- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Diabetes
Protecting and Repairing the Glycocalyx: The Key to Vascular Health
Title: Protecting and Repairing the Glycocalyx: The Key to Vascular Health
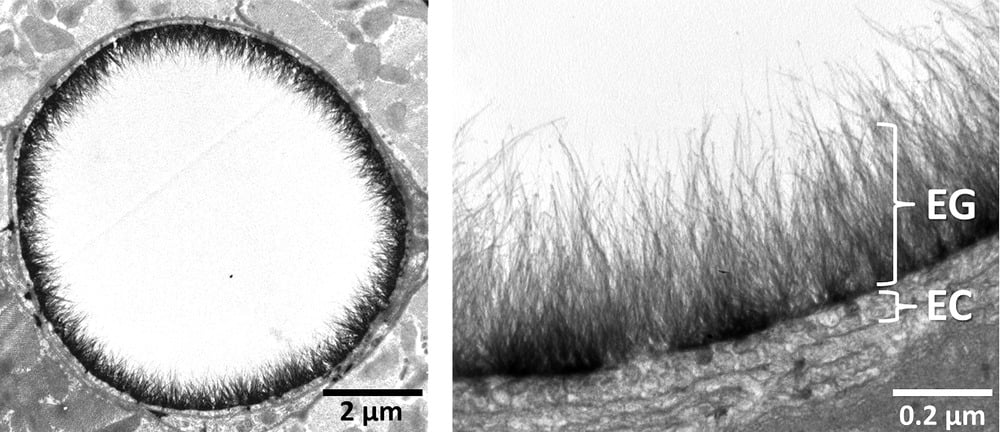
In recent years, the glycocalyx has gained attention in the health and wellness world, especially for its crucial role in vascular health. This thin, gel-like layer on the surface of cells, particularly on the endothelial cells lining our blood vessels, plays a vital role in keeping our blood vessels healthy and free from dangerous plaques. But what exactly is the glycocalyx, how does it get damaged, and, importantly, how can we repair it? Let’s dive into the science and strategies behind protecting this vital structure.
What Is the Glycocalyx?
The glycocalyx is a delicate, sugar-rich coating found on the surface of many cells. It’s particularly abundant on endothelial cells, which form the inner lining of blood vessels. Made of glycoproteins, glycolipids, and proteoglycans, the glycocalyx serves as a protective shield, helping to:
- Maintain smooth blood flow by reducing friction.
- Prevent blood cells and harmful substances like oxidized LDL (low-density lipoprotein) from sticking to vessel walls.
- Act as a barrier against pathogens.
- Enable cellular communication through various signaling molecules.
The glycocalyx is essentially the first line of defense for our blood vessels, safeguarding them from inflammation and damage. However, modern lifestyle factors can lead to glycocalyx damage, contributing to vascular diseases such as atherosclerosis.
How Does Glycocalyx Damage Lead to Plaque Buildup?
When the glycocalyx is damaged, it loses its integrity, making it easier for harmful molecules like oxidized LDL cholesterol to interact with the endothelial cells underneath. This damage can trigger an inflammatory response in the vessel wall, which can initiate plaque formation. Over time, as plaque builds up, it can restrict blood flow, leading to conditions like heart attacks, strokes, and other cardiovascular issues.
The Impact of High Blood Sugar and Fats on the Glycocalyx
Chronic high blood sugar, often seen in diabetes, and certain types of fats can contribute to glycocalyx damage. Here’s how:
- Oxidative Stress from Hyperglycemia:
- When blood sugar levels remain high, they trigger an overproduction of reactive oxygen species (ROS) in the endothelial cells. These molecules are highly reactive and can damage cellular structures, including the glycocalyx, by breaking down its carbohydrate components.
- Inflammation and Glycation:
- High blood sugar leads to the formation of advanced glycation end products (AGEs), which occur when glucose molecules bind to proteins and fats. These AGEs accumulate in blood vessels, directly interacting with and damaging the glycocalyx. They also activate receptors (RAGE) on endothelial cells, triggering inflammation and further degrading the glycocalyx.
