- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Blog
Follow our blog and stay up to date.
The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
Healthcare is at a pivotal moment in history, where technological innovation is redefining how care is delivered, managed, and optimized. At the core of this revolution are Artificial Intelligence (AI), Clinical Informatics, and Machine Learning (ML), fields that intersect to create a paradigm shift in the way we approach health and wellness. This confluence has the potential to enhance decision-making, streamline operations, and improve patient outcomes.
1. Transforming Healthcare Through
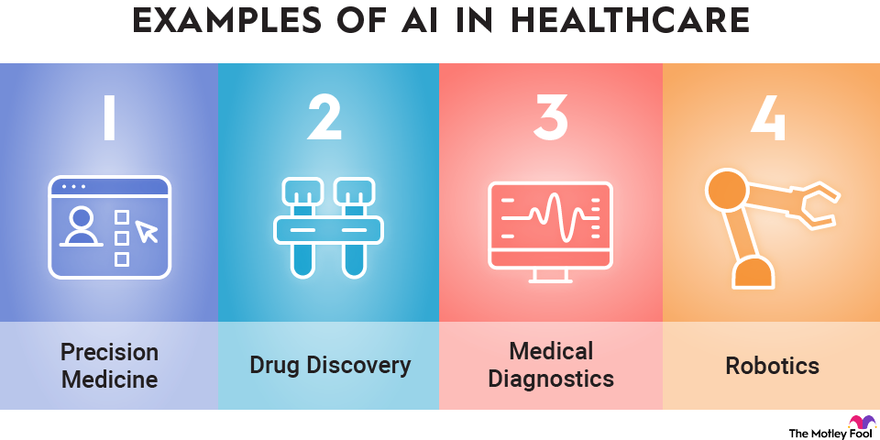
AI brings an unprecedented ability to process and analyze large datasets with speed and accuracy that no human could match. In healthcare, AI is being applied to areas such as:
- Predictive Analytics: AI algorithms can predict patient outcomes based on historical data, enabling proactive intervention. For example, models trained on electronic health record (EHR) data can forecast hospital readmissions or identify patients at risk for chronic diseases.
- Medical Imaging: AI-powered tools can analyze X-rays, MRIs, and CT scans, often detecting anomalies with greater precision than human radiologists.
- Personalized Medicine: AI tailors treatment plans by analyzing genetic, lifestyle, and environmental factors. This ensures therapies are as effective as possible for individual patients.
2. The Role of Clinical Informatics
Clinical Informatics is the backbone of data-driven decision-making in healthcare. It focuses on the optimal use of information and technology to improve patient care and health outcomes. Informatics integrates with AI and ML in several ways:
- Data Integration: Informatics ensures the seamless aggregation and harmonization of diverse healthcare data sources, from EHRs to wearable devices.
- Interoperability: The field promotes standards and protocols that allow AI systems to access and utilize data across different platforms and institutions.
- Clinical Decision Support Systems (CDSS): Informatics integrates AI-driven insights into clinician workflows, enabling smarter, faster, and more accurate decisions at the point of care.
3. Machine Learning as the Engine of Innovation
Machine Learning, a subset of AI, excels at identifying patterns in data and making predictions. In healthcare, ML applications are advancing at a rapid pace:
- Drug Discovery: ML accelerates drug development by predicting how compounds interact with biological systems, reducing the time and cost of bringing new medications to market.
- Operational Efficiency: Hospitals are using ML to optimize staffing, predict supply needs, and improve resource allocation, reducing waste and enhancing patient experiences.
- Natural Language Processing (NLP): ML-powered NLP systems analyze unstructured clinical notes, turning them into actionable insights. This has implications for billing, compliance, and clinical documentation.
4. Ethical and Practical Considerations
While the potential of AI, ML, and Clinical Informatics in healthcare is vast, it is not without challenges:
- Data Privacy and Security: With vast amounts of sensitive health data being processed, ensuring robust cybersecurity measures is critical.
- Bias in Algorithms: AI systems trained on biased datasets can perpetuate disparities in care. Diverse data representation is essential to mitigate this risk.
- Clinician Adoption: Integrating AI tools into clinical practice requires buy-in from healthcare professionals. These tools must be user-friendly and provide clear, actionable insights.
5. The Future of Healthcare
The intersection of AI, Clinical Informatics, and ML is laying the groundwork for a healthcare system that is:
- More Predictive: By identifying health issues before they become critical, we can move from reactive to preventive care.
- More Personalized: Treatments will be increasingly tailored to the unique characteristics of each patient.
