- Home
- About
- Portfolio
- Crush the Match – Medical School and Residency Platform
- Food¢ense – Curbing Childhood Obesity and Food Waste
- HealthStack – Shared and Jailed HIPAA Hosting $50
- Marta Care – Let Us Help When You Can’t
- MD Idea Lab – We Build Prototypes for Doctors
- Nervcell – The Healthcare Web Browser
- Patient Keto – Personalized Keto Medicine and Telehealth
- SwipeChart – Rapid EMR Interface
- Treatment Scores – Quantifying the Science of Medicine
- Treatments – Diagnosed. Now What?
- VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Evidence Based Medicine
Unveiling the Mysteries of Epidemiology: The Backbone of Medicine
Introduction
In the vast realm of medicine, epidemiology stands as an unsung hero – the silent sentinel that plays a pivotal role in preventing, controlling, and understanding diseases. While this field may not garner the same attention as groundbreaking medical discoveries, it is the backbone that supports the entire healthcare system. In this article, we delve into the fascinating world of epidemiology, shedding light on what it is, why it matters, and how it shapes the practice of medicine.
What is Epidemiology?
Epidemiology is often described as the science of public health. It is the study of how diseases spread and impact populations, and it seeks to understand the patterns, causes, and consequences of health and disease in human communities. This field employs a variety of research methods to investigate the distribution and determinants of health-related outcomes, with the ultimate goal of improving public health.
Why Does Epidemiology Matter in Medicine?
Disease Prevention and Control:
Epidemiology plays a pivotal role in preventing and controlling diseases. By identifying risk factors, understanding the transmission of diseases, and evaluating interventions, epidemiologists help develop strategies to mitigate the impact of illnesses.
Public Health Policy:
Policymakers rely on epidemiological data to make informed decisions. This information helps shape public health policies, such as vaccination programs, smoking bans, and disaster preparedness, to protect and improve public health.
Outbreak Investigations:
During disease outbreaks, epidemiologists are the first responders. They conduct field investigations to identify the source of the outbreak, understand its transmission, and implement measures to contain it.
Research and Innovation:
Epidemiological studies provide the foundation for medical research. They generate hypotheses, drive clinical trials, and lead to the development of new treatments and therapies.
Key Concepts in Epidemiology
Incidence and Prevalence:
Incidence measures the rate of new cases of a disease within a specific time frame and population. Prevalence, on the other hand, reflects the total number of cases within a population at a given time. These metrics are essential for understanding the burden of diseases.
Risk Factors:
Identifying risk factors, such as genetics, lifestyle choices, and environmental exposures, is crucial in preventing diseases. Epidemiologists help pinpoint these factors, allowing for targeted interventions.
Cohort Studies and Case-Control Studies:
Cohort studies follow a group of individuals over time to assess the development of diseases, while case-control studies compare those with a specific condition to those without it. Both study designs help unravel the causes of diseases.
Outbreak Investigations:
During outbreaks, epidemiologists work swiftly to trace the origins of the disease, identify its transmission patterns, and implement control measures to limit its spread.
Surveillance Systems:
Epidemiologists use surveillance systems to monitor diseases on an ongoing basis. These systems enable early detection of outbreaks, providing a chance for swift intervention.
Challenges in Epidemiology
Epidemiology is not without its challenges. The field faces obstacles such as the difficulty of establishing causation, the ethical concerns surrounding experiments on human populations, and the evolving nature of diseases. With the rise of emerging infectious diseases and the increasing globalization of health threats, epidemiologists must adapt to new challenges continuously.
Conclusion
Epidemiology is the silent force that ensures the well-being of societies by enabling the prevention and control of diseases. In the practice of medicine, this field provides the essential knowledge and tools to understand the spread of illnesses, identify risk factors, and develop effective strategies for disease prevention and treatment. As medicine and healthcare evolve, epidemiology will remain a steadfast ally, contributing to the health and longevity of humanity. It is the unsung hero that keeps us safe, vigilant, and prepared for the health challenges of the future.