- Excessive Omega-6 Intake and Inflammation:
- A high intake of omega-6 fatty acids, often from seed oils like soybean, corn, and sunflower oils, can shift the body toward a pro-inflammatory state. This imbalance between omega-6 and omega-3 fatty acids can increase inflammation that directly harms the glycocalyx.
- By creating an inflammatory response, omega-6 fatty acids contribute to oxidative stress and enzymatic activity that breaks down glycocalyx components. Replacing seed oils with anti-inflammatory fats, such as those found in olive oil, avocado oil, and fatty fish, can help protect the glycocalyx by reducing these inflammatory triggers.
- Enzymatic Degradation:
- Hyperglycemia and oxidative stress stimulate enzymes like heparanase and hyaluronidase, which break down the glycocalyx components such as heparan sulfate and hyaluronic acid, causing it to thin.
When the glycocalyx is compromised, the blood vessel becomes more permeable to cholesterol and other inflammatory molecules, leading to plaque buildup and increased cardiovascular risk.
The Role of Remnant Cholesterol and TG/HDL Ratios in Glycocalyx Assessment
For primary care providers (PCPs) and general practitioners (GPs), calculating a patient’s Remnant Cholesterol and Triglyceride-to-HDL (TG/HDL) ratio can provide a quick, valuable assessment of cardiovascular risk and potential glycocalyx damage. These indicators offer insight into lipid metabolism and inflammation, both of which affect the glycocalyx.
- Remnant Cholesterol: Calculated as total cholesterol minus LDL and HDL cholesterol, remnant cholesterol reflects the amount of triglyceride-rich lipoproteins. High levels are associated with increased risk of atherosclerosis and glycocalyx degradation, as these remnant particles can penetrate the endothelium and contribute to plaque formation.
- TG/HDL Ratio: The TG/HDL ratio is an easy-to-calculate marker of insulin resistance and metabolic health. High TG and low HDL levels often correlate with higher oxidative stress and systemic inflammation, both of which damage the glycocalyx. A TG/HDL ratio above 3.0 can indicate increased cardiovascular risk and a compromised glycocalyx.
Incorporating these markers into regular check-ups can help PCPs and GPs identify patients with higher glycocalyx damage risk, guiding preventive measures such as dietary adjustments, lifestyle changes, and early intervention.
Can the Glycocalyx Be Repaired?
The good news is that, while fragile, the glycocalyx can be repaired and maintained with the right dietary, lifestyle, and medical interventions. Here are some of the most effective strategies:
1. Control Blood Sugar Levels
- Dietary Changes: Reducing refined carbohydrates and sugars is essential for maintaining blood sugar levels. A diet focused on whole, unprocessed foods with a low glycemic index can minimize blood sugar spikes and the resulting oxidative stress.
- Exercise: Physical activity improves insulin sensitivity, helping regulate blood glucose and reduce glycocalyx damage from hyperglycemia.
- Medications: For individuals with diabetes, medications like metformin can help keep blood glucose within a healthy range, reducing the risk of glycocalyx damage.
2. Boost Antioxidants
- Vitamin C and E: These antioxidants help neutralize ROS, protecting the glycocalyx from oxidative damage.
