- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
- Home
- Warp Core Health
- Blog
- Biochemistry
- Mitochondrial Metabolism: An Essential Regulator of Adipose Tissue, Metabolic Health, Inflammation, and Brain Function
Mitochondrial Metabolism: An Essential Regulator of Adipose Tissue, Metabolic Health, Inflammation, and Brain Function
- September 15, 2023
- Stephen Fitzmeyer, MD
- Biochemistry, Fats, Metabolic Health, Mitochondria
- No Comments
By Stephen Fitzmeyer, MD
Mitochondria, often referred to as the powerhouses of the cell, play a crucial role in various aspects of human physiology. Beyond their well-known role in energy production, emerging research has shed light on the intricate relationship between mitochondrial metabolism and adipose tissue development and function. Moreover, recent discoveries have highlighted the impact of mitochondrial metabolism on metabolic health, inflammation, and even brain function. Understanding these connections could pave the way for new therapeutic strategies in tackling obesity, metabolic disorders, and neurodegenerative diseases.
Adipose tissue, commonly known as fat, was once perceived as an inert energy storage depot. However, it is now recognized as a dynamic and metabolically active organ that influences whole-body homeostasis. Adipose tissue consists of two main types: white adipose tissue (WAT) and brown adipose tissue (BAT). WAT primarily stores energy in the form of triglycerides, while BAT dissipates energy through thermogenesis. Both types of adipose tissue are influenced by mitochondrial metabolism, albeit in different ways.
In WAT, mitochondrial metabolism has been found to regulate adipogenesis, the process by which precursor cells differentiate into mature adipocytes. Studies have shown that impaired mitochondrial function leads to dysfunctional adipocyte differentiation and altered adipose tissue development. Furthermore, mitochondrial dysfunction in WAT has been linked to insulin resistance, a hallmark of metabolic disorders such as obesity and type 2 diabetes.
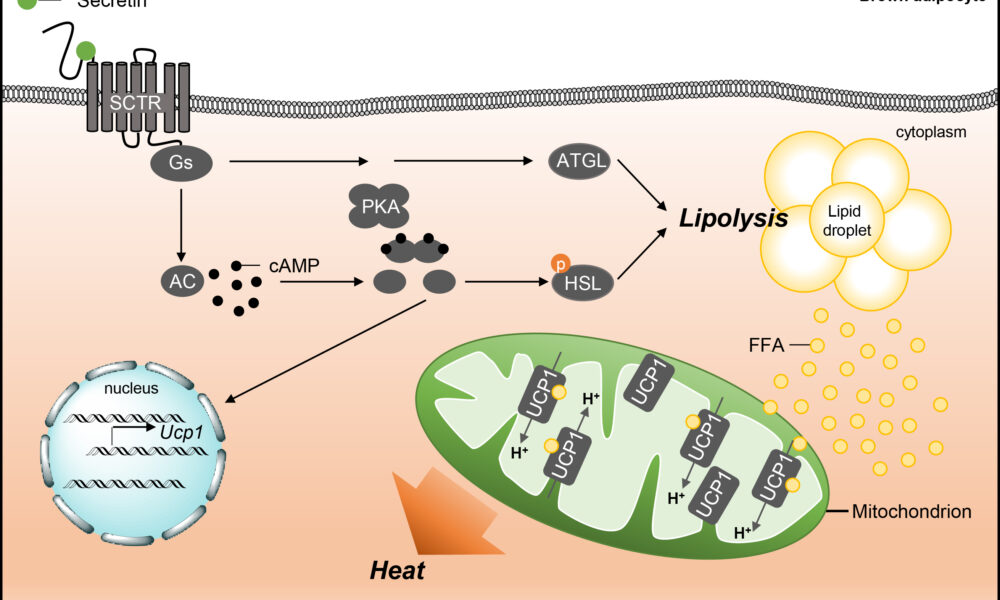
On the other hand, BAT is enriched with mitochondria and possesses a high capacity for oxidative metabolism. Brown adipocytes express a protein called uncoupling protein 1 (UCP1), which uncouples oxidative phosphorylation from ATP synthesis, resulting in the generation of heat. This unique characteristic of BAT is essential for maintaining body temperature and regulating energy expenditure. Emerging evidence suggests that impaired mitochondrial metabolism in BAT contributes to obesity and metabolic dysfunction. Conversely, enhancing mitochondrial function in BAT has been proposed as a potential therapeutic strategy to combat obesity and associated metabolic disorders.
