- Home
- About
- Portfolio
- Crush the Match – Medical School and Residency Platform
- Food¢ense – Curbing Childhood Obesity and Food Waste
- HealthStack – Shared and Jailed HIPAA Hosting $50
- Marta Care – Let Us Help When You Can’t
- MD Idea Lab – We Build Prototypes for Doctors
- Nervcell – The Healthcare Web Browser
- Patient Keto – Personalized Keto Medicine and Telehealth
- SwipeChart – Rapid EMR Interface
- Treatment Scores – Quantifying the Science of Medicine
- Treatments – Diagnosed. Now What?
- VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Nutritional Psychiatry
Exploring the Potential of Ketogenic Diet and Intermittent Fasting in Schizoaffective Disorder Management
Introduction:
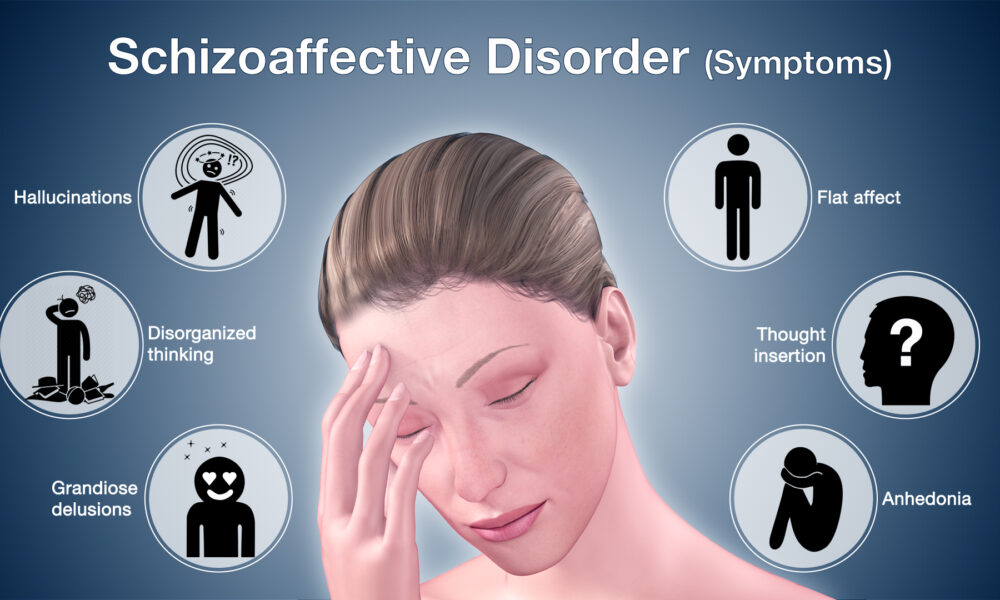
Schizoaffective disorder is a complex psychiatric condition characterized by a combination of mood disorders, such as bipolar disorder or major depression, and schizophrenia symptoms. While medication and therapy are commonly used in its treatment, emerging research suggests that dietary interventions, specifically the ketogenic diet and intermittent fasting, may hold promise in managing symptoms and improving overall well-being for individuals with schizoaffective disorder. In this article, we will explore the potential efficacy of adopting a ketogenic diet and intermittent fasting in the management of schizoaffective disorder.
Understanding Schizoaffective Disorder:
Schizoaffective disorder is a challenging mental health condition that often requires a comprehensive approach to treatment. It is characterized by a range of symptoms, including hallucinations, delusions, disorganized thinking, mood disturbances, and cognitive impairments. Conventional treatment typically involves a combination of antipsychotic medications, mood stabilizers, and psychotherapy.
The Potential Benefits of Ketogenic Diet:
- Enhanced Mood Stability: The ketogenic diet has been associated with improved mood regulation and stability. By stabilizing blood sugar levels and providing a steady supply of ketones to the brain, the diet may help mitigate mood swings and promote emotional balance, potentially benefiting individuals with schizoaffective disorder.
- Cognitive Improvements: Cognitive impairments are common in schizoaffective disorder. The ketogenic diet has shown potential in enhancing cognitive function, including memory and attention. The neuroprotective properties of ketones may help support neuronal health and improve cognitive performance in individuals with schizoaffective disorder.
- Reduction in Inflammation: Inflammation has been linked to the development and progression of psychiatric disorders. The ketogenic diet’s anti-inflammatory effects may help mitigate neuroinflammation, potentially contributing to the management of symptoms in schizoaffective disorder.