- More Efficient: Automation of administrative tasks will allow clinicians to focus more on patient care.
Conclusion
The synergy between AI, Clinical Informatics, and Machine Learning is transforming healthcare into a smarter, more adaptive system. These technologies are not merely tools but catalysts for innovation, enabling a future where healthcare is not only more efficient but also more human.
As we navigate this new frontier, the focus must remain on ensuring ethical implementation, fostering trust among stakeholders, and keeping the patient at the center of every innovation.
Accessing Siloed EMR Systems with FHIR: Connecting to Multiple EMRs
In today’s healthcare landscape, the ability to connect to multiple EMRs (Electronic Medical Records) seamlessly has become crucial for improving patient care, reducing administrative overhead, and driving innovation. However, the diversity in EMR systems, proprietary data formats, and communication protocols has historically made integration a daunting challenge. Enter FHIR (Fast Healthcare Interoperability Resources), the game-changing standard developed by HL7 (Health Level Seven International), which is paving the way for interoperability in healthcare.
The Problem: Siloed EMR Systems
Healthcare providers often use different EMR systems, each designed with unique data structures, interfaces, and workflows. While these systems are essential for managing patient information, they don’t “talk” to each other natively. This lack of interoperability creates data silos, leading to:
- Inefficiencies: Manual data entry and reconciliation slow down workflows.
- Fragmented Care: Providers may not have access to a complete patient history.
- Missed Opportunities: Innovations like patient-facing apps and decision-support tools struggle to integrate across multiple platforms.
The Solution: FHIR as a Universal Language
FHIR offers a standardized framework for accessing and exchanging healthcare information. By leveraging its RESTful API architecture and well-defined data models (resources), FHIR enables seamless integration across multiple EMRs. Here’s how:
- Unified Data Access via FHIR APIs Modern EMR systems like Epic, Cerner, and Allscripts have adopted FHIR APIs as part of their platforms. This standardization allows external applications to retrieve and interact with data like patient demographics, medications, and lab results without requiring custom integration for each EMR.
- Standardized Resources FHIR resources—such as Patient, Observation, Encounter, and Medication—act as reusable data models. These resources provide a consistent structure across systems, making it easier for developers to query and update data in a predictable way, regardless of the underlying EMR.
- SMART on FHIR for Authentication The SMART on FHIR framework adds an additional layer by standardizing the way apps authenticate and gain authorized access to EMR data using OAuth 2.0. This ensures secure, scalable integration while respecting patient privacy and data security regulations like HIPAA.
Benefits of Connecting to Multiple EMRs
- Streamlined Care Coordination FHIR enables providers to access and share patient data across different healthcare systems. A specialist in one hospital can view relevant records from another provider’s EMR, ensuring continuity of care.
- Simplified Integration for Developers Developers can create third-party applications, such as telehealth platforms or chronic disease management tools, that work with multiple EMRs out of the box. Instead of writing custom connectors for each system, developers interact with a single FHIR-based API.
- Empowering Patients Patient-facing apps can use FHIR to aggregate data from multiple EMRs, giving individuals a unified view of their health records. This transparency improves patient engagement and health outcomes.
- Faster Innovation The reduced complexity of integrating with EMRs allows startups and innovators to focus on building features that directly improve care delivery rather than wrestling with legacy integration challenges.
Challenges to Consider
While FHIR greatly simplifies the process of connecting to multiple EMRs, it’s not without challenges:
- Vendor Variability: Not all EMRs implement FHIR in the same way. Developers may encounter slight differences in API behavior across systems.
- Data Gaps: Older EMRs or smaller providers might not support FHIR, requiring fallback mechanisms.
- Access Control: Even with FHIR, gaining authorized access to data involves navigating organizational policies and regulatory requirements.
The Future of EMR Connectivity
As FHIR adoption continues to grow, the dream of a truly interoperable healthcare ecosystem is becoming a reality. Initiatives like the 21st Century Cures Act in the United States mandate that EMR vendors provide FHIR APIs to improve data access and patient empowerment. This regulatory push, combined with advancements in technology, means that healthcare organizations can now leverage FHIR to unlock the full potential of their data.
Conclusion
Connecting to multiple EMRs is no longer an insurmountable challenge. With FHIR as the universal standard, healthcare providers, developers, and patients can break down data silos, enabling seamless information exchange and fostering innovation. Whether you’re building a new application or improving workflows in your organization, FHIR offers the tools to bridge the gaps between EMRs and create a more connected healthcare future.
