk or non-dairy alternatives like coconut milk or water, provides a range of beneficial bacteria and yeast strains. Additionally, naturally fermented pickles and miso can be considered, but portion control is essential due to their carbohydrate content.
Understanding Prebiotics: Prebiotics are non-digestible fibers that serve as food for beneficial gut bacteria. While not providing direct probiotic benefits, they help nourish and support the growth of beneficial bacteria in the gut. Some prebiotic-rich keto-friendly foods include non-starchy vegetables like leafy greens, broccoli, cauliflower, asparagus, and garlic. These can be incorporated into meals to promote a healthy gut microbiota while maintaining ketosis.
The Role of Postbiotics: Postbiotics are the byproducts or metabolites produced by probiotic bacteria during fermentation. They include substances like short-chain fatty acids (SCFAs), enzymes, vitamins, and organic acids. SCFAs, such as butyrate, acetate, and propionate, have been extensively studied for their health benefits. They can regulate the immune system, support gut barrier function, and have anti-inflammatory and antimicrobial effects. While research on postbiotics is still emerging, they show promise as a way to reap the benefits of probiotics without consuming live bacteria.
Conclusion: Incorporating prebiotic-rich foods, fermented vegetables, and certain types of yogurt, kefir, pickles, and miso can provide probiotic benefits while following a keto diet. These foods can help nourish the gut microbiota and promote a healthy balance of beneficial bacteria. Additionally, understanding the role of prebiotics and postbiotics adds depth to gut health management. Prebiotic-rich foods like non-starchy vegetables support the growth of beneficial bacteria, while postbiotics offer potential health benefits without the need for live bacteria. As always, it is important to consult with healthcare professionals or registered dietitians for personalized advice based on individual dietary needs and health considerations. By incorporating prebiotics, probiotics, and understanding postbiotics, individuals can optimize their gut health while following a keto diet and reap the potential benefits for overall well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unleashing the Potential of Polyphenols: Reversing Metabolic Syndrome Naturally
- May 10, 2024
- Stephen Fitzmeyer, MD
- No Comments
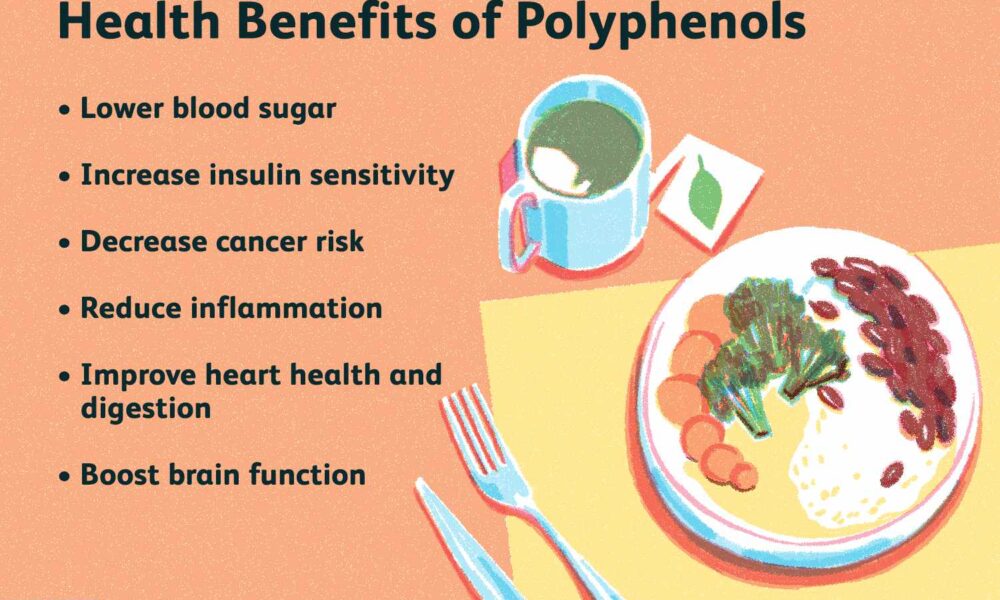
Introduction: Metabolic syndrome poses a significant threat to cardiovascular health and overall well-being. However, emerging research suggests that the natural compounds known as polyphenols may hold the key to reversing metabolic syndrome and promoting better health. Abundant in various fruits, vegetables, whole grains, nuts, and beverages like tea and coffee, polyphenols offer numerous health benefits. In this article, we will delve into the importance of polyphenols in combating metabolic syndrome and explore how they can be incorporated into a healthy lifestyle.
