- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Global Health
Intermittent Fasting: The Key to Metabolic Health, Empowered by the Ketogenic Diet for Satiety, Hunger Reduction, and Craving Control
By Stephen Fitzmeyer, MD
Introduction
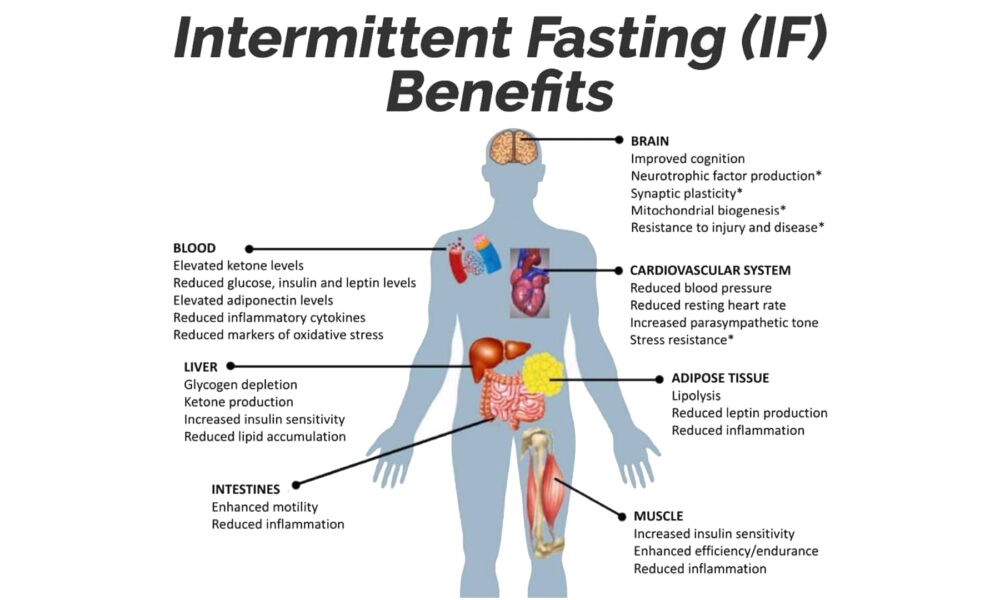
In the realm of metabolic health, one strategy has risen above the rest: Intermittent Fasting (IF). When coupled with the Ketogenic (Keto) diet, IF becomes an unrivaled approach that unlocks the full potential of satiety, hunger reduction, and cravings control. By harnessing the power of fasting, IF paves the way for optimal metabolic function, while the Keto diet amplifies these benefits, leading to improved overall health and well-being.
Intermittent Fasting: A Metabolic Game Changer
Intermittent Fasting has garnered widespread acclaim due to its profound impact on metabolic health. Rather than focusing solely on what you eat, IF centers on when you eat, establishing periods of fasting interspersed with designated eating windows.
At the core of IF lies its ability to promote metabolic flexibility. By depriving your body of constant food intake, it becomes adept at tapping into stored fat as an alternative energy source. This metabolic switch leads to weight loss, increased insulin sensitivity, and reduced inflammation.
Satiety and Hunger Reduction: The Role of IF
One of the key advantages of IF is its capacity to enhance satiety and curb hunger. During fasting periods, your body turns to its fat stores for fuel, facilitating fat burning and weight loss. However, the benefits extend far beyond shedding pounds.
IF effectively regulates hunger and fullness hormones, such as ghrelin and leptin, which influence appetite. With consistent practice, these hormones rebalance, resulting in reduced hunger and decreased cravings. By allowing your body ample time between meals, IF equips you with a newfound sense of control over your eating habits.
The Power of the Ketogenic Diet
Enter the Ketogenic diet, a low-carbohydrate, high-fat approach that synergizes remarkably with IF. By drastically reducing carbohydrate intake and increasing healthy fat consumption, the Keto diet promotes nutritional ketosis—a metabolic state where your body primarily relies on fat for energy.
