- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
- Home
- Warp Core Health
- Blog
- Metabolic Syndrome
Category: Metabolic Syndrome
Reversing Metabolic Syndrome: The Power of a Ketogenic Diet and Intermittent Fasting
- April 24, 2024
- Stephen Fitzmeyer, MD
- No Comments
Introduction:
Metabolic syndrome is a cluster of metabolic abnormalities characterized by insulin resistance, high blood pressure, excessive abdominal fat, elevated triglyceride levels, and low levels of HDL cholesterol. It is a significant risk factor for various chronic conditions, including type 2 diabetes and cardiovascular disease. However, emerging evidence suggests that a ketogenic diet and intermittent fasting (IF) can be powerful tools in reversing metabolic syndrome and restoring optimal metabolic health. In this article, we will explore the potential of a ketogenic diet and IF to combat metabolic syndrome and promote overall well-being.
Understanding Optimal Metabolic Health:
To determine optimal metabolic health, various markers are considered. These markers include:
- A1C: A measure of average blood sugar levels over the past two to three months. An A1C level of less than 5.7% is generally considered optimal.
- Blood Pressure: Blood pressure lower than 120/80 mmHg is considered within the normal range and indicative of good metabolic health.
- Waist Circumference: Excessive abdominal fat, often measured by waist circumference, is a key indicator of metabolic syndrome. A waist circumference of 0.5 or less is considered optimal.
- Triglycerides: Triglyceride levels below 150 mg/dL are typically considered healthy and associated with lower risk of metabolic syndrome.
- HDL Cholesterol: High-density lipoprotein (HDL) cholesterol is often referred to as “good” cholesterol. Levels of HDL cholesterol at or above 60 mg/dL (1.6 mmol/L) are generally considered desirable.
Reversing Metabolic Syndrome with a Ketogenic Diet and IF:
- Ketogenic Diet: A ketogenic diet is low in carbohydrates, moderate in protein, and high in healthy fats. By drastically reducing carbohydrate intake, the body enters a state of ketosis, where it primarily burns fat for fuel instead of glucose. This metabolic shift can lead to significant improvements in metabolic markers.
- Insulin Resistance: Carbohydrate restriction and the production of ketones during a ketogenic diet can improve insulin sensitivity and reduce insulin resistance.
- Weight Loss: A ketogenic diet is often associated with weight loss, especially abdominal fat. This reduction in excess fat can positively impact waist circumference and metabolic health.
- Triglycerides and HDL Cholesterol: A ketogenic diet typically leads to a decrease in triglyceride levels and an increase in HDL cholesterol, both of which are beneficial for metabolic health.
- Intermittent Fasting (IF): IF involves cycling between periods of eating and fasting. This eating pattern promotes metabolic flexibility and enhances the body’s ability to utilize stored fat for fuel.
- Insulin Sensitivity: IF can improve insulin sensitivity and reduce insulin levels, contributing to better glycemic control and metabolic health.
- Blood Pressure: Some studies suggest that IF can help lower blood pressure, potentially improving overall cardiovascular health.
- Weight Management: By restricting the eating window and promoting calorie control, IF can aid in weight loss and reduction of abdominal fat.
- A1C and Triglycerides: IF has shown promising effects on improving glycemic control and reducing triglyceride levels in individuals with metabolic syndrome.
Conclusion:
Metabolic syndrome is a significant health concern that increases the risk of chronic conditions. However, the combination of a ketogenic diet and intermittent fasting offers a powerful approach to reversing metabolic syndrome and restoring optimal metabolic health.
By adopting a ketogenic diet, individuals can shift their metabolism to efficiently burn fat for fuel, leading to improvements in insulin sensitivity, weight loss, and favorable changes in lipid profiles. Intermittent fasting complements the ketogenic diet
by promoting metabolic flexibility, reducing insulin levels, and aiding in weight management.