Mitochondrial metabolism not only influences adipose tissue development and function but also plays a pivotal role in metabolic health and inflammation. Dysfunctional mitochondria can lead to an imbalance in cellular energy metabolism, resulting in the accumulation of toxic metabolites and the generation of reactive oxygen species (ROS). Excessive ROS production contributes to oxidative stress and chronic low-grade inflammation, which are closely associated with obesity, insulin resistance, and cardiovascular diseases. Inflammation disrupts normal adipose tissue function and can further exacerbate metabolic dysfunction.
Furthermore, recent studies have highlighted the impact of mitochondrial metabolism on brain health and function. The brain is a highly energy-demanding organ, and mitochondrial dysfunction has been implicated in various neurodegenerative disorders, including Alzheimer’s and Parkinson’s diseases. Impaired mitochondrial function in the brain can lead to reduced energy production, compromised neuronal activity, and increased vulnerability to oxidative stress and inflammation. Therefore, maintaining mitochondrial health in the brain is crucial for preserving cognitive function and preventing neurodegeneration.
The intricate interplay between mitochondrial metabolism, adipose tissue development, metabolic health, inflammation, and brain function underscores the importance of understanding these relationships in a holistic manner. Targeting mitochondrial dysfunction may hold promise for therapeutic interventions aimed at improving metabolic health, combating obesity, and even mitigating neurodegenerative diseases.
In conclusion, mitochondrial metabolism is a key regulator of adipose tissue development and function. It influences both white and brown adipose tissues, impacting metabolic health, inflammation, and even brain function. Exploring the molecular mechanisms underlying these connections could provide valuable insights into the pathogenesis of obesity, metabolic disorders, and neurodegenerative diseases. Ultimately, this knowledge may open doors to novel therapeutic strategies that target mitochondrial function, empowering individuals to take control of their metabolic well-being and combat the growing burden of obesity and associated diseases. By promoting mitochondrial health and optimizing adipose tissue function, we may pave the way for a healthier future.
It is evident that mitochondria play a multifaceted role in our bodies, extending far beyond their traditional association with energy production. Their influence on adipose tissue development and function, metabolic health, inflammation, and brain function highlights their significance in maintaining overall physiological balance.
As researchers continue to delve into the intricate mechanisms that govern mitochondrial metabolism, new therapeutic avenues may emerge. Targeted interventions aimed at enhancing mitochondrial function could potentially revolutionize the treatment of metabolic disorders, including obesity, insulin resistance, and neurodegenerative diseases.
Moreover, advancements in our understanding of mitochondrial metabolism may lead to the identification of novel biomarkers for early detection and risk assessment of these conditions. This could enable personalized interventions and interventions at an earlier stage, with the potential to halt or reverse disease progression.
However, it is important to acknowledge that the complexities of mitochondrial metabolism and its interactions with various bodily systems require further investigation. Ongoing research is needed to unravel the underlying mechanisms and to validate the potential therapeutic strategies that target mitochondrial function.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Recent Posts
- Protected: Warp Core Health: Building a Custom AI Model for Transforming Healthcare
- The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
- Accessing Siloed EMR Systems with FHIR: Connecting to Multiple EMRs
- How AI and Informatics Are Transforming Healthcare
- How AI Can Transform Healthcare Applications
Categories
- ApoB
- Artificial Intelligence
- Autophagy
- Biochemistry
- Biomedical Informatics
- Biostatistics
- Blood Glucose
- CAC
- Carbs
- CCD
- CDA
- Clinical Informatics
- Coding Bootcamp
- Coronary Artery Disease
- COVID-19
- Cybersecurity
- Data Science
- Diabetes
- Diet
- EHS
- EMR
- Epidemiology
- Evidence Based Medicine
- Fats
- FHIR
- Fiber
- Generative AI
- Global Health
- Health Administration
- Health Informatics
- Health IT
- HIPAA
- HL7
- Hyperglycemia
- Hypoglycemia
- ICD 10
- Intermittent Fasting
- Ketogenic Diet
- Machine Learning
- Macronutrients
- MCT Oil
- Metabolic Health
- Metabolic Syndrome
- Minerals
- Mitochondria
- MySQL
- Neurology
- Nutritional Ketosis
- Nutritional Neurology
- Nutritional Psychiatry
- PHP
- PHR
- Programming
- Prompt Engineering
- Proteins
- Prototypes
- Public Health
- Python
- Recipes
- Sleep Health
- Stroke
- Uric Acid
- Vegan and Vegetarians
- Vitamin D
- Vitamin K2
- Vitamins