The Keto diet is a satiety powerhouse. Healthy fats take longer to digest, keeping you feeling full and satisfied for extended periods. This phenomenon effectively curbs hunger, reduces cravings, and prevents the energy crashes associated with high-carbohydrate diets.
IF and Keto: The Dynamic Duo for Metabolic Health
When Intermittent Fasting and the Ketogenic diet join forces, a metabolic transformation occurs. IF acts as the catalyst, priming your body for efficient fat burning, while the Keto diet ensures that fat becomes the primary fuel source.
By following a Ketogenic diet within your designated eating window, you not only maintain a state of ketosis but also heighten the feeling of satiety. The combined approach effectively reduces hunger and cravings, making it easier to adhere to your dietary goals and achieve optimal metabolic health.
Conclusion
Intermittent Fasting is the key to unlocking metabolic health, and when paired with the Ketogenic diet, it becomes an unbeatable strategy for satiety, hunger reduction, and craving control. IF enhances your body’s ability to tap into stored fat for energy and regulates hunger hormones, while the Keto diet amplifies these effects through increased fat consumption.
Embrace Intermittent Fasting as your metabolic ally and leverage the Ketogenic diet as the perfect complement. Together, they offer a path to sustainable weight loss, improved insulin sensitivity, and enhanced overall well-being. Experience the transformative power of IF and Keto, and embrace a life of metabolic vitality.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
From Cholera to COVID-19: The Role of Epidemiology in Disease Outbreaks
By Stephen Fitzmeyer, MD
The cholera outbreak in 1854 in London, and the work of John Snow, is considered a turning point in the field of epidemiology. The outbreak caused thousands of deaths and was traced back to contaminated water from the Broad Street pump. Snow’s investigation led him to identify the source of the outbreak, and he subsequently recommended measures to prevent the spread of cholera.
Fast forward to modern times, and we are facing a new epidemic – COVID-19. The similarities between the two outbreaks are striking, and so are the differences. Like cholera, COVID-19 is a highly contagious disease that spreads through contact with infected individuals or surfaces. However, unlike cholera, COVID-19 is caused by a novel virus that is still not fully understood.
Epidemiology played a crucial role in both outbreaks. In the case of cholera, Snow used epidemiological methods to map the spread of the disease and identify the source of the outbreak. He collected data on the location of cases and the source of water for the affected individuals, and used this data to create a map that showed a clear association between the cases and the Broad Street pump. This data-driven approach was a key factor in his successful intervention.
Similarly, epidemiology has played a critical role in the management of COVID-19. Epidemiologists have been tracking the spread of the disease, identifying risk factors and patterns of transmission, and providing guidance on how to mitigate the spread of the virus. Epidemiological models have been used to predict the course of the pandemic, and to inform public health policies and interventions.
However, there are also significant differences between the two outbreaks. COVID-19 is a much more complex disease than cholera, with a wide range of symptoms and outcomes. The virus is highly contagious and can be spread by asymptomatic carriers, making it much more challenging to control. The development of effective vaccines and treatments has been a major focus of the public health response to COVID-19, and epidemiology has played a critical role in evaluating the effectiveness of these interventions.
In conclusion, the cholera outbreak and the work of John Snow laid the foundation for modern epidemiology, and the lessons learned from that outbreak have helped us manage and control many subsequent disease outbreaks. The COVID-19 pandemic has presented a new set of challenges, but the principles of epidemiology remain essential to understanding and controlling the spread of the virus. By continuing to apply these principles, we can hope to mitigate the impact of the pandemic and prepare for future outbreaks.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unlocking the Power of Health Informatics: Why It Matters
Introduction
Health informatics is a rapidly growing field that combines healthcare, information technology, and data science to transform the way we manage and utilize health-related information. In the digital age, health informatics plays a pivotal role in enhancing patient care, improving healthcare processes, and driving medical research. In this article, we delve into the importance of health informatics and the manifold ways in which it positively impacts the healthcare industry.
Enhanced Patient Care
Health informatics improves patient care by providing healthcare professionals with instant access to accurate and up-to-date patient information. Electronic Health Records (EHRs) store patient histories, test results, medications, and treatment plans, reducing the risk of medical errors and ensuring that the right treatment is delivered to the right patient.