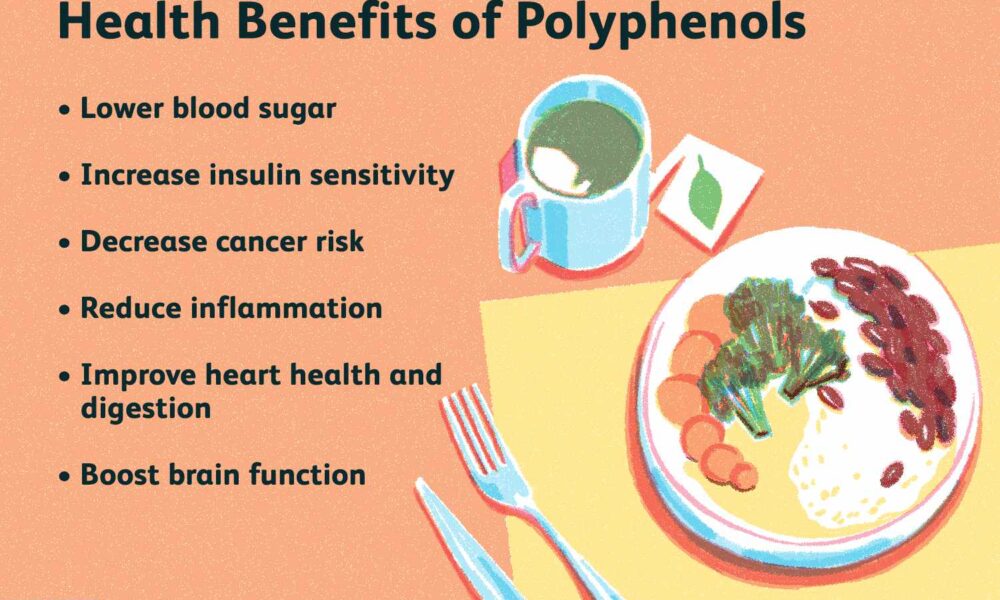
- Polyphenols: Found in foods like berries, green tea, and dark chocolate, polyphenols have anti-inflammatory properties and protect the glycocalyx from ROS. Resveratrol, a specific polyphenol in red wine, is known for supporting vascular health and glycocalyx repair.
- Omega-3 Fatty Acids: Known for their anti-inflammatory effects, omega-3s (found in fatty fish and fish oil supplements) help reduce inflammation and protect the glycocalyx from enzymatic degradation. They also help stabilize the endothelial cells, reducing breakdown of glycocalyx components.
3. Support Glycocalyx Health with Key Nutrients
- L-arginine: This amino acid boosts nitric oxide production, which improves endothelial function and supports glycocalyx repair.
- Hyaluronic Acid and Chondroitin Sulfate: These are essential building blocks of the glycocalyx, often found in joint supplements. They support glycocalyx structure and help it retain moisture, keeping it intact and functional.
- Sulfur-Rich Foods: Garlic, onions, and cruciferous vegetables contain sulfur, which supports the synthesis of glycosaminoglycans, vital components of the glycocalyx.
4. Adopt a Low-Carb Lifestyle and Eliminate Inflammatory Foods
A low-carb lifestyle, with the elimination of seed oils, grains, and sugars, is especially beneficial for glycocalyx health:
- Reduced Blood Sugar Spikes: Limiting carbohydrate intake stabilizes blood sugar, preventing the oxidative stress associated with high blood glucose. This lowers the formation of AGEs and reduces direct damage to the glycocalyx.
- Improved Insulin Sensitivity: A low-carb approach, often combined with exercise, enhances insulin sensitivity, allowing cells to better utilize glucose, thereby keeping blood sugar stable and minimizing glycocalyx damage.
- Eliminating Seed Oils: Seed oils, high in omega-6 fatty acids, are inflammatory when consumed in excess. By replacing these oils with healthy fats (like olive oil, avocado oil, and butter), inflammation can be reduced, preserving glycocalyx health.
- Removing Grains and Sugars: High-glycemic grains and sugars contribute to glycation, leading to AGEs that harm the glycocalyx. Focusing on nutrient-dense vegetables and quality proteins provides energy without causing the blood sugar spikes that damage vascular health.
5. Avoid Harmful Substances
- Reduce Inflammatory Fats: Trans fats and excessive omega-6 fats (commonly found in processed seed oils) contribute to inflammation that damages the glycocalyx. Focusing on anti-inflammatory fats like olive oil, avocado oil, and omega-3-rich foods can support vascular health.