When followed diligently and under proper supervision, a ketogenic diet and intermittent fasting can help individuals meet the criteria for optimal metabolic health. By adopting these lifestyle modifications, individuals failing to meet three or more of the markers can potentially reverse metabolic syndrome and improve overall well-being.
It is important to note that before embarking on any significant dietary changes, it is crucial to consult with a healthcare professional or a registered dietitian who can provide personalized guidance and ensure that the chosen approach is suitable for individual needs and health conditions.
In conclusion, a ketogenic diet and intermittent fasting offer a promising strategy for reversing metabolic syndrome. By focusing on reducing carbohydrate intake, promoting healthy fat consumption, and incorporating fasting periods, individuals can improve insulin sensitivity, achieve weight loss, manage blood pressure, and optimize lipid profiles. Reversing metabolic syndrome through these dietary interventions not only mitigates the risk of chronic diseases but also enhances overall metabolic health and promotes a better quality of life.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Role of Vitamin D in Reducing Severity of COVID-19: A Review of the Evidence
- April 7, 2024
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
The COVID-19 pandemic has caused significant morbidity and mortality worldwide. Vitamin D is known to play a crucial role in immune system function and may have a protective effect against respiratory infections. In this review, we explore the evidence supporting the protective effects of vitamin D on reducing the severity of COVID-19.
Body:
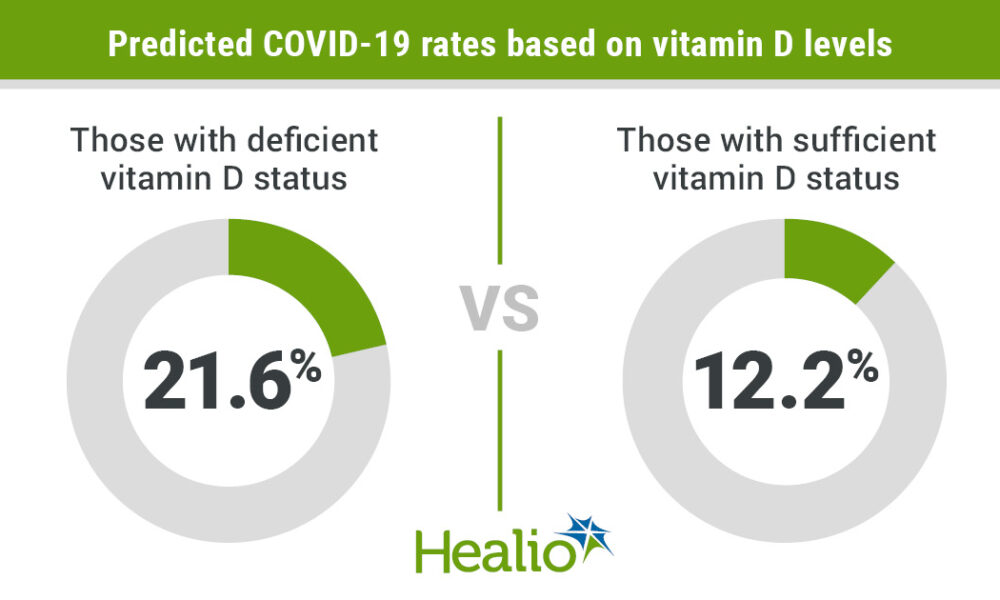
Numerous studies have reported an association between vitamin D deficiency and increased risk of respiratory infections, including COVID-19. In a systematic review and meta-analysis, Jolliffe et al. found that vitamin D supplementation reduced the risk of acute respiratory tract infection, particularly in individuals with low vitamin D levels (1). Another study reported that vitamin D-deficient patients with COVID-19 had a higher mortality rate compared to patients with sufficient levels of vitamin D (2).
Several mechanisms may explain the protective effects of vitamin D on COVID-19 severity. Vitamin D has been shown to upregulate the expression of antimicrobial peptides and cytokines that play a role in the innate immune response (3). Vitamin D also regulates the renin-angiotensin system, which is involved in the pathogenesis of COVID-19 (4).