How AI Can Transform Healthcare Applications
How AI Can Transform Healthcare Applications
As a developer of healthcare applications, you’re constantly looking for ways to improve functionality, efficiency, and user experience. Artificial Intelligence (AI) offers a transformative opportunity to enhance healthcare apps, making them smarter, more user-friendly, and impactful. Here’s how AI can elevate your healthcare applications to the next level.
1. Enhancing Patient Care and Management
- Personalized Treatment Recommendations: AI algorithms analyze patient data like lab results, genetic information, and medical history to suggest tailored treatment plans.
- Virtual Assistants: Chatbots powered by natural language processing (NLP) can answer common patient questions, help schedule appointments, and remind patients about medications.
- Predictive Analytics: AI models predict potential health issues, such as diabetes or cardiovascular disease, allowing for early intervention and better patient outcomes.
2. Supporting Clinical Decision-Making
- AI Diagnosis Tools: Machine learning can analyze medical images, lab tests, or patient-reported symptoms to help identify conditions quickly and accurately.
- Drug Interaction Alerts: AI systems can flag potential drug interactions or contraindications based on a patient’s medication history.
- Risk Assessment Models: Predictive models assess patient risks for conditions like stroke or sepsis, enabling proactive care.
3. Optimizing Workflow
- Automated Documentation: NLP tools transcribe and summarize doctor-patient conversations, reducing administrative burdens.
- Intelligent Scheduling: AI-powered tools optimize staff and appointment scheduling, minimizing wait times and maximizing resource utilization.
- Claims Automation: Automate insurance claim reviews with AI, reducing errors and speeding up reimbursement processes.
4. Enhancing Telemedicine and Remote Monitoring
- AI Diagnostics: Enhance telehealth platforms with tools that analyze patient-reported data or uploaded images during virtual consultations.
- Wearable Data Integration: Develop AI algorithms to process data from wearables, offering actionable insights into patient health.
- Symptom Checkers: AI-driven tools allow patients to input symptoms and receive preliminary assessments, streamlining triage.
5. Delivering Data Insights and Analytics
- Patient Cohort Analysis: AI identifies patterns in patient populations, improving treatment strategies and research.
- Health Trend Forecasting: Analyze big data to predict public health trends or disease outbreaks.
- Operational Efficiency: Use AI to optimize inventory, staffing, and resource allocation in clinical settings.
6. Improving Patient Engagement
- Conversational Interfaces: Enable patients to interact with your app through natural language queries, making healthcare more accessible.
- Gamification: Use AI to personalize gamified elements, encouraging adherence to treatment plans or healthy behaviors.
- Educational Content: Deliver tailored educational materials based on a patient’s condition or interests.
7. Ensuring Compliance and Security
- Data Anonymization: AI can de-identify sensitive patient data for compliance with regulations like HIPAA and GDPR.
- Fraud Detection: AI detects anomalies in billing or prescriptions that may indicate fraud.
- Secure Data Sharing: Facilitate secure and efficient sharing of patient records among healthcare providers.
8. Facilitating Research and Development
- Clinical Trial Matching: Match eligible patients to clinical trials using AI-driven analysis of their medical profiles.
- Drug Discovery: Use AI models to simulate and analyze potential drug compounds.
- Real-World Evidence: Generate insights from patient data to support post-market surveillance and drug efficacy studies.
9. Expanding Accessibility
- Language Translation: Offer multilingual support for diverse patient populations with AI translation tools.
- Accessibility Features: Build AI-driven speech-to-text and text-to-speech features for patients with disabilities.
10. Elevating User Experience
- Predictive Navigation: Anticipate user actions to streamline navigation and improve usability.
- Behavioral Nudges: Deliver proactive reminders or nudges, such as medication adherence prompts, based on user behavior.
- Dynamic Interfaces: Personalize app interfaces based on user preferences and engagement patterns.