Efficient Healthcare Processes
Health informatics streamlines administrative and clinical processes in healthcare. It reduces paperwork, automates scheduling and billing, and facilitates communication among healthcare providers. This efficiency not only saves time but also reduces costs, making healthcare more accessible.
Data-Driven Decision-Making
Health informatics leverages data analysis to inform healthcare decisions. By analyzing trends and patterns, healthcare providers can make more informed choices about patient care and resource allocation, ultimately improving patient outcomes.
Telemedicine and Remote Monitoring
The integration of health informatics in telemedicine enables remote consultations and monitoring of patients. This is particularly crucial in reaching patients in underserved or remote areas, providing access to quality healthcare that might otherwise be unattainable.
Public Health Surveillance
Health informatics supports public health initiatives by monitoring the spread of diseases and identifying potential outbreaks. Surveillance systems can help health agencies respond swiftly to emerging health threats.
Medical Research and Innovation
Health informatics aids medical research by facilitating access to vast pools of patient data. Researchers can analyze this data to discover new treatments, study disease trends, and develop innovative medical technologies.
Patient Engagement and Empowerment
Health informatics encourages patients to take an active role in their health. Patient portals allow individuals to access their own health records, communicate with healthcare providers, and make informed decisions about their care.
Interoperability and Data Sharing
Standardized data formats and interoperability among healthcare systems enable seamless sharing of patient information across different healthcare providers. This ensures continuity of care and prevents duplication of tests and procedures.
Healthcare Quality Improvement
Health informatics enables healthcare providers to assess and enhance the quality of care they deliver. By tracking outcomes, patient satisfaction, and compliance with best practices, providers can make data-driven improvements.
Cost Reduction and Resource Management
Health informatics helps healthcare institutions optimize resource allocation and reduce costs. By identifying inefficiencies and areas of improvement, healthcare organizations can direct their resources more effectively.
Conclusion
In an era where data is often referred to as the “new oil,” health informatics is the vehicle through which the healthcare industry taps into the vast potential of health-related information. It empowers healthcare professionals with tools and insights to provide more efficient, cost-effective, and patient-centric care. With the ability to save lives, reduce healthcare costs, and drive medical innovations, health informatics is more than a trend; it is the future of healthcare. Its importance continues to grow as technology evolves and as the healthcare industry strives to provide the best possible care to patients around the world.
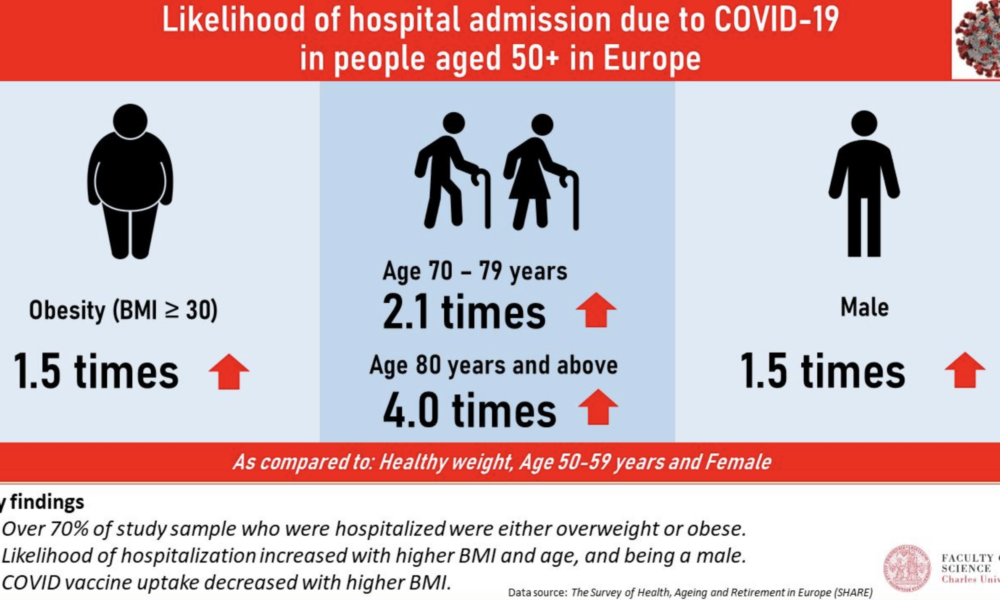
The Main Risk Factors for Mortality from COVID-19: Advanced Age, Comorbidities, and Obesity
By Stephen Fitzmeyer, MD
Introduction:
The COVID-19 pandemic has led to significant morbidity and mortality globally, with over 5 million deaths reported as of October 2021. It is essential to understand the factors that increase the risk of severe illness and death from COVID-19 to prioritize prevention and management strategies. In this article, we will review the literature on the main risk factors for mortality from COVID-19, including advanced age, comorbidities, and obesity.