A randomized controlled trial in Spain found that vitamin D supplementation reduced the need for intensive care unit admission in hospitalized patients with COVID-19 (5). Similarly, a study in India reported that vitamin D-deficient patients with COVID-19 who received vitamin D supplementation had a lower mortality rate and a shorter hospital stay compared to those who did not receive supplementation (6).
Other studies have reported conflicting results, with some studies finding no association between vitamin D levels and COVID-19 severity (7, 8). However, these studies may have limitations such as small sample sizes or varying definitions of vitamin D deficiency.
Conclusion:
Overall, the evidence suggests that vitamin D may have a protective effect against COVID-19 severity. Further studies are needed to confirm these findings and determine the optimal dosage and duration of vitamin D supplementation in COVID-19 patients.
References:
1. Jolliffe DA, Camargo CA Jr, Sluyter JD, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583.
2. Jain A, Chaurasia R, Sengar NS, et al. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep. 2020;10(1):20191.
3. Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881-886.
Alwarawrah Y, Kiernan K, MacIver NJ. Changes in Nutrient Levels Shape Immune Responses. J Immunol Res. 2018;2018:8202585.
4. Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, et al. “Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study”. J Steroid Biochem Mol Biol. 2020;203:105751.
5. Rastogi A, Bhansali A, Khare N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomized, placebo-controlled, study (SHADE study). Postgrad Med J. 2020;97(1147):442-447.
6. Rastogi A, Bhansali A, Khare N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomized, placebo-controlled, study (SHADE study). Postgrad Med J. 2020;0:1-7.
7. Alcala-Diaz JF, Limia-Perez L, Guerrero-Romero F, et al. Calcifediol treatment and hospital mortality due to COVID-19: a cohort study. Nutrients. 2021;13(5):1760.
8. Imran TF, Rahman A, Mahmood T, et al. Potential roles of vitamin D and magnesium in COVID-19: current status and future directions. Heliyon. 2021;7(4):e06812.
9. Noguera-Julian M, Marquez L, Buño A, et al. Low vitamin D status is associated with worse ICU outcome in COVID-19. Nutrients. 2021;13(4):1351. doi:10.3390/nu13041351. PMID: 33920934; PMCID: PMC8071314.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Example Patient Data Stored in a MySQL Database in SQL Format
- March 15, 2024
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
here is an example of patient data stored in a MySQL database in SQL format:
CREATE TABLE patients (
patient_id INT AUTO_INCREMENT PRIMARY KEY,
name VARCHAR(50) NOT NULL,
age INT NOT NULL,
gender VARCHAR(10) NOT NULL,
diagnosis VARCHAR(100),
medication VARCHAR(100),
medication_start_date DATE,
medication_end_date DATE
);
INSERT INTO patients (name, age, gender, diagnosis, medication, medication_start_date, medication_end_date)
VALUES (‘John Smith’, 45, ‘Male’, ‘Diabetes’, ‘Metformin’, ‘2021-01-01’, ‘2022-01-01’),
(‘Jane Doe’, 35, ‘Female’, ‘Hypertension’, ‘Lisinopril’, ‘2021-02-01’, ‘2022-02-01’),
(‘Mike Johnson’, 50, ‘Male’, ‘Chronic Obstructive Pulmonary Disease’, ‘Albuterol’, ‘2021-03-01’, ‘2022-03-01’),
(‘Sarah Lee’, 28, ‘Female’, ‘Anxiety’, ‘Sertraline’, ‘2021-04-01’, ‘2022-04-01’);
This creates a table called “patients” with columns for patient_id, name, age, gender, diagnosis, medication, medication_start_date, and medication_end_date. The INSERT statements add four patient records to the table, each with a name, age, gender, diagnosis, medication, medication start date, and medication end date. This is just an example, and the table structure and data can be customized to suit your specific healthcare application.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unlocking Heart Health: Confronting the Metabolic Syndrome Epidemic Impacting 88% of American Adults
- January 5, 2024
- Stephen Fitzmeyer, MD
- Comments Off on Unlocking Heart Health: Confronting the Metabolic Syndrome Epidemic Impacting 88% of American Adults
Introduction:
In the realm of heart health, cholesterol has long been in the spotlight. However, emerging research challenges the traditional understanding of cholesterol and its impact on cardiovascular issues. It’s time to take a closer look at the outdated science surrounding LDL cholesterol measurements and explore a fresh perspective on preventing chronic diseases like atherosclerosis and coronary heart disease.