The Potential Benefits of Intermittent Fasting:
- Neuroprotective Effects: Intermittent fasting has been shown to induce cellular stress responses that promote cellular repair and resilience. This process, known as autophagy, may help clear damaged cells and dysfunctional proteins, potentially improving neuronal health and protecting against the progression of schizoaffective disorder.
- Regulation of Mood: Intermittent fasting has been associated with improvements in mood and mental well-being. The regulation of neurotransmitters and the production of brain-derived neurotrophic factor (BDNF) during fasting periods may contribute to mood stabilization and alleviate depressive symptoms commonly associated with schizoaffective disorder.
- Improved Antipsychotic Medication Efficacy: Some research suggests that intermittent fasting may enhance the effectiveness of antipsychotic medications. Fasting-related changes in metabolic processes and gene expression may influence drug metabolism and efficacy, potentially leading to better symptom management.
Considerations and Consultation:
It is crucial to approach the implementation of a ketogenic diet or intermittent fasting under the guidance of healthcare professionals experienced in these dietary interventions, especially when managing a complex condition like schizoaffective disorder. They can provide individualized recommendations, monitor progress, and ensure nutritional needs are met.
It is important to note that dietary interventions should be integrated into a comprehensive treatment plan that includes regular psychiatric evaluation, medication management, therapy, and other supportive measures tailored to the individual’s needs.
Conclusion:
While research on the specific effects of ketogenic diet and intermittent fasting in schizoaffective disorder is limited, emerging evidence suggests their potential benefits in managing symptoms and improving overall well-being. These dietary interventions have shown promise in mood stabilization, cognitive enhancement, reduction of inflammation, and neuroprotection. As with any treatment approach, it is crucial to consult with healthcare professionals to tailor these interventions to individual needs and ensure comprehensive care. Further research is needed to
further investigate the efficacy, safety, and long-term effects of ketogenic diet and intermittent fasting in schizoaffective disorder.
As the field of nutritional psychiatry continues to evolve, exploring the potential of dietary interventions in the management of schizoaffective disorder is an exciting area of research. The ketogenic diet and intermittent fasting offer unique mechanisms that may complement conventional treatment approaches and improve outcomes for individuals with this complex condition.
However, it is important to approach these interventions with caution and under the supervision of healthcare professionals. Each person’s response to dietary changes can vary, and careful monitoring is necessary to ensure that nutritional needs are met, potential side effects are addressed, and the interventions are integrated effectively into the overall treatment plan.
Future studies should focus on conducting rigorous clinical trials to investigate the specific effects of ketogenic diet and intermittent fasting in schizoaffective disorder. This research should explore optimal dietary protocols, long-term sustainability, potential interactions with medications, and the impact on specific symptoms and functional outcomes.
In conclusion, while the ketogenic diet and intermittent fasting show promise in the management of schizoaffective disorder, further research is needed to establish their efficacy, safety, and long-term effects. By combining the advancements in nutritional psychiatry with conventional treatment approaches, we may unlock new possibilities for improving the lives of individuals with schizoaffective disorder and enhancing their mental well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Nutritional Psychiatry: Harnessing the Power of Ketogenic Diet and Intermittent Fasting for Mental Well-being
Introduction:
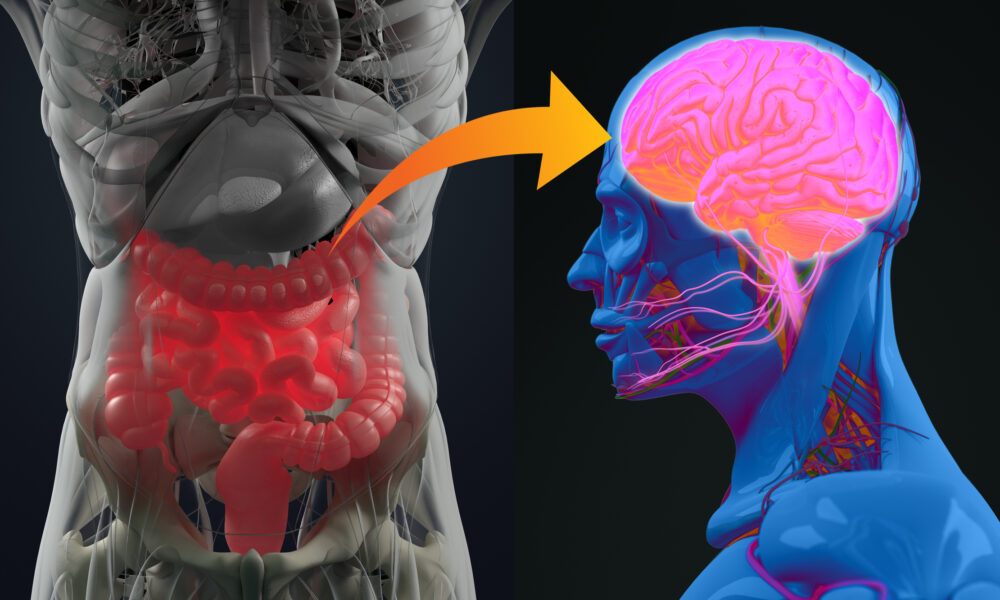
The field of nutritional psychiatry is gaining recognition as research increasingly highlights the profound connection between diet and mental health. Emerging evidence suggests that dietary interventions, such as the ketogenic diet and intermittent fasting, can play a significant role in the treatment of psychiatric disorders. In this article, we will explore the potential benefits of adopting a ketogenic diet and intermittent fasting as therapeutic strategies for improving mental well-being.
