- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: PHR
Understanding the Continuity of Care Document (CCD) in Healthcare
Stephen Fitzmeyer, MD
In healthcare, it is crucial to have an accurate and complete medical history for patients in order to provide the best possible care. The Continuity of Care Document (CCD) is a standard format for summarizing a patient’s medical history and care plan. It contains a concise summary of the patient’s health status, including medical conditions, medications, allergies, and other relevant information. In this article, we will explore the CCD in more detail, including its structure and use cases.
The CCD is based on the HL7 Clinical Document Architecture (CDA) standard, which provides a framework for structuring clinical documents. The CCD is designed to be a concise, easy-to-read summary of a patient’s health status that can be shared among healthcare providers. It includes information about the patient’s medical conditions, medications, allergies, immunizations, procedures, and laboratory results. The CCD also includes information about the patient’s care plan, such as goals, instructions, and recommended follow-up visits.
The CCD can be used in a variety of settings to improve care coordination and continuity. For example, a patient might be referred from a primary care physician to a specialist. By sharing the CCD, the specialist can quickly get up to speed on the patient’s medical history and current care plan, which can improve the quality of care and reduce the risk of medical errors. The CCD can also be used in emergency situations, where a patient might not be able to provide a complete medical history.
Here are some examples of how the CCD can be used:
Referrals: When a patient is referred from one healthcare provider to another, the referring provider can send a CCD to the receiving provider. This ensures that the receiving provider has all the necessary information to provide appropriate care.
Transitions of Care: When a patient is discharged from a hospital or other healthcare facility, a CCD can be sent to the patient’s primary care provider. This ensures that the primary care provider has all the necessary information to manage the patient’s care after discharge.
Emergency Situations: When a patient is brought to an emergency department, a CCD can be used to provide important medical information to the emergency department staff. This can help ensure that the patient receives appropriate care and treatment.
Patient Portals: Some healthcare organizations offer patient portals that allow patients to access their medical records online. The CCD can be used to provide a summary of the patient’s medical history and care plan in a format that is easy for patients to understand.
In conclusion, the CCD is a standard format for summarizing a patient’s medical history and care plan. It includes information about the patient’s medical conditions, medications, allergies, immunizations, procedures, and laboratory results. The CCD can be used in a variety of settings to improve care coordination and continuity, including referrals, transitions of care, emergency situations, and patient portals. By using the CCD, healthcare providers can improve the quality of care and reduce the risk of medical errors.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
HL7: The Technicalities and Use Cases in Healthcare
By Stephen Fitzmeyer, MD
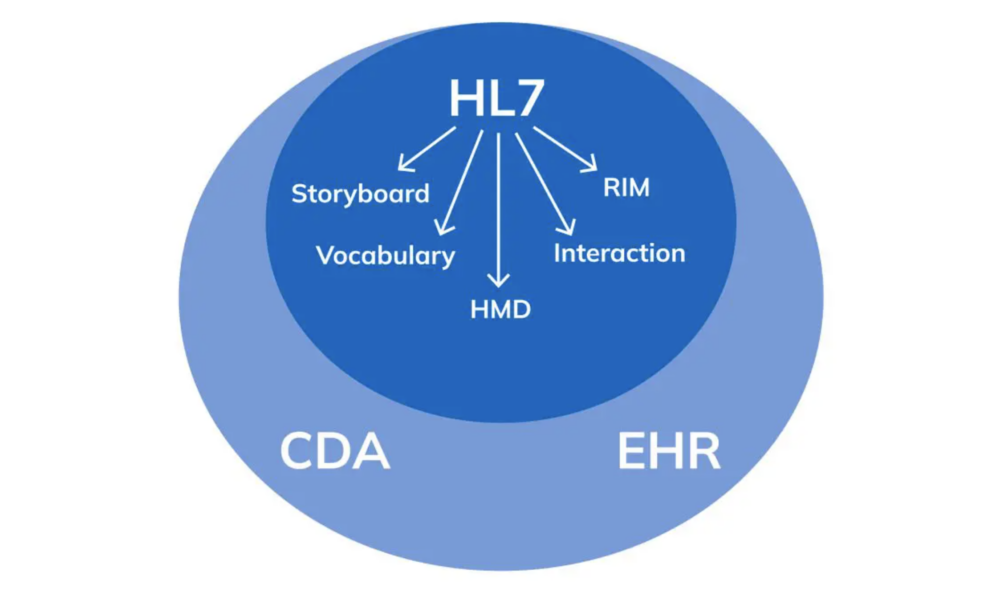
HL7 (Health Level Seven) is a widely adopted standard in healthcare for exchanging information between various healthcare applications, such as electronic health record systems, laboratory information systems, and radiology information systems. The standard defines a set of rules and formats for the exchange of clinical and administrative data. In this article, we will explore the technicalities of HL7 and provide examples of how it can be used in healthcare.