- Combating Inflammation and Oxidative Stress: Polyphenols are renowned for their potent antioxidant and anti-inflammatory properties. By neutralizing harmful free radicals and reducing chronic low-grade inflammation, these compounds address the root causes of metabolic syndrome. Including polyphenol-rich foods in your diet can help fortify your body’s defense against oxidative stress and inflammation, thereby reducing the risk of developing metabolic abnormalities.
- Improving Insulin Sensitivity: Insulin resistance is a hallmark of metabolic syndrome, characterized by diminished cellular response to insulin. Polyphenols have shown promise in enhancing insulin sensitivity, enabling cells to efficiently absorb glucose from the bloodstream. By improving insulin sensitivity, polyphenols help regulate blood sugar levels and reduce the risk of developing type 2 diabetes, a common consequence of metabolic syndrome.
- Lowering Lipid Levels: Polyphenols have been found to possess lipid-lowering effects, particularly by reducing LDL cholesterol (the “bad” cholesterol) and triglyceride levels, while increasing HDL cholesterol (the “good” cholesterol”). Dyslipidemia, an abnormal lipid profile, is a significant component of metabolic syndrome. By incorporating polyphenol-rich foods into your diet, you can restore a healthier lipid profile, reducing the risk of cardiovascular disease associated with metabolic syndrome.
- Managing Blood Pressure: Hypertension, or high blood pressure, is prevalent in individuals with metabolic syndrome. Polyphenols have demonstrated the ability to lower blood pressure through various mechanisms. They promote the production of nitric oxide, a compound that relaxes blood vessels, leading to improved blood flow and reduced blood pressure. Additionally, certain polyphenols possess diuretic properties, aiding in the excretion of excess sodium and water, further contributing to blood pressure regulation.
- Modulating Gut Health: Emerging research suggests that polyphenols can influence the composition and activity of the gut microbiota, the complex community of microorganisms residing in our digestive system. A healthy gut microbiota plays a crucial role in maintaining metabolic balance and overall well-being. Polyphenols can act as prebiotics, nourishing beneficial bacteria and promoting a diverse and balanced gut microbiota. This interaction between polyphenols and the gut microbiota may contribute to improving metabolic parameters associated with metabolic syndrome.
Conclusion: Polyphenols offer a promising avenue for reversing metabolic syndrome and improving overall health. By incorporating polyphenol-rich foods into your diet, you can harness their antioxidant, anti-inflammatory, insulin-sensitizing, lipid-lowering, blood pressure-regulating, and gut microbiota-modulating properties. Remember that a holistic approach, including regular physical activity, weight management, and professional guidance, is crucial in managing metabolic syndrome effectively. Embrace the power of polyphenols and embark on a journey towards a healthier, metabolic syndrome-free life.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Reversing Type 2 Diabetes or Prediabetes with Keto and Intermittent Fasting
- May 5, 2024
- Stephen Fitzmeyer, MD
- No Comments
Introduction: Type 2 diabetes and prediabetes have become increasingly prevalent health concerns, affecting millions of people worldwide. However, emerging research suggests that adopting a combination of the ketogenic diet (keto) and intermittent fasting (IF) can be a powerful strategy to reverse or manage these conditions effectively. In this article, we will explore how embracing the keto lifestyle and incorporating intermittent fasting can help you take control of your blood sugar levels, improve insulin sensitivity, and potentially reverse type 2 diabetes or prediabetes.
Understanding Type 2 Diabetes and Prediabetes: Type 2 diabetes is a chronic condition characterized by high blood sugar levels resulting from insulin resistance and inadequate insulin production. Prediabetes, on the other hand, refers to a condition where blood sugar levels are higher than normal but not yet in the diabetic range. Both conditions are strongly associated with lifestyle factors, including poor diet, sedentary behavior, and obesity.
The Power of the Ketogenic Diet (Keto): The ketogenic diet is a low-carbohydrate, high-fat eating plan that encourages the body to enter a state of ketosis. By significantly reducing carbohydrate intake and increasing healthy fat consumption, keto prompts the body to shift its primary fuel source from glucose to ketones. This metabolic shift can lead to improved blood sugar control, reduced insulin resistance, and enhanced weight management. Studies have shown that following a keto diet can result in significant improvements in glycemic control and insulin sensitivity for individuals with type 2 diabetes or prediabetes.