The Ketogenic Diet: Nourishing the Brain
The ketogenic diet is a low-carbohydrate, high-fat eating plan that shifts the body’s metabolism into a state of ketosis. This metabolic state prompts the production of ketones, which become the brain’s primary fuel source, replacing glucose. Here’s how the ketogenic diet can positively impact mental health:
- Stabilizing Mood and Mental Clarity: The ketogenic diet has been associated with improved mood stability and mental clarity. By reducing blood sugar fluctuations and providing a steady supply of ketones to the brain, the diet may help regulate neurotransmitters and promote a balanced emotional state.
- Reducing Inflammation: Chronic inflammation is often linked to psychiatric disorders. The ketogenic diet has shown anti-inflammatory effects, potentially alleviating inflammation in the brain and contributing to improved mental health outcomes.
- Enhancing Neuroprotection: Ketones produced during ketosis have neuroprotective properties, potentially shielding the brain from oxidative stress and supporting neuronal function. This neuroprotective effect may be particularly relevant in the treatment of conditions such as Alzheimer’s disease and epilepsy.
Intermittent Fasting: Resetting the Mind and Body
Intermittent fasting (IF) involves cycling between periods of eating and fasting, which can have profound effects on brain function and mental well-being. Here are some ways IF may benefit mental health:
- Promoting Autophagy: During fasting periods, the body enters a state of autophagy, a process where damaged cells and cellular components are recycled and cleared. Autophagy supports cellular renewal and may play a vital role in clearing protein aggregates associated with neurodegenerative disorders.
- Enhancing Brain-Derived Neurotrophic Factor (BDNF): IF has been shown to increase the production of BDNF, a protein crucial for the growth and survival of neurons. Higher levels of BDNF have been associated with improved mood, cognitive function, and the prevention of mental disorders.
- Regulating Circadian Rhythms: IF helps regulate the body’s internal clock, which governs various physiological processes, including sleep patterns. Proper regulation of circadian rhythms is essential for mental well-being, as disruptions can contribute to mood disorders and cognitive impairments.
Implementing a Nutritional Psychiatry Approach
While the ketogenic diet and intermittent fasting show promise in the treatment of psychiatric disorders, it is essential to approach these interventions with care and under professional guidance. Here are a few considerations:
- Personalization: Nutritional psychiatry interventions should be tailored to individual needs and goals. Consulting with a healthcare professional or registered dietitian experienced in these approaches can help determine the most suitable strategies.
- Monitoring and Evaluation: Regular monitoring of mental health symptoms and overall well-being is crucial during dietary interventions. Adjustments to the diet or fasting protocols may be necessary to optimize outcomes.
- Comprehensive Approach: Nutritional psychiatry should be considered as part of a holistic approach to mental health. It is essential to address other aspects such as exercise, sleep, stress management, and social support to achieve optimal outcomes.
Conclusion:
The emerging field of nutritional psychiatry highlights the powerful impact of diet on mental well-being. The ketogenic diet and intermittent fasting offer promising strategies for treating psychiatric disorders by nourishing the brain, reducing inflammation, promoting
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/