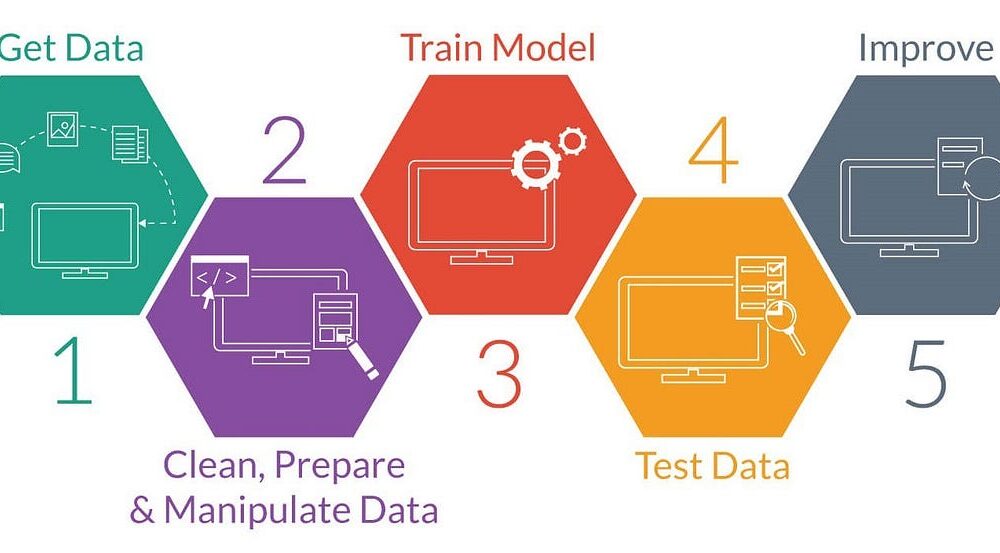
Example: Implementing an AI-Powered Symptom Checker
Here’s an example of how you might structure an app to include a symptom checker using AI:
- Input Collection: The app asks users to input symptoms via text or voice.
- Natural Language Processing (NLP): AI processes the input to extract relevant medical terms and symptoms.
- Symptom Analysis: The app uses a machine learning model trained on a medical dataset to compare the user’s symptoms with known patterns of illnesses.
- Recommendation Engine: Based on the analysis, the app provides possible conditions and suggests whether the user should seek immediate care, consult a doctor, or try home remedies.
- Continuous Learning: The app collects anonymized feedback from user interactions to improve the accuracy of the model over time.
Example Code for NLP Symptom Processing:
from transformers import pipeline
# Load a pre-trained NLP model for healthcare applications
nlp_model = pipeline("text-classification", model="bert-base-healthcare")
# Example user input
user_input = "I have a persistent cough and shortness of breath."
# Process the input
analysis = nlp_model(user_input)
# Output AI-generated insights
print("Potential conditions:", analysis)
This code snippet demonstrates how to use a pre-trained NLP (Natural Language Processing) model from the Hugging Face transformers library to classify text related to healthcare applications. Here’s a breakdown of what each part of the code does:
1. Importing pipeline from the transformers library
from transformers import pipelineThe pipeline function provides an easy interface to use pre-trained models for various NLP tasks like text classification, question answering, translation, etc.
2. Loading a Pre-trained NLP Model
nlp_model = pipeline("text-classification", model="bert-base-healthcare")pipeline("text-classification"): This specifies that the task is text classification, where input text will be categorized into predefined classes or labels.model="bert-base-healthcare": Refers to a pre-trained BERT (Bidirectional Encoder Representations from Transformers) model fine-tuned for healthcare-related text classification. This specific model would likely be trained to understand healthcare vocabulary and contexts.
3. Processing User Input
user_input = "I have a persistent cough and shortness of breath."
analysis = nlp_model(user_input)The pipeline processes the input text using the loaded model to predict potential conditions or categories related to the input.
4. Outputting Results
print("Potential conditions:", analysis)The analysis variable contains the model’s predictions, such as potential health conditions or relevant categories for the provided symptoms.
Example Output
Potential conditions: [{'label': 'Respiratory Issue', 'score': 0.95}]- label: The predicted category (e.g., “Respiratory Issue”).
- score: The confidence score for this prediction (e.g., 0.95, indicating 95% confidence).
Use Case
This code can be part of a healthcare chatbot, clinical decision support system, or any application designed to provide preliminary insights based on patient symptoms. However, these AI-generated insights should not replace professional medical advice.
Getting Started with AI Integration
To start incorporating AI into your healthcare applications:
- Start Small: Begin with a single AI feature, such as a chatbot or predictive analytics, to test feasibility and user acceptance.
- Prioritize Data Quality: Ensure clean, accurate data to power your AI models effectively.
- Focus on Ethics: Build trust by maintaining transparency, privacy, and fairness in AI algorithms.
- Iterate and Scale: Use feedback to refine AI functionalities and expand capabilities over time.
AI is reshaping healthcare, offering exciting opportunities to create more impactful applications. By leveraging AI, you can provide better care, improve efficiency, and drive innovation in healthcare technology.