- Limit Smoking and Alcohol: Both smoking and excessive alcohol increase oxidative stress and inflammation, damaging the glycocalyx. Avoiding these substances is key for vascular and overall health.
6. Explore Emerging Therapies and Supplements
- Glycocalyx-Targeted Supplements: Some supplements aim to support glycocalyx health directly with compounds like glycosaminoglycans, which are essential to its structure. These “endocalyx” supplements may help repair and strengthen the glycocalyx.
- Stem Cell and Regenerative Therapies: Though still in experimental stages, stem cell and regenerative therapies hold promise for repairing damaged glycocalyx in severe cases.
- Nitric Oxide (NO) Enhancing Therapies: Therapies that boost NO production in the endothelium are being researched for their potential to help restore glycocalyx health and improve overall vascular function.
The Path Forward for Glycocalyx Health
Protecting and repairing the glycocalyx is crucial for maintaining vascular health and preventing the progression of plaque buildup. By focusing on blood sugar control, boosting antioxidants, incorporating essential nutrients, and utilizing key indicators like Remnant Cholesterol and TG/HDL ratios, we can help assess, repair, and protect this delicate structure to support cardiovascular wellness. A low-carb lifestyle, especially one that excludes seed oils, grains, and sugars, provides even greater protection, creating conditions that allow the glycocalyx to repair and thrive.
As research continues, our understanding of the glycocalyx and its role in health will expand, unlocking even more ways to protect this remarkable structure and the vital functions it supports. By nurturing the glycocalyx, we’re investing in the foundation of our cardiovascular health, giving us a powerful tool for longevity and well-being.
Leveraging Fiber for Blood Sugar Control in a Ketogenic Diet: A Guide for Type 1 and Type 2 Diabetics
By Stephen Fitzmeyer, MD
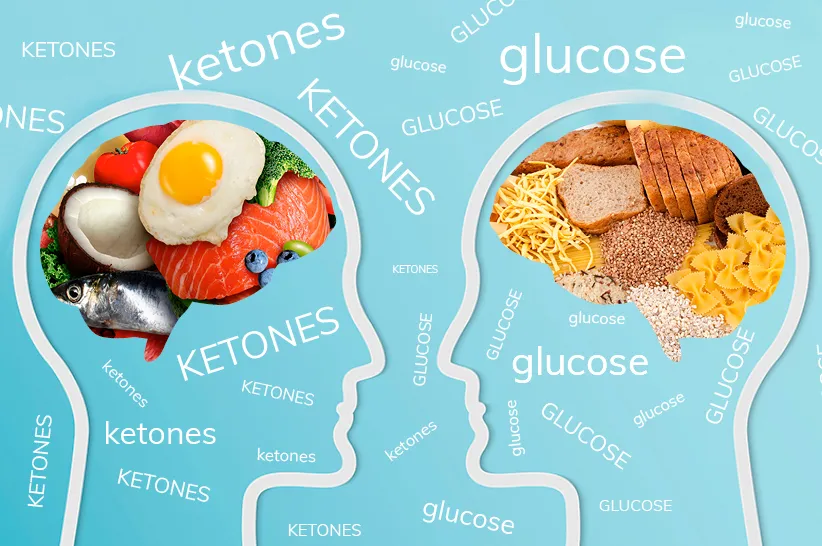
For individuals living with Type 1 or Type 2 diabetes, maintaining stable blood sugar levels is of utmost importance. While a ketogenic diet can be a beneficial approach for managing diabetes, it requires careful consideration of nutrient intake, including fiber. Incorporating fiber-rich foods into each meal can play a crucial role in controlling and stabilizing blood sugar levels. In this article, we will explore the scientific evidence supporting the use of fiber for blood sugar control in a ketogenic diet and provide practical recommendations for individuals with diabetes.