Metabolic Syndrome: The Real Culprit:
Rather than fixating solely on LDL cholesterol, it’s essential to understand the role of Metabolic Syndrome in the development of cardiovascular issues. Shockingly, an estimated 88% of adults in the United States suffer from or will suffer from chronic diseases associated with Metabolic Syndrome. This condition is caused by hyperinsulinemia, a result of the Standard American Diet rich in carbohydrates and sugars.
A Comprehensive Approach:
To effectively address Metabolic Syndrome, it’s crucial to measure and manage its individual components. These include A1C levels (average blood sugar), blood pressure, waist/height ratio, triglyceride levels, and HDL cholesterol levels. By focusing on these factors, you can make targeted lifestyle adjustments and mitigate the risk of developing atherosclerosis and coronary heart disease.
The Power of Coronary Artery Calcium (CAC) Scans:
While LDL cholesterol measurements may be unreliable predictors, there is a valuable diagnostic tool: the Coronary Artery Calcium (CAC) scan. This scan provides detailed images of the coronary arteries and identifies calcium deposits, which serve as early signs of coronary artery disease. By tracking your CAC score, you can accurately gauge your risk of heart disease and take appropriate action.
Understanding Your CAC Score:
A CAC score of 0 indicates no plaque detected, signifying a minimal risk of coronary artery disease. As the score increases, the risk also escalates. For instance, scores between 1 and 10 represent extremely minimal levels of calcium, while scores of 300 or higher suggest extensive plaque and a significantly elevated risk of heart attack. Achieving a CAC score of 0 should be the ultimate goal in your heart health journey.
Reversing Metabolic Syndrome:
To lower your CAC score and reverse Metabolic Syndrome, dietary changes are paramount. Adopting a low-carbohydrate approach while focusing on whole foods is key. Emphasize high-fat (75%), moderate-protein (20%), and low-carb (5%) choices. By eliminating or significantly reducing your intake of carbohydrates and sugars, you can optimize your metabolism and support overall heart health.
The Role of “Seed Oils” in Chronic Diseases:
In addition to dietary adjustments, it’s vital to avoid “seed oils” for optimal health. Oils like soybean, safflower, sunflower, and others were initially intended for industrial purposes, not human consumption. The introduction of these oils into the American diet coincided with a rise in obesity, diabetes, stroke, heart disease, Alzheimer’s, and other chronic diseases. Opt for healthier alternatives like butter, lard, and olive oil to protect your well-being.
Reconceptualizing Heart Disease and Type 3 Diabetes:
Research suggests a compelling connection between heart disease and undiagnosed diabetes. Furthermore, there is a growing movement to rename dementia and Alzheimer’s as Type 3 Diabetes, emphasizing the influence of carbohydrates and sugars on brain health. This new perspective challenges the conventional notion of a low-fat diet and opens the door to exploring the benefits of low-carb approaches.
Conclusion:
Rethinking cholesterol and adopting a comprehensive approach to heart health is crucial. By understanding the significance of Metabolic Syndrome, prioritizing CAC scans, and making strategic dietary adjustments, you can optimize your cardiovascular well-being. Embrace the power of whole foods, eliminate harmful oils, and consider the connections between heart disease, diabetes, and carbohydrate consumption. By taking these steps, you can pave the way for a healthier heart and a reduced risk of chronic diseases.