HL7 is composed of several messages, each containing one or more segments. Segments are made up of fields, and fields can contain subfields. Each segment contains information about a specific aspect of a patient’s clinical or administrative data. The most common message types in HL7 are the ADT (Admit, Discharge, Transfer), ORM (Order), and ORU (Observation Result) messages.
For example, an ADT message might contain information about a patient’s admission to the hospital, including their demographic information, admission date and time, and the admitting physician’s name. An ORM message might contain information about a laboratory test order, including the test name, patient’s name, and date and time the test was ordered. An ORU message might contain information about the results of a laboratory test, including the test name, patient’s name, and the actual test results.
HL7 can be used in a variety of ways to exchange data between healthcare applications. For example, a laboratory information system might send an ORU message to an electronic health record system when the results of a laboratory test are ready. The electronic health record system can then display the results to the provider, allowing them to make informed decisions about the patient’s care.
Another example is the use of HL7 in medical billing. A hospital’s billing system might receive ADT messages from an electronic health record system when a patient is admitted, transferred, or discharged. The billing system can then use this information to generate a claim for payment from the patient’s insurance company.
In addition to facilitating data exchange between healthcare applications, HL7 can also be used to integrate clinical decision support systems (CDSS) into electronic health record systems. CDSS systems can analyze patient data and provide recommendations to providers, such as suggesting alternative medications or highlighting potential drug interactions. By integrating CDSS systems with electronic health record systems using HL7, providers can make more informed decisions and improve patient outcomes.
In conclusion, HL7 is a widely adopted standard in healthcare for exchanging clinical and administrative data between various healthcare applications. HL7 messages contain segments and fields that contain patient data, and there are several message types used for different purposes. HL7 can be used to exchange data between applications, integrate CDSS systems into electronic health record systems, and facilitate medical billing. By adopting HL7, healthcare providers can improve patient outcomes and streamline administrative processes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Revolutionizing Patient Forms: Warp Core Health’s AI-Generated Smart Forms
By Stephen Fitzmeyer, MD
Introduction: The repetitive nature of filling out the same forms during each visit to a healthcare provider can be a time-consuming and tedious process for patients. However, Warp Core Health, an innovative healthcare technology company, is leading the charge in transforming the patient form experience. Through their groundbreaking AI-powered solutions, Warp Core Health is developing an AI-generated form that patients fill out once, and subsequently, only relevant information is presented for review and update based on the reason for the visit. This revolution in patient forms aims to streamline the healthcare experience, save time, and improve the overall efficiency of medical visits.
- The Current Challenge: Traditionally, patients are required to provide a comprehensive range of information during each visit, regardless of the reason for their appointment. This results in repetitive and time-consuming form filling, often causing frustration for patients who feel that the process is unnecessary and inefficient. Furthermore, healthcare providers must sift through extensive paperwork to locate the specific details relevant to the visit, creating an additional administrative burden.
- AI-Generated Smart Forms: Warp Core Health’s AI-generated smart forms represent a significant advancement in the patient form process. With the power of artificial intelligence, these forms are designed to be dynamic and tailored to each patient’s specific needs. By leveraging machine learning algorithms, the smart forms intelligently analyze the reason for the visit and present only the relevant sections and questions for review and update.
- Personalized and Streamlined Experience: By eliminating the need to repeat previously provided information, patients can experience a more streamlined and personalized visit. With AI-generated smart forms, patients can focus on updating crucial details related to their current health condition, symptoms, or concerns. This targeted approach ensures that patients’ valuable time is maximized during their appointments, enabling healthcare providers to focus on delivering the most appropriate care.
- Enhanced Accuracy and Efficiency: Warp Core Health’s AI algorithms continually learn from patient data, allowing for improved accuracy and efficiency over time. As patients update their information during subsequent visits, the smart forms intelligently adapt and present new questions or prompts based on previous responses and the reason for the current visit. This iterative process ensures that patient information remains up-to-date and relevant, while minimizing redundant or unnecessary data entry.