Introduction
For years, health-conscious individuals have been advised to consume fruit as part of a balanced diet due to its nutritional value and potential health benefits. However, recent studies have shed light on an important distinction between whole fruit and fruit juice regarding their effect on blood sugar levels. It turns out that the presence of fiber in whole fruit plays a significant role in slowing down the absorption of fructose, the natural sugar found in fruit. In contrast, fruit juice lacks the same fiber content, leading to a more rapid rise in blood sugar levels. Let’s delve deeper into the research and uncover the implications of these findings.
The Role of Fiber
Fiber is a key component of whole fruits that is absent in fruit juice. This dietary component consists of soluble and insoluble fibers, both of which contribute to a slower and more controlled release of sugars into the bloodstream. When consuming whole fruit, the fibrous structure acts as a physical barrier, reducing the speed at which sugars, including fructose, are absorbed. As a result, blood sugar levels rise more gradually, minimizing the risk of blood sugar spikes.
The Role of Fiber in Blood Sugar Control
Fiber-rich foods have a significant impact on blood sugar control. Fiber consists of indigestible carbohydrates that cannot be broken down by human enzymes. Instead, fiber passes through the digestive system relatively intact. There are two main types of fiber: soluble fiber and insoluble fiber. Both types contribute to blood sugar control in different ways.
Soluble fiber forms a gel-like substance in the digestive tract, slowing down the digestion and absorption of carbohydrates, including sugars. This results in a more gradual release of glucose into the bloodstream, preventing sudden spikes in blood sugar levels. Insoluble fiber, on the other hand, adds bulk to the stool, promoting regular bowel movements and preventing constipation, a common issue for individuals with diabetes.
Scientific Studies on Fiber and Blood Sugar Control
Numerous studies have investigated the effects of fiber on blood sugar control, including its impact on postprandial glucose levels (blood sugar levels after a meal) and glycemic control over the long term.
A study published in the journal “Diabetes Care” examined the effects of a high-fiber diet on glycemic control in individuals with Type 2 diabetes. The researchers found that participants who consumed a diet rich in fiber experienced significant improvements in glycemic control, including reduced HbA1c levels (a marker of long-term blood sugar control) and lower postprandial glucose levels.
Another study published in the “Journal of Clinical Nutrition” compared the effects of two different breakfast meals on blood sugar control in individuals with Type 2 diabetes. One meal contained high-fiber foods such as oats and fruits, while the other meal contained low-fiber foods. The researchers found that the high-fiber breakfast led to significantly lower postprandial glucose levels and improved overall glycemic control compared to the low-fiber breakfast.
Slower Absorption and Glycemic Index
The glycemic index (GI) is a measure of how quickly a particular food raises blood sugar levels. Foods with a low GI are digested and absorbed more slowly, leading to a gradual increase in blood sugar levels. Several studies have compared the glycemic index of whole fruit and fruit juice, consistently finding that whole fruit has a lower GI than its juice counterpart.
One study published in the journal “Diabetes Care” compared the effects of consuming whole apples versus apple juice in a group of participants. The researchers found that whole apples had a lower glycemic response, resulting in a more gradual increase in blood sugar levels, compared to apple juice. These findings highlight the role of fiber in moderating the absorption of fructose and its impact on blood sugar.
Long-Term Health Implications
The differential effect of whole fruit and fruit juice on blood sugar levels has significant implications for long-term health. Rapid spikes in blood sugar can strain the body’s ability to produce enough insulin to regulate glucose levels effectively. Over time, this may lead to insulin resistance, an underlying factor in the development of type 2 diabetes.
Furthermore, the consumption of whole fruits provides additional health benefits beyond blood sugar regulation. Fruits are rich in vitamins, minerals, antioxidants, and other phytochemicals that contribute to overall well-being and the prevention of chronic diseases such as heart disease and certain cancers. By choosing whole fruits over fruit juice, individuals can harness the combined benefits of fiber and essential nutrients.
The Importance of Including Fiber in Every Meal
For individuals with diabetes following a ketogenic diet, it is crucial to include a source of fiber in every meal. Here are some reasons why:
Blood Sugar Regulation: Including fiber in each meal helps regulate blood sugar levels by slowing down the absorption of glucose. This can minimize the risk of blood sugar spikes and promote better overall glucose control.