Intermittent Fasting (IF) for Blood Sugar Management: Intermittent fasting involves cycling between periods of eating and fasting. This practice can improve insulin sensitivity, enhance cellular repair processes, and promote weight loss. By allowing the body to enter fasting states, intermittent fasting helps regulate blood sugar levels and reduces insulin resistance. Intermittent fasting can be practiced in various ways, such as the 16:8 method (fasting for 16 hours and eating within an 8-hour window) or alternate-day fasting. It is essential to work with healthcare professionals or registered dietitians to determine the most suitable fasting approach for your individual needs.
Reversing Type 2 Diabetes and Prediabetes: By combining the benefits of the ketogenic diet and intermittent fasting, individuals with type 2 diabetes or prediabetes can potentially reverse or effectively manage their conditions. Keto helps control blood sugar levels by reducing carbohydrate intake and relying on ketones for energy. Intermittent fasting further enhances blood sugar management by improving insulin sensitivity and supporting weight loss. When implemented consistently and under medical supervision, this approach can lead to significant improvements in glycemic control, weight reduction, and overall metabolic health.
The Importance of Personalized Approaches: It’s crucial to note that reversing type 2 diabetes or prediabetes with keto and intermittent fasting requires an individualized approach. Working closely with healthcare professionals or registered dietitians who specialize in metabolic health is essential to ensure the right balance of nutrients, appropriate monitoring, and adjustment of medications as needed. Regular blood sugar monitoring, medical check-ups, and ongoing support are crucial components of a successful journey towards improved metabolic health.
Empowering Yourself for a Healthier Future: Reversing type 2 diabetes or prediabetes with keto and intermittent fasting is not a quick fix but a long-term commitment to your well-being. By embracing this lifestyle approach, you can regain control of your blood sugar levels, reduce reliance on medications, and potentially reverse the course of these conditions. Remember to prioritize whole, nutrient-dense foods, stay physically active, manage stress levels, and maintain a supportive network to sustain your journey towards better metabolic health.
Conclusion: The combination of the ketogenic diet and intermittent
fasting has shown promising results in reversing type 2 diabetes or prediabetes. With a focus on low-carbohydrate, high-fat eating and incorporating periods of fasting, individuals can improve their blood sugar control, enhance insulin sensitivity, and potentially reverse these conditions. However, it is crucial to work closely with healthcare professionals or registered dietitians who can provide personalized guidance and monitor your progress throughout the process.
Taking control of your health now through the power of keto and intermittent fasting can help you avoid the chronic diseases that plague so many individuals today. By making proactive choices and embracing a lifestyle that prioritizes your well-being, you can break free from the cycle of diabetes and pave the way for a healthier future.
Remember, reversing type 2 diabetes or prediabetes requires commitment, patience, and ongoing support. Surround yourself with a supportive network, stay informed about the latest research and developments, and consult with healthcare professionals who specialize in metabolic health. By taking charge of your nutrition and lifestyle choices, you can rewrite your health story and experience the transformative effects of keto and intermittent fasting.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Recent Posts
- Protected: Warp Core Health: Building a Custom AI Model for Transforming Healthcare
- The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
- Accessing Siloed EMR Systems with FHIR: Connecting to Multiple EMRs
- How AI and Informatics Are Transforming Healthcare
- How AI Can Transform Healthcare Applications
Categories
- ApoB
- Artificial Intelligence
- Autophagy
- Biochemistry
- Biomedical Informatics
- Biostatistics
- Blood Glucose
- CAC
- Carbs
- CCD
- CDA
- Clinical Informatics
- Coding Bootcamp
- Coronary Artery Disease
- COVID-19
- Cybersecurity
- Data Science
- Diabetes
- Diet
- EHS
- EMR
- Epidemiology
- Evidence Based Medicine
- Fats
- FHIR
- Fiber
- Generative AI
- Global Health
- Health Administration
- Health Informatics
- Health IT
- HIPAA
- HL7
- Hyperglycemia
- Hypoglycemia
- ICD 10
- Intermittent Fasting
- Ketogenic Diet
- Machine Learning
- Macronutrients
- MCT Oil
- Metabolic Health
- Metabolic Syndrome
- Minerals
- Mitochondria
- MySQL
- Neurology
- Nutritional Ketosis
- Nutritional Neurology
- Nutritional Psychiatry
- PHP
- PHR
- Programming
- Prompt Engineering
- Proteins
- Prototypes
- Public Health
- Python
- Recipes
- Sleep Health
- Stroke
- Uric Acid
- Vegan and Vegetarians
- Vitamin D
- Vitamin K2
- Vitamins