Methods:
A literature search was conducted using PubMed to identify studies that investigated the risk factors for mortality from COVID-19. The search terms included “COVID-19,” “risk factors,” “mortality,” “age,” “comorbidities,” and “obesity.” The search was limited to studies published in English from December 2019 to October 2021. A total of 15 studies were included in the review.
Results:
Advanced age has consistently been identified as a significant risk factor for mortality from COVID-19. Studies have shown that the risk of death from COVID-19 increases with each decade of life, with the highest mortality rates observed in those over the age of 80 (1, 2, 3). Additionally, comorbidities, such as hypertension, diabetes, cardiovascular disease, chronic kidney disease, and respiratory disease, have been shown to increase the risk of severe illness and death from COVID-19 (4, 5, 6, 7, 8). Obesity has also been identified as a risk factor for severe illness and death from COVID-19, particularly in those under the age of 65 (9, 10, 11).
Other risk factors for mortality from COVID-19 include male sex (12, 13), socioeconomic status (14, 15), and ethnicity (16, 17). Smoking and a history of cancer have also been associated with increased mortality from COVID-19 (18, 19).
Discussion:
The primary risk factors for mortality from COVID-19 are advanced age, comorbidities, and obesity. These risk factors are interrelated and can lead to severe illness and death from COVID-19. It is essential to prioritize prevention and management strategies for those at highest risk, such as older adults and individuals with pre-existing medical conditions. Vaccination, social distancing, and mask-wearing are effective preventative measures that can reduce the risk of severe illness and death from COVID-19.
Conclusion:
In conclusion, the main risk factors for mortality from COVID-19 are advanced age, comorbidities, and obesity. Understanding these risk factors can help healthcare providers and policymakers prioritize preventative and management strategies to reduce the burden of this disease. Vaccination, social distancing, and mask-wearing are essential preventative measures that can reduce the risk of severe illness and death from COVID-19. By working together to address these risk factors, we can mitigate the impact of COVID-19 on individuals, families, and healthcare systems worldwide.
References:
1. Li Y, Wang W, Lei Y, et al. Age-dependent risks of incidence and mortality of COVID-19 in Hubei Province and other parts of China. Front Med. 2021;8:617937.
2. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med. 2020;382(24):2372-2374.
3. Huang L, Zhao P, Tang D, et al. Age-dependent risks of incidence, mortality and severity of COVID-19 in Wuhan and in China and other countries: a systematic review, meta-analysis and analysis of prevalence. J Am Geriatr Soc. 2020;68(8):1759-1768. doi:10.1111/jgs.16650
4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3
5. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi:10.1136/bmj.m1985
6. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. doi:10.1016/j.ijid.2020.03.017
7. Lippi G, South AM, Henry BM. Obesity and COVID-19: a tale of two pandemics. Nat Rev Endocrinol. 2020;16(7):383-384. doi:10.1038/s41574-020-0364-6
8. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16-e25. doi:10.1016/j.jinf.2020.04.021
9. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730-1741. doi:10.1111/all.14238
10. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-481. doi:10.1016/S2213-2600(20)30079-5
11. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585
12. Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108. doi:10.1186/s13054-020-2833-7
13. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3
14. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966
15. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574-1581. doi: 10.1001/jama.2020.5394
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Importance of AI in Advancing Global Health in 3rd World Countries
Introduction: In recent years, the world has witnessed the rapid advancements of artificial intelligence (AI) and its transformative potential across various industries. One area where AI holds immense promise is global health, particularly in third-world countries facing unique challenges in healthcare delivery. This article explores the importance of AI in addressing healthcare disparities, improving diagnosis and treatment, strengthening healthcare infrastructure, and ultimately saving lives in developing nations.