Satiety and Weight Management: Fiber-rich foods are generally more filling and can contribute to a sense of satiety after a meal. This can aid in appetite management and weight control, which is particularly important for individuals with diabetes. Maintaining a healthy weight helps improve insulin sensitivity and supports blood sugar management.
Digestive Health: Fiber plays a vital role in maintaining a healthy digestive system. It adds bulk to the stool, promotes regular bowel movements, and helps prevent gastrointestinal issues such as constipation. This is particularly relevant for individuals with diabetes, as they are more prone to digestive complications.
How can you supplement fiber in your ketogenic diet without grains or carbs?
If you’re looking to supplement fiber in your diet without relying on grains or carbs, there are several options you can consider. Here are some fiber-rich foods that are low in grains and carbohydrates:
- Vegetables: Non-starchy vegetables like broccoli, cauliflower, Brussels sprouts, kale, spinach, and asparagus are excellent sources of fiber. You can include these in your meals and snacks.
- Berries: Berries such as raspberries, blackberries, and strawberries are relatively low in carbs and high in fiber. They can be consumed fresh or frozen and added to yogurt or smoothies.
- Chia seeds: Chia seeds are packed with fiber and can be easily incorporated into your diet. They can be added to smoothies, yogurt, or used as a topping for salads or oatmeal.
- Flaxseeds: Flaxseeds are another great source of fiber. You can sprinkle ground flaxseeds on your meals, add them to smoothies, or use them in baking recipes.
- Avocado: Avocado is a nutrient-dense fruit that is high in healthy fats and fiber. You can enjoy avocado as a topping, in salads, or as a guacamole dip.
- Nuts and seeds: Almonds, walnuts, and sunflower seeds are examples of nuts and seeds that provide both fiber and healthy fats. They can be eaten as a snack or added to various dishes.
- Legumes: While legumes like beans and lentils contain carbohydrates, they are also excellent sources of fiber and protein. Including moderate amounts of legumes in your diet can be beneficial.
- Psyllium husk: Psyllium husk is a fiber supplement derived from the seeds of the Plantago ovata plant. It is low in carbs and can be mixed with water or added to recipes as a thickening agent.
- Coconut: Coconut is rich in fiber and healthy fats. You can incorporate shredded coconut into your meals, use coconut flour for baking, or enjoy coconut milk in smoothies or curries.
- Cabbage: Cabbage is a low-carb vegetable that provides a good amount of fiber. You can use it in salads, stir-fries, or even make cabbage wraps instead of grain-based wraps.
- Mushrooms: Mushrooms are low in carbs and contain fiber. They can be used in a variety of dishes, such as stir-fries, soups, or stuffed mushroom caps.
- Cauliflower rice: Cauliflower can be grated or processed into rice-like grains, providing a low-carb alternative to traditional grains. You can use cauliflower rice as a base for stir-fries, salads, or side dishes.
- Seaweed: Various types of seaweed, such as nori or kelp, are low in carbs and high in fiber. You can enjoy them in sushi rolls, salads, or as a crunchy snack.
- Artichokes: Artichokes are a good source of fiber and can be enjoyed steamed, grilled, or added to dips like spinach artichoke dip.
- Green leafy vegetables: Leafy greens like spinach, Swiss chard, and kale are low in carbs and rich in fiber. They can be used in salads, smoothies, or sautéed as a side dish.
Consulting a Healthcare Professional
It is crucial to consult with a healthcare professional or registered dietitian experienced in diabetes management before making any significant changes to your diet, especially if you have diabetes. They can provide personalized guidance based on your specific needs and help you create a well-balanced meal plan that incorporates fiber-rich foods while adhering to a ketogenic approach.