Remember, it’s always essential to consult with your healthcare provider before making any significant changes to your diet or lifestyle. Together, you can tailor a plan that suits your specific needs and promotes optimal heart health.
Embrace the paradigm shift in understanding cholesterol and take charge of your cardiovascular well-being today. Your heart will thank you for it.
Author:
Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Are You One of the 88% of the the U.S. Adult Population suffering from Chronic Inflammation? Here’s what you should know to find out and fix it.
- August 15, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
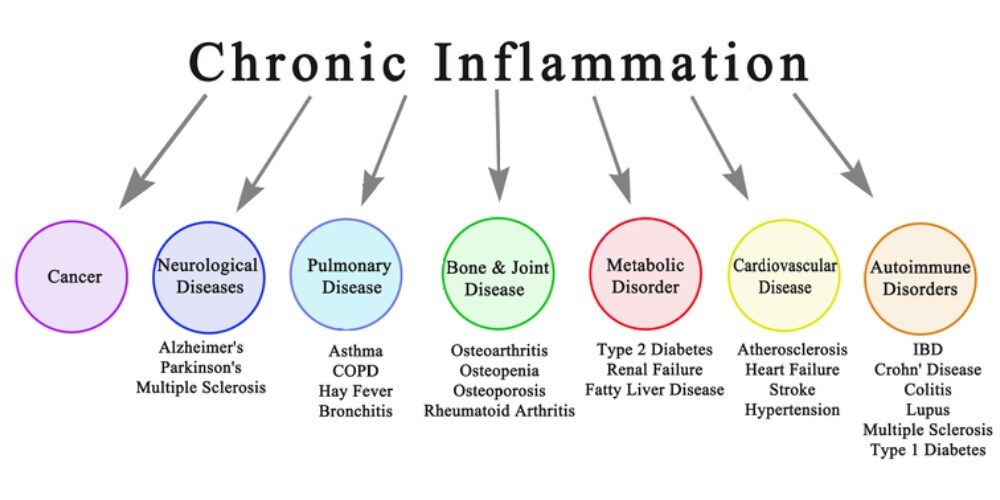
Introduction: Chronic inflammation is a silent yet powerful contributor to various health problems. It serves as a warning sign of underlying conditions such as metabolic syndrome, poor diet, and other chronic diseases. In this article, we aim to shed light on the detrimental effects of chronic inflammation and emphasize the significance of making positive lifestyle changes to prevent its progression and the onset of related health issues.
Chronic inflammation has been linked to the development of several chronic diseases, including cardiovascular disease, type 2 diabetes, autoimmune disorders, obesity, cancer, neurodegenerative diseases, and respiratory diseases. Understanding the significant impact of chronic inflammation on these chronic diseases highlights the urgency of addressing inflammation through lifestyle modifications.
Part 1: Chronic Inflammation and its Link to Metabolic Syndrome
Chronic inflammation is closely intertwined with metabolic syndrome, a cluster of conditions that includes obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels. This syndrome sets the stage for chronic inflammation, fueling a vicious cycle. As chronic inflammation persists, it further promotes the development of metabolic abnormalities, increasing the risk of cardiovascular disease, type 2 diabetes, and other chronic illnesses.
Part 2: The Role of Diet in Chronic Inflammation
A poor diet plays a significant role in chronic inflammation. Consuming processed foods high in refined carbohydrates, added sugars, unhealthy fats, and artificial additives triggers an inflammatory response within the body. Moreover, the excessive intake of omega-6 fatty acids found in seed oils, commonly used in processed foods, promotes an imbalance in the omega-6 to omega-3 ratio, further exacerbating inflammation. To reduce chronic inflammation, it is important to avoid seed oils such as soybean oil, corn oil, sunflower oil, and cottonseed oil, and instead opt for healthier alternatives like olive oil, avocado oil, and coconut oil.