Coding Evidence-Based Medicine into Web-Based Applications
By Stephen Fitzmeyer, MD
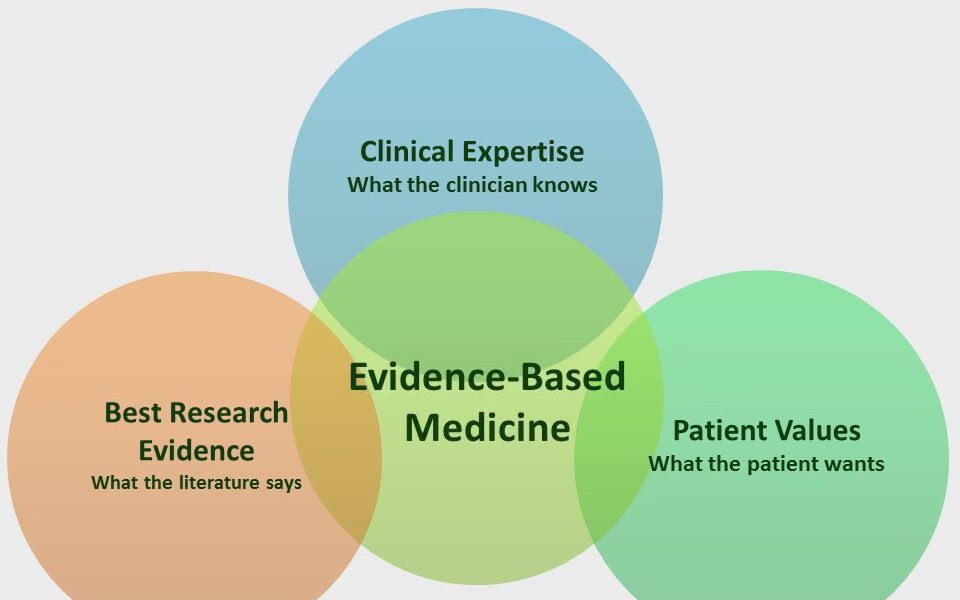
Evidence-based medicine (EBM) is a medical approach that involves using the best available evidence to make informed clinical decisions. The goal of EBM is to improve the quality of patient care by integrating research evidence, clinical expertise, and patient preferences into clinical decision making. In recent years, there has been a growing interest in using technology to support EBM and help clinicians make evidence-based decisions. Web-based applications are a popular way to accomplish this goal.
Web-based applications that incorporate EBM can provide clinicians with easy access to the latest research evidence, as well as clinical practice guidelines and other relevant resources. These applications can help clinicians make informed decisions about diagnosis, treatment, and management of a wide range of medical conditions.
The process of building a web-based EBM application involves several steps. The first step is to identify the target audience and determine the specific clinical needs that the application will address. This may involve conducting a needs assessment and identifying gaps in current clinical practice.
The second step is to identify relevant EBM resources and integrate them into the application. This may involve using electronic databases, such as PubMed or Cochrane Library, to search for the latest research evidence. It may also involve incorporating clinical practice guidelines, systematic reviews, and other evidence-based resources into the application.
Once the relevant EBM resources have been identified, the next step is to design the application’s user interface. The application should be easy to navigate, intuitive to use, and provide users with relevant information at the appropriate time. The design of the application should be based on user-centered design principles, which involve actively involving users in the design process and incorporating their feedback into the final product.
After the application has been designed, the next step is to develop the application using web development languages and frameworks such as HTML, CSS, JavaScript, and React. The application may also incorporate server-side programming languages such as PHP or Python, and databases such as MongoDB or MySQL to store and retrieve data.
Finally, the application should be tested and validated to ensure that it is functioning as intended and providing accurate and reliable information to users. This may involve user testing, where the application is tested by actual users, as well as usability testing, where the application is tested for ease of use and effectiveness.
In conclusion, web-based applications that incorporate EBM can provide clinicians with easy access to the latest research evidence and clinical practice guidelines, helping them make informed decisions about patient care. The development of these applications involves identifying the target audience and their clinical needs, integrating relevant EBM resources, designing an intuitive user interface, developing the application using web development languages and frameworks, and testing and validating the application to ensure that it is effective and reliable. By following these steps, developers can build web-based EBM applications that improve patient care and support evidence-based decision making in clinical practice.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/