Protecting and Repairing the Glycocalyx: The Key to Vascular Health
Title: Protecting and Repairing the Glycocalyx: The Key to Vascular Health
In recent years, the glycocalyx has gained attention in the health and wellness world, especially for its crucial role in vascular health. This thin, gel-like layer on the surface of cells, particularly on the endothelial cells lining our blood vessels, plays a vital role in keeping our blood vessels healthy and free from dangerous plaques. But what exactly is the glycocalyx, how does it get damaged, and, importantly, how can we repair it? Let’s dive into the science and strategies behind protecting this vital structure.
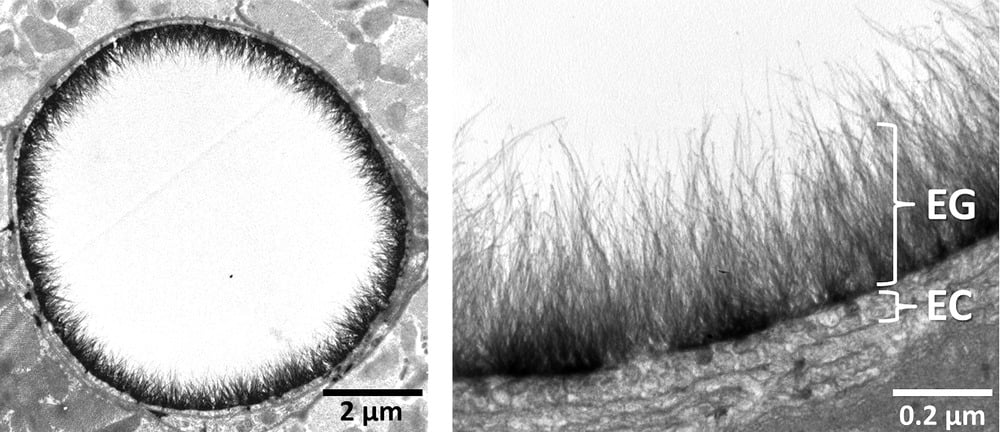
What Is the Glycocalyx?
The glycocalyx is a delicate, sugar-rich coating found on the surface of many cells. It’s particularly abundant on endothelial cells, which form the inner lining of blood vessels. Made of glycoproteins, glycolipids, and proteoglycans, the glycocalyx serves as a protective shield, helping to:
- Maintain smooth blood flow by reducing friction.
- Prevent blood cells and harmful substances like oxidized LDL (low-density lipoprotein) from sticking to vessel walls.
- Act as a barrier against pathogens.
- Enable cellular communication through various signaling molecules.
The glycocalyx is essentially the first line of defense for our blood vessels, safeguarding them from inflammation and damage. However, modern lifestyle factors can lead to glycocalyx damage, contributing to vascular diseases such as atherosclerosis.
How Does Glycocalyx Damage Lead to Plaque Buildup?
When the glycocalyx is damaged, it loses its integrity, making it easier for harmful molecules like oxidized LDL cholesterol to interact with the endothelial cells underneath. This damage can trigger an inflammatory response in the vessel wall, which can initiate plaque formation. Over time, as plaque builds up, it can restrict blood flow, leading to conditions like heart attacks, strokes, and other cardiovascular issues.
The Impact of High Blood Sugar and Fats on the Glycocalyx
Chronic high blood sugar, often seen in diabetes, and certain types of fats can contribute to glycocalyx damage. Here’s how:
- Oxidative Stress from Hyperglycemia:
- When blood sugar levels remain high, they trigger an overproduction of reactive oxygen species (ROS) in the endothelial cells. These molecules are highly reactive and can damage cellular structures, including the glycocalyx, by breaking down its carbohydrate components.
- Inflammation and Glycation:
- High blood sugar leads to the formation of advanced glycation end products (AGEs), which occur when glucose molecules bind to proteins and fats. These AGEs accumulate in blood vessels, directly interacting with and damaging the glycocalyx. They also activate receptors (RAGE) on endothelial cells, triggering inflammation and further degrading the glycocalyx.
- Excessive Omega-6 Intake and Inflammation:
- A high intake of omega-6 fatty acids, often from seed oils like soybean, corn, and sunflower oils, can shift the body toward a pro-inflammatory state. This imbalance between omega-6 and omega-3 fatty acids can increase inflammation that directly harms the glycocalyx.