Part 3: Inflammatory Markers to Assess Chronic Inflammation
If you suspect chronic inflammation, your physician may order specific blood tests to assess inflammatory markers in your body. These markers can provide valuable insights into the presence and extent of inflammation. Common inflammatory markers include:
- C-reactive Protein (CRP): Elevated CRP levels indicate systemic inflammation and can be indicative of various diseases.
- Erythrocyte Sedimentation Rate (ESR): ESR measures the rate at which red blood cells settle in a tube, which can be elevated during inflammation.
- Interleukin-6 (IL-6): IL-6 is a cytokine involved in the inflammatory response, and increased levels may indicate ongoing inflammation.
- Tumor Necrosis Factor-alpha (TNF-α): TNF-α is another cytokine associated with inflammation, and elevated levels are observed in chronic inflammatory conditions.
- Fasting Insulin: Insulin resistance, often associated with chronic inflammation, can be assessed through fasting insulin levels.
Part 4: Taking Control: Lifestyle Changes to Combat Chronic Inflammation
The good news is that chronic inflammation is not entirely beyond our control. By making positive lifestyle changes, we can reduce its impact and mitigate the risks associated with it. Here are some key steps to consider:
- Adopting a Healthy Diet: By adopting a high-fat, low-carb diet rich in healthy fats, adequate protein, and non-starchy vegetables, you can reduce chronic inflammation, enhance your overall well-being, and enjoy a healthier and more vibrant life. Emphasize foods such as fatty fish, grass-fed meats, eggs, nuts, seeds, avocados, olive oil, and non-starchy vegetables. Avoid processed foods, sugary beverages, and seed oils high in omega-6 fatty acids, as they contribute to inflammation.
- Regular Exercise: Engage in regular physical activity to combat obesity, improve insulin sensitivity, and reduce systemic inflammation.
- Stress Management: Chronic stress contributes to inflammation. Incorporate stress management techniques such as meditation, mindfulness, and relaxation exercises into your routine.
Conclusion: Chronic inflammation is a red flag indicating underlying health issues and the potential development of chronic diseases. Metabolic syndrome, poor diet, and other factors contribute to its persistence. By recognizing the role of chronic inflammation in these conditions, we can take proactive steps to address it through lifestyle modifications. Adopting a healthy diet, engaging in regular exercise, managing stress, and avoiding seed oils are crucial in combating chronic inflammation and reducing the risk of associated chronic diseases.
If you suspect chronic inflammation, it is essential to consult with your healthcare provider. They can order specific blood tests to assess inflammatory markers in your body, such as C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and fasting insulin. These tests provide valuable insights into the presence and extent of inflammation, helping your physician develop an appropriate treatment plan.
Don’t wait until chronic inflammation leads to more serious health complications. Take action now to protect your well-being and prevent the development of chronic diseases. Your health is your most valuable asset, and addressing chronic inflammation is a vital step in safeguarding it.
Remember, you are in control of your health. By making conscious choices and adopting a proactive approach, you can reduce chronic inflammation, improve your well-being, and lead a vibrant life. Prioritize your health, make informed choices, and embrace a lifestyle that promotes well-being. Understanding the connection between chronic inflammation, metabolic syndrome, poor diet, and chronic diseases empowers you to break free from this harmful cycle and achieve better health and vitality. Start today and enjoy the long-term benefits of a life free from chronic inflammation. Your body will thank you for it.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Exonerating Salt: Metabolic Syndrome Unveiled as the Underlying Culprit of Hypertension
- August 1, 2023
- Dr. Stephen Fitzmeyer, Dr. Sharon Lojun
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
Hypertension, commonly known as high blood pressure, has long been associated with excessive salt intake. However, emerging research challenges this widely accepted belief, suggesting that hypertension is primarily a result of metabolic syndrome rather than a direct consequence of salt consumption. Metabolic syndrome, characterized by a cluster of metabolic abnormalities, including obesity, insulin resistance, and dyslipidemia, plays a pivotal role in salt retention and the development of hypertension. In this article, we will explore the misconceptions surrounding the salt hypothesis and delve into the intricate connection between metabolic syndrome and hypertension.