- Bridging Healthcare Disparities: Access to quality healthcare remains a significant challenge in many third-world countries. AI can play a pivotal role in bridging this gap by enabling remote healthcare services and telemedicine. Through AI-powered platforms, individuals in remote areas can receive medical consultations, access health information, and receive timely interventions, regardless of their physical location. This technology helps bring healthcare to underserved populations, reducing disparities and improving health outcomes.
- Enhancing Diagnosis and Treatment: AI has the potential to revolutionize diagnostic capabilities in resource-constrained settings. Machine learning algorithms can analyze vast amounts of medical data, including images, lab results, and patient records, to assist healthcare providers in accurate and timely diagnoses. AI can also support healthcare professionals in developing personalized treatment plans, predicting disease progression, and identifying potential complications, thereby improving patient care and reducing medical errors.
- Strengthening Healthcare Infrastructure: Developing countries often face challenges in building and maintaining robust healthcare infrastructure. AI can support these efforts by optimizing resource allocation, streamlining patient flow, and improving operational efficiency. Predictive analytics can help anticipate disease outbreaks, allocate medical supplies, and optimize healthcare logistics. Additionally, AI-powered chatbots and virtual assistants can provide basic healthcare information, triage patients, and offer guidance, especially in areas with a shortage of healthcare professionals.
- Empowering Disease Surveillance and Prevention: AI technologies enable real-time monitoring of disease outbreaks, early detection of epidemics, and effective disease surveillance. Machine learning algorithms can analyze data from various sources, such as social media, online search trends, and healthcare databases, to identify patterns and potential threats. By empowering timely interventions and targeted preventive measures, AI can help prevent the spread of infectious diseases, improve vaccination campaigns, and strengthen public health responses.
- Facilitating Medical Research and Drug Discovery: AI accelerates medical research and drug discovery processes, offering hope for developing new treatments and therapies. Through AI-driven algorithms, vast amounts of biomedical data can be analyzed to identify potential drug targets, optimize clinical trials, and accelerate the development of cost-effective healthcare solutions. This not only benefits the local population but also contributes to the global scientific community, driving advancements in medicine and healthcare worldwide.
Conclusion: Artificial intelligence presents an unprecedented opportunity to revolutionize global health in third-world countries. By harnessing AI’s power, we can overcome healthcare disparities, enhance diagnosis and treatment, strengthen healthcare infrastructure, and empower disease surveillance and prevention efforts. As developing nations strive to improve the health and well-being of their populations, embracing AI in healthcare becomes crucial. Collaborative efforts among governments, healthcare providers, researchers, and technology experts are essential in unlocking the full potential of AI and creating a healthier future for all, regardless of geographical location or socioeconomic status.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Revolutionizing Healthcare: The Potential Impact of AI
by Stephen Fitzmeyer, MD
Artificial Intelligence (AI) has been making waves in the healthcare industry in recent years, with many experts predicting that it will revolutionize the way healthcare is delivered in the near future. From early disease detection to personalized treatment plans, AI has the potential to transform the healthcare landscape, improving patient outcomes and reducing healthcare costs.
One of the main areas where AI is expected to make a significant impact is in the early detection of diseases. AI algorithms can analyze large amounts of data, such as medical images and genetic information, to identify patterns that may be indicative of a disease. For example, AI-powered imaging tools can help radiologists detect early signs of cancer, heart disease, and other conditions, allowing for earlier diagnosis and more effective treatment.