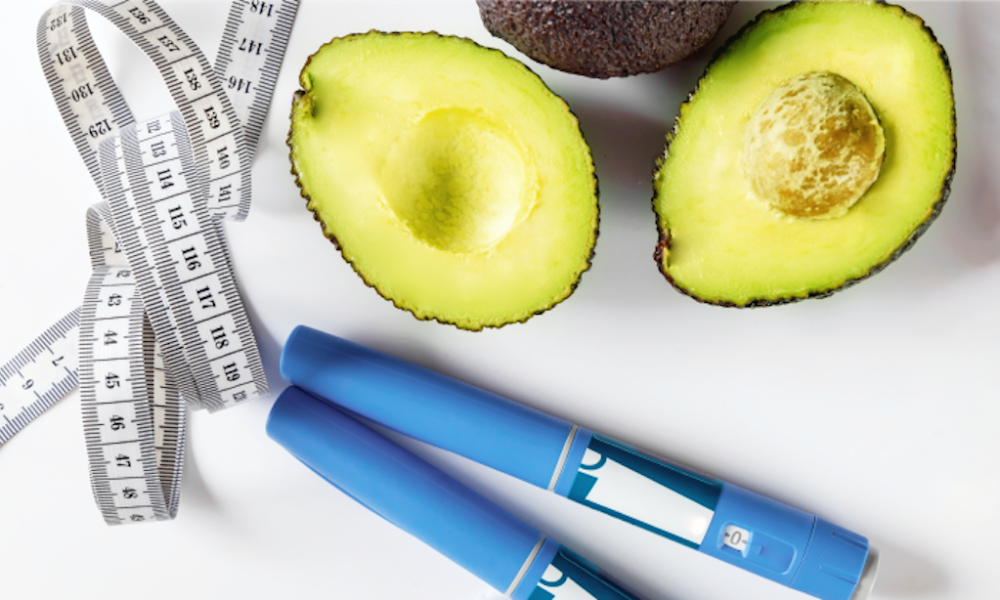
- By creating an inflammatory response, omega-6 fatty acids contribute to oxidative stress and enzymatic activity that breaks down glycocalyx components. Replacing seed oils with anti-inflammatory fats, such as those found in olive oil, avocado oil, and fatty fish, can help protect the glycocalyx by reducing these inflammatory triggers.
- Enzymatic Degradation:
- Hyperglycemia and oxidative stress stimulate enzymes like heparanase and hyaluronidase, which break down the glycocalyx components such as heparan sulfate and hyaluronic acid, causing it to thin.
When the glycocalyx is compromised, the blood vessel becomes more permeable to cholesterol and other inflammatory molecules, leading to plaque buildup and increased cardiovascular risk.
The Role of Remnant Cholesterol and TG/HDL Ratios in Glycocalyx Assessment
For primary care providers (PCPs) and general practitioners (GPs), calculating a patient’s Remnant Cholesterol and Triglyceride-to-HDL (TG/HDL) ratio can provide a quick, valuable assessment of cardiovascular risk and potential glycocalyx damage. These indicators offer insight into lipid metabolism and inflammation, both of which affect the glycocalyx.
- Remnant Cholesterol: Calculated as total cholesterol minus LDL and HDL cholesterol, remnant cholesterol reflects the amount of triglyceride-rich lipoproteins. High levels are associated with increased risk of atherosclerosis and glycocalyx degradation, as these remnant particles can penetrate the endothelium and contribute to plaque formation.
- TG/HDL Ratio: The TG/HDL ratio is an easy-to-calculate marker of insulin resistance and metabolic health. High TG and low HDL levels often correlate with higher oxidative stress and systemic inflammation, both of which damage the glycocalyx. A TG/HDL ratio above 3.0 can indicate increased cardiovascular risk and a compromised glycocalyx.
Incorporating these markers into regular check-ups can help PCPs and GPs identify patients with higher glycocalyx damage risk, guiding preventive measures such as dietary adjustments, lifestyle changes, and early intervention.
Can the Glycocalyx Be Repaired?