- Integration with Electronic Health Records (EHR): Warp Core Health’s AI-generated smart forms seamlessly integrate with existing electronic health record (EHR) systems, creating a powerful synergy between patient information and form customization. As new data is added to the EHR, such as diagnoses, treatments, or test results, it further enhances the customization of smart forms for future visits. The AI algorithms analyze the updated EHR data and dynamically adjust the smart forms to ensure that patients are presented with the most relevant sections and questions specific to their follow-up or next visit. This dynamic customization optimizes the patient form experience, allowing for efficient updates and reviews of pertinent information while eliminating the need to navigate through irrelevant sections. By harnessing the power of EHR integration, Warp Core Health’s smart forms adapt to each patient’s evolving healthcare journey, ensuring a personalized and tailored experience throughout their medical visits.
- Data Security and Privacy: Warp Core Health places a high priority on maintaining the security and privacy of patient data. Their AI-generated smart forms are designed to adhere to stringent data protection regulations, ensuring that sensitive information remains confidential. Robust encryption, access controls, and compliance with industry standards are implemented to safeguard patient privacy throughout the form-filling and data storage processes.
Conclusion: Warp Core Health’s pioneering efforts in developing AI-generated smart forms are set to revolutionize the patient form experience in healthcare. By leveraging artificial intelligence, these forms minimize repetitive data entry, present only relevant information for review and update, and enhance the accuracy and efficiency of medical visits. With seamless integration into electronic health record systems, Warp Core Health ensures that patient information remains up-to-date, contributing to improved continuity of care. As the healthcare industry embraces the power of AI technology, Warp Core Health’s innovative approach to patient forms promises to transform the patient experience, saving time, and improving the overall efficiency of healthcare delivery.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Author: Sharon Lojun, M.D., M.S.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
A Step-by-Step Guide to Coding a Personal Health Record
By Stephen Fitzmeyer, MD
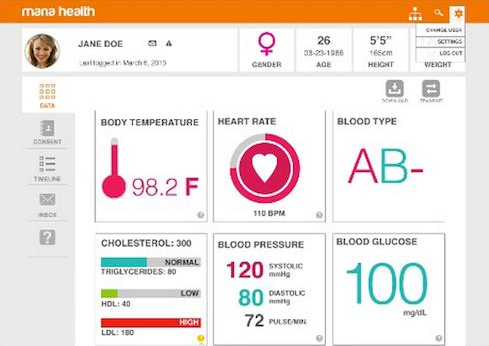
A personal health record (PHR) is a digital tool that allows individuals to maintain and manage their health information in a secure and accessible way. PHRs can be created by healthcare providers or individuals themselves. In this article, we will discuss the steps to coding a PHR.
Step 1: Define the data model
The first step in coding a PHR is to define the data model. This involves identifying the different types of health information that will be stored in the PHR. The data model should include the patient’s demographic information, medical history, medications, allergies, immunizations, laboratory results, and other relevant health information. The data model should also define the relationships between different types of information.
Step 2: Choose a programming language
The next step is to choose a programming language for coding the PHR. There are many programming languages to choose from, including Java, Python, Ruby, and PHP. The choice of programming language will depend on the developer’s expertise, the features required, and the platform on which the PHR will be deployed.
Step 3: Design the user interface
The user interface (UI) is the part of the PHR that patients will interact with. The UI should be intuitive and easy to use. It should allow patients to input and view their health information, as well as update and share it with healthcare providers. The design of the UI should be based on best practices for user experience (UX) and accessibility.
Step 4: Develop the back-end
The back-end of the PHR is the part of the application that handles the storage and retrieval of data. The back-end should be designed to ensure the security and confidentiality of patient health information. It should also be scalable and efficient, to handle large volumes of data and support future expansion.
Step 5: Integrate with other systems
PHRs need to integrate with other healthcare systems, such as electronic health records (EHRs), health information exchanges (HIEs), and patient portals. Integration with these systems will allow patients to access their health information from different sources, and share it with healthcare providers as needed.
Step 6: Test and deploy
Before deploying the PHR, it is essential to test it thoroughly to ensure that it works as expected and meets the needs of patients and healthcare providers. Testing should include functionality testing, performance testing, security testing, and user acceptance testing. Once testing is complete, the PHR can be deployed on a secure platform, such as a cloud-based server or a local server.
Conclusion
Coding a PHR requires careful planning and attention to detail. By following the steps outlined in this article, developers can create a PHR that is secure, scalable, and user-friendly. A well-designed PHR can empower patients to take control of their health information, improve healthcare outcomes, and support the delivery of personalized and coordinated healthcare services.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/