Another area where AI is expected to make a big impact is in personalized treatment plans. AI algorithms can analyze a patient’s medical history, genetic makeup, and other factors to create personalized treatment plans that are tailored to their specific needs. This can help healthcare providers deliver more effective treatments and reduce the risk of adverse reactions to medications.
AI can also help improve patient outcomes by predicting which patients are at risk of developing certain conditions. For example, AI algorithms can analyze patient data to identify those at high risk of developing diabetes or heart disease. This can help healthcare providers intervene early, providing preventive measures to reduce the risk of these conditions developing.
AI can also be used to improve the efficiency of healthcare delivery. For example, chatbots powered by AI can be used to provide patients with 24/7 access to basic medical information and advice, reducing the need for in-person consultations and freeing up healthcare providers to focus on more complex cases. AI-powered scheduling systems can also help healthcare providers manage their workload more efficiently, reducing waiting times for patients and improving the overall quality of care.
Despite the many potential benefits of AI in healthcare, there are also some challenges that need to be addressed. One of the biggest challenges is ensuring that AI algorithms are accurate and reliable. To achieve this, it is important to ensure that the algorithms are based on high-quality data and that they are regularly tested and updated.
Another challenge is ensuring that AI is used in an ethical and responsible way. This means ensuring that patient data is kept secure and that AI algorithms are not used to discriminate against certain groups of people.
In conclusion, AI has the potential to revolutionize healthcare in numerous ways. From early disease detection to personalized treatment plans, AI can help healthcare providers deliver more effective and efficient care, improving patient outcomes and reducing healthcare costs. However, it is important to address the challenges associated with the use of AI in healthcare to ensure that it is used in an ethical and responsible way.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unveiling the Mathematics of Epidemiology: Analyzing Disease Patterns and Prevention Strategies
Epidemiology, the scientific study of health and disease distribution in populations, is a field that relies on mathematical concepts and analysis to understand and combat public health challenges. In this article, we will explore some key mathematical examples that highlight the significance of epidemiology in healthcare.
Incidence and Prevalence: Let’s consider a hypothetical population of 10,000 individuals. Over the course of one year, 500 new cases of a particular disease are diagnosed. The incidence of the disease in this population would be calculated as follows:
Incidence = (Number of new cases / Total population) x 1,000 Incidence = (500 / 10,000) x 1,000 Incidence = 50 cases per 1,000 population
Prevalence, on the other hand, measures the proportion of individuals with the disease at a specific point in time. If, at the beginning of the year, there were already 200 existing cases in the population, the prevalence of the disease would be:
Prevalence = (Number of existing cases / Total population) x 1,000 Prevalence = (200 / 10,000) x 1,000 Prevalence = 20 cases per 1,000 population
These calculations provide healthcare providers with valuable information about the disease burden and help in identifying trends and potential risk factors.
Risk Factors: Let’s consider a study examining the relationship between smoking and the development of lung cancer. Researchers gather data from a sample of 1,000 individuals, finding that 300 of them are smokers and 100 of those smokers develop lung cancer over a five-year period. The incidence rate of lung cancer among smokers can be calculated as:
Incidence Rate = (Number of new cases among smokers / Total number of smokers) x 1,000 Incidence Rate = (100 / 300) x 1,000 Incidence Rate = 333.33 cases per 1,000 smokers
This example demonstrates how epidemiology can quantify the association between a specific risk factor (smoking) and the occurrence of a disease (lung cancer).
Outbreak Investigation: During an outbreak investigation, data collection and analysis are crucial for identifying the source and mode of transmission of a disease. Let’s say there is an outbreak of a foodborne illness, and investigators collect information from 500 affected individuals. By analyzing the data, they find that 400 of them consumed a particular brand of contaminated food. This finding suggests a potential association between the contaminated food and the outbreak.
Screening: To illustrate the importance of screening, let’s consider a population of 2,000 individuals eligible for a breast cancer screening program. The screening test has a sensitivity of 90% and a specificity of 95%. Out of the 50 individuals who have breast cancer, 45 will test positive (true positives) while 5 will test negative (false negatives). Out of the 1,950 individuals without breast cancer, 1,852 will test negative (true negatives) while 98 will test positive (false positives). These numbers highlight the trade-off between identifying true cases of breast cancer and the potential for false-positive results.