Conclusion
Incorporating fiber into a ketogenic diet is essential for individuals with Type 1 or Type 2 diabetes aiming to maintain stable blood sugar levels. Scientific studies have consistently demonstrated the positive impact of fiber on glycemic control and blood sugar management. By prioritizing fiber-rich foods such as non-starchy vegetables, berries, seeds, and nuts, individuals with diabetes can enhance their overall dietary fiber intake while adhering to a ketogenic eating pattern. By doing so, they can work towards better blood sugar control and improved long-term health outcomes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unraveling the Dawn Phenomenon: Understanding Gluconeogenesis in Type 1 Diabetes
By Stephen Fitzmeyer, MD
Introduction:
The dawn phenomenon is a well-known phenomenon observed in individuals with type 1 diabetes, characterized by an abnormal rise in blood glucose levels during the early morning hours, even in the absence of food intake. It has been a subject of scientific curiosity and investigation for many years. While the exact cause of the dawn phenomenon remains unclear, one hypothesis suggests that overactive gluconeogenesis may play a significant role in its manifestation. In this article, we delve into the relationship between the dawn phenomenon and gluconeogenesis in type 1 diabetes to shed light on this intriguing phenomenon.
Understanding the Dawn Phenomenon:
To comprehend the dawn phenomenon, it is essential to grasp the concept of gluconeogenesis. Gluconeogenesis is a natural process in which the liver produces glucose from non-carbohydrate sources, such as amino acids and glycerol. This metabolic pathway is crucial in maintaining blood glucose levels during periods of fasting or prolonged exercise.
In individuals with type 1 diabetes, who lack insulin production, the dawn phenomenon is believed to occur due to the combined effect of several factors. During the late night and early morning hours, hormones such as cortisol, growth hormone, and glucagon are released in higher amounts. These hormones work together to increase insulin resistance and stimulate hepatic gluconeogenesis. The elevated blood glucose levels observed in the morning are thought to be a consequence of these hormonal changes.
Role of Gluconeogenesis in the Dawn Phenomenon:
Gluconeogenesis is regulated by a complex interplay of hormonal and metabolic factors. Under normal circumstances, insulin suppresses gluconeogenesis, primarily by inhibiting the release of glucagon and promoting glucose uptake in peripheral tissues. However, in type 1 diabetes, the absence of insulin disrupts this balance, resulting in uncontrolled gluconeogenesis.
Research has suggested that the dawn phenomenon may be associated with overactive gluconeogenesis. Studies have shown increased levels of hepatic glucose production during the early morning hours in individuals with type 1 diabetes experiencing the dawn phenomenon. This excessive glucose production can contribute to the elevated blood glucose levels observed upon waking.
Alternative Factors:
While overactive gluconeogenesis is one plausible explanation for the dawn phenomenon, it is important to note that other factors may also contribute to its occurrence. The release of counterregulatory hormones, such as cortisol and growth hormone, may promote hepatic glucose output, leading to increased blood glucose levels. Additionally, alterations in circadian rhythms and overnight hypoglycemia followed by a rebound effect might also contribute to the dawn phenomenon.
Clinical Implications:
Understanding the mechanisms underlying the dawn phenomenon is crucial for effective diabetes management. Several strategies can help mitigate its impact. Adjusting insulin regimens, particularly by optimizing basal insulin doses during the early morning hours, can help counteract the excessive hepatic glucose production. Additionally, lifestyle modifications such as regular exercise, a balanced diet, and adequate sleep may aid in maintaining stable blood glucose levels.
Conclusion:
While the dawn phenomenon in individuals with type 1 diabetes remains a subject of ongoing research, overactive gluconeogenesis appears to be one of the contributing factors. The hormonal changes that occur during the early morning hours, coupled with the absence of insulin, disrupt the delicate balance of glucose regulation. Further research is needed to unravel the intricate mechanisms involved in the dawn phenomenon fully. By gaining a deeper understanding of this phenomenon, healthcare professionals can develop more effective strategies to manage blood glucose levels and improve the overall well-being of individuals living with type 1 diabetes.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/