The Salt Paradox:
For decades, medical professionals and public health campaigns have emphasized reducing salt intake as a means to prevent and manage hypertension. However, the relationship between salt consumption and hypertension is not as straightforward as once believed. Numerous studies have failed to establish a consistent link between salt intake and blood pressure elevation. Furthermore, populations consuming low-salt diets have not demonstrated significant reductions in hypertension rates. This paradox raises questions about the true nature of the relationship between salt and hypertension.
Metabolic Syndrome: The Underlying Culprit:
Metabolic syndrome, a cluster of interconnected metabolic abnormalities, is now recognized as a significant contributor to hypertension. Obesity, insulin resistance, dyslipidemia, and chronic inflammation characteristic of metabolic syndrome disrupt the body’s delicate balance, leading to salt retention and the subsequent rise in blood pressure. Insulin resistance, a hallmark of metabolic syndrome, impairs sodium excretion by the kidneys, promoting salt retention and fluid accumulation. These metabolic derangements create a vicious cycle, perpetuating hypertension and further exacerbating the effects of salt retention.
Unveiling the Root Causes:
While salt intake may play a minor role in hypertension for a subset of individuals with salt sensitivity, it is crucial to focus on the underlying metabolic dysfunctions. Ultra-processed carbohydrates and fats, prevalent in modern diets, have been identified as primary culprits in the development of metabolic syndrome. These refined and heavily processed food products contribute to obesity, insulin resistance, and chronic inflammation, creating an environment conducive to hypertension and salt retention.
The Role of Lifestyle Interventions:
In addressing the underlying metabolic dysfunctions associated with hypertension, lifestyle interventions take center stage. A ketogenic diet, characterized by low carbohydrate intake and increased fat consumption, has shown promising results in improving metabolic health and blood pressure control. By shifting the body’s primary fuel source from carbohydrates to fats, a ketogenic diet improves insulin sensitivity, promotes weight loss, and mitigates chronic inflammation, thereby tackling the root causes of hypertension.
Intermittent fasting, an eating pattern that cycles between periods of fasting and feeding, has also demonstrated metabolic benefits. Beyond calorie restriction, intermittent fasting enhances insulin sensitivity, promotes autophagy, and regulates blood pressure, making it a valuable tool in the management of hypertension associated with metabolic syndrome.
Conclusion:
Contrary to the long-standing belief that salt intake is the primary driver of hypertension, the emerging evidence suggests that metabolic syndrome, with its associated metabolic dysfunctions, is the root cause of salt retention and subsequent development of hypertension. While salt sensitivity may play a role in some individuals, it is essential to address the broader metabolic context to effectively manage hypertension. Lifestyle interventions, such as adopting a ketogenic diet and incorporating intermittent fasting, offer promising strategies to reverse metabolic syndrome, improve metabolic health, and alleviate hypertension. By shifting the focus from salt intake to metabolic health, we can reframe our approach to hypertension management and pave the way for more effective prevention and treatment strategies.
Why Your Doctor Should Start Paying Attention to Your Uric Acid Levels
- June 29, 2023
- Stephen Fitzmeyer, MD
- No Comments
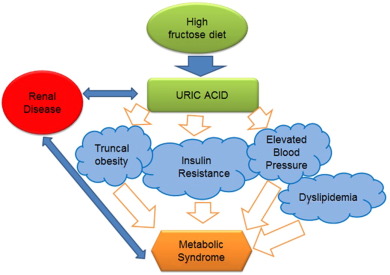
Uric acid, a natural waste product created during the breakdown of purines in the body, has long been associated with a painful condition known as gout. However, recent research has shown that elevated uric acid levels can have broader health implications beyond gout, indicating the importance of monitoring and managing uric acid levels in routine medical care. This article explores the reasons why your doctor should start paying attention to your uric acid levels and how adopting a ketogenic diet can help lower uric acid levels and promote metabolic health.