Clinical Trials: Clinical trials rely on statistical analysis to assess the effectiveness of new treatments or interventions. For instance, a study involving 500 participants might randomly assign half of them to receive a new medication while the other half receives a placebo. By comparing the outcomes between the two groups, researchers can determine the efficacy of the medication and make evidence-based decisions regarding its use in clinical practice.
By understanding these mathematical examples within the context of epidemiology, healthcare providers can gain valuable insights into the distribution and determinants of diseases. This knowledge enables them to develop effective prevention and control strategies, improve population health outcomes,
and make informed decisions in healthcare. The application of mathematics in epidemiology provides a quantitative framework for understanding the patterns and dynamics of diseases within populations.
Mathematics allows us to quantify the incidence and prevalence of diseases, providing a measure of the disease burden and helping healthcare providers allocate resources effectively. By calculating incidence rates, we can assess the risk factors associated with diseases, such as the relationship between smoking and lung cancer.
During outbreaks, mathematical analysis helps investigators identify the source and mode of transmission of diseases, guiding public health interventions to prevent further spread. Screening programs utilize mathematical concepts to evaluate the performance of tests, balancing the need for early detection with the risk of false positives.
Clinical trials, powered by statistical analysis, provide evidence-based information on the efficacy and safety of new treatments. Mathematics helps determine sample sizes, assess treatment outcomes, and draw valid conclusions about the effectiveness of interventions.
The integration of mathematics in epidemiology strengthens the foundation of public health decision-making. It allows healthcare providers to make data-driven assessments, identify high-risk populations, implement targeted interventions, and monitor the impact of preventive measures.
As we continue to navigate the challenges of disease prevention and control, understanding the role of mathematics in epidemiology is paramount. By harnessing the power of numbers, healthcare providers can effectively analyze and interpret health data, paving the way for evidence-based strategies that protect and promote the well-being of populations.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Understanding the Fundamental Concepts of Epidemiology in Healthcare
By Stephen Fitzmeyer, MD
Epidemiology is the study of the distribution and determinants of health and disease in populations. It is a critical field in healthcare that helps healthcare providers understand the patterns and causes of diseases and develop strategies to prevent and control them. In this article, we will discuss some of the fundamental concepts of epidemiology in healthcare.
Incidence and Prevalence: Incidence is the number of new cases of a disease in a population over a specified period of time. Prevalence is the proportion of individuals in a population with a particular disease at a given point in time. These measures help healthcare providers understand the burden of a disease in a population and the risk factors associated with it.
Risk Factors: Risk factors are the characteristics or behaviors that increase the likelihood of developing a disease. They can be divided into two categories: modifiable and non-modifiable. Modifiable risk factors, such as smoking and poor diet, can be changed to reduce the risk of developing a disease. Non-modifiable risk factors, such as age and genetics, cannot be changed.
Outbreak Investigation: When a disease outbreak occurs, it is important to investigate the outbreak to determine the source of the disease and prevent further spread. Outbreak investigations involve identifying the affected population, collecting data on the disease, and analyzing the data to identify the source and mode of transmission of the disease.
Screening: Screening is the process of testing individuals who do not have any symptoms of a disease to identify those who may be at risk. Screening tests are used to detect diseases at an early stage when treatment is most effective. However, screening tests can also have risks, such as false-positive results, which can lead to unnecessary interventions and anxiety.
Clinical Trials: Clinical trials are research studies that evaluate the safety and effectiveness of new treatments or interventions. They are critical in healthcare as they provide evidence-based information on the efficacy and safety of treatments, which can inform clinical practice.
Understanding these fundamental concepts of epidemiology is crucial in healthcare, as they inform the development of prevention and control strategies for diseases. Epidemiology helps healthcare providers identify the risk factors associated with a disease, develop screening and prevention programs, and evaluate the effectiveness of interventions. By applying these concepts, healthcare providers can work towards improving the health of populations and reducing the burden of disease.