The good news is that, while fragile, the glycocalyx can be repaired and maintained with the right dietary, lifestyle, and medical interventions. Here are some of the most effective strategies:
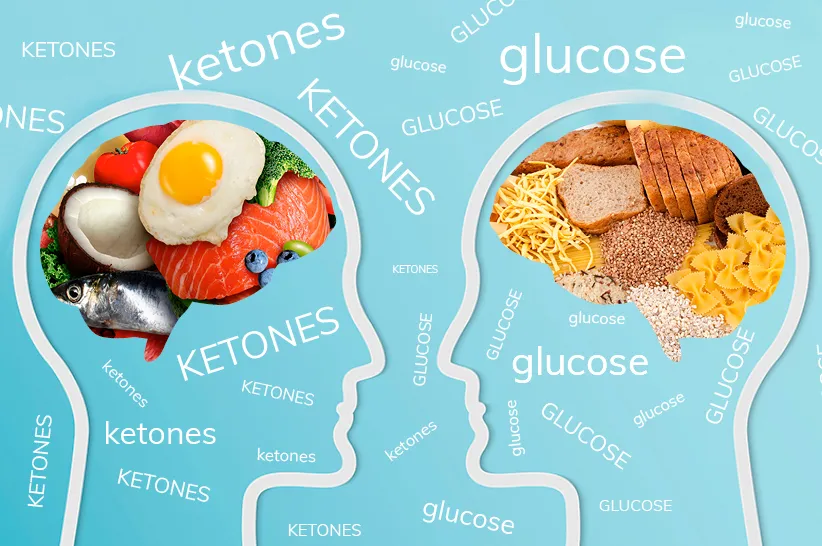
1. Control Blood Sugar Levels
- Dietary Changes: Reducing refined carbohydrates and sugars is essential for maintaining blood sugar levels. A diet focused on whole, unprocessed foods with a low glycemic index can minimize blood sugar spikes and the resulting oxidative stress.
- Exercise: Physical activity improves insulin sensitivity, helping regulate blood glucose and reduce glycocalyx damage from hyperglycemia.
- Medications: For individuals with diabetes, medications like metformin can help keep blood glucose within a healthy range, reducing the risk of glycocalyx damage.
2. Boost Antioxidants
- Vitamin C and E: These antioxidants help neutralize ROS, protecting the glycocalyx from oxidative damage.
- Polyphenols: Found in foods like berries, green tea, and dark chocolate, polyphenols have anti-inflammatory properties and protect the glycocalyx from ROS. Resveratrol, a specific polyphenol in red wine, is known for supporting vascular health and glycocalyx repair.
- Omega-3 Fatty Acids: Known for their anti-inflammatory effects, omega-3s (found in fatty fish and fish oil supplements) help reduce inflammation and protect the glycocalyx from enzymatic degradation. They also help stabilize the endothelial cells, reducing breakdown of glycocalyx components.
3. Support Glycocalyx Health with Key Nutrients
- L-arginine: This amino acid boosts nitric oxide production, which improves endothelial function and supports glycocalyx repair.
- Hyaluronic Acid and Chondroitin Sulfate: These are essential building blocks of the glycocalyx, often found in joint supplements. They support glycocalyx structure and help it retain moisture, keeping it intact and functional.
- Sulfur-Rich Foods: Garlic, onions, and cruciferous vegetables contain sulfur, which supports the synthesis of glycosaminoglycans, vital components of the glycocalyx.
4. Adopt a Low-Carb Lifestyle and Eliminate Inflammatory Foods
A low-carb lifestyle, with the elimination of seed oils, grains, and sugars, is especially beneficial for glycocalyx health:
- Reduced Blood Sugar Spikes: Limiting carbohydrate intake stabilizes blood sugar, preventing the oxidative stress associated with high blood glucose. This lowers the formation of AGEs and reduces direct damage to the glycocalyx.
- Improved Insulin Sensitivity: A low-carb approach, often combined with exercise, enhances insulin sensitivity, allowing cells to better utilize glucose, thereby keeping blood sugar stable and minimizing glycocalyx damage.
- Eliminating Seed Oils: Seed oils, high in omega-6 fatty acids, are inflammatory when consumed in excess. By replacing these oils with healthy fats (like olive oil, avocado oil, and butter), inflammation can be reduced, preserving glycocalyx health.
- Removing Grains and Sugars: High-glycemic grains and sugars contribute to glycation, leading to AGEs that harm the glycocalyx. Focusing on nutrient-dense vegetables and quality proteins provides energy without causing the blood sugar spikes that damage vascular health.
5. Avoid Harmful Substances
- Reduce Inflammatory Fats: Trans fats and excessive omega-6 fats (commonly found in processed seed oils) contribute to inflammation that damages the glycocalyx. Focusing on anti-inflammatory fats like olive oil, avocado oil, and omega-3-rich foods can support vascular health.
- Limit Smoking and Alcohol: Both smoking and excessive alcohol increase oxidative stress and inflammation, damaging the glycocalyx. Avoiding these substances is key for vascular and overall health.
6. Explore Emerging Therapies and Supplements
- Glycocalyx-Targeted Supplements: Some supplements aim to support glycocalyx health directly with compounds like glycosaminoglycans, which are essential to its structure. These “endocalyx” supplements may help repair and strengthen the glycocalyx.
- Stem Cell and Regenerative Therapies: Though still in experimental stages, stem cell and regenerative therapies hold promise for repairing damaged glycocalyx in severe cases.
- Nitric Oxide (NO) Enhancing Therapies: Therapies that boost NO production in the endothelium are being researched for their potential to help restore glycocalyx health and improve overall vascular function.
The Path Forward for Glycocalyx Health
Protecting and repairing the glycocalyx is crucial for maintaining vascular health and preventing the progression of plaque buildup. By focusing on blood sugar control, boosting antioxidants, incorporating essential nutrients, and utilizing key indicators like Remnant Cholesterol and TG/HDL ratios, we can help assess, repair, and protect this delicate structure to support cardiovascular wellness. A low-carb lifestyle, especially one that excludes seed oils, grains, and sugars, provides even greater protection, creating conditions that allow the glycocalyx to repair and thrive.
As research continues, our understanding of the glycocalyx and its role in health will expand, unlocking even more ways to protect this remarkable structure and the vital functions it supports. By nurturing the glycocalyx, we’re investing in the foundation of our cardiovascular health, giving us a powerful tool for longevity and well-being.
Unveiling the Mysteries of Epidemiology: The Backbone of Medicine
Introduction
In the vast realm of medicine, epidemiology stands as an unsung hero – the silent sentinel that plays a pivotal role in preventing, controlling, and understanding diseases. While this field may not garner the same attention as groundbreaking medical discoveries, it is the backbone that supports the entire healthcare system. In this article, we delve into the fascinating world of epidemiology, shedding light on what it is, why it matters, and how it shapes the practice of medicine.
What is Epidemiology?
Epidemiology is often described as the science of public health. It is the study of how diseases spread and impact populations, and it seeks to understand the patterns, causes, and consequences of health and disease in human communities. This field employs a variety of research methods to investigate the distribution and determinants of health-related outcomes, with the ultimate goal of improving public health.
Why Does Epidemiology Matter in Medicine?
Disease Prevention and Control:
Epidemiology plays a pivotal role in preventing and controlling diseases. By identifying risk factors, understanding the transmission of diseases, and evaluating interventions, epidemiologists help develop strategies to mitigate the impact of illnesses.
Public Health Policy:
Policymakers rely on epidemiological data to make informed decisions. This information helps shape public health policies, such as vaccination programs, smoking bans, and disaster preparedness, to protect and improve public health.
Outbreak Investigations:
During disease outbreaks, epidemiologists are the first responders. They conduct field investigations to identify the source of the outbreak, understand its transmission, and implement measures to contain it.
Research and Innovation:
Epidemiological studies provide the foundation for medical research. They generate hypotheses, drive clinical trials, and lead to the development of new treatments and therapies.
Key Concepts in Epidemiology
Incidence and Prevalence:
Incidence measures the rate of new cases of a disease within a specific time frame and population. Prevalence, on the other hand, reflects the total number of cases within a population at a given time. These metrics are essential for understanding the burden of diseases.
Risk Factors:
Identifying risk factors, such as genetics, lifestyle choices, and environmental exposures, is crucial in preventing diseases. Epidemiologists help pinpoint these factors, allowing for targeted interventions.
Cohort Studies and Case-Control Studies:
Cohort studies follow a group of individuals over time to assess the development of diseases, while case-control studies compare those with a specific condition to those without it. Both study designs help unravel the causes of diseases.
Outbreak Investigations:
During outbreaks, epidemiologists work swiftly to trace the origins of the disease, identify its transmission patterns, and implement control measures to limit its spread.
Surveillance Systems:
Epidemiologists use surveillance systems to monitor diseases on an ongoing basis. These systems enable early detection of outbreaks, providing a chance for swift intervention.
Challenges in Epidemiology
Epidemiology is not without its challenges. The field faces obstacles such as the difficulty of establishing causation, the ethical concerns surrounding experiments on human populations, and the evolving nature of diseases. With the rise of emerging infectious diseases and the increasing globalization of health threats, epidemiologists must adapt to new challenges continuously.
Conclusion
Epidemiology is the silent force that ensures the well-being of societies by enabling the prevention and control of diseases. In the practice of medicine, this field provides the essential knowledge and tools to understand the spread of illnesses, identify risk factors, and develop effective strategies for disease prevention and treatment. As medicine and healthcare evolve, epidemiology will remain a steadfast ally, contributing to the health and longevity of humanity. It is the unsung hero that keeps us safe, vigilant, and prepared for the health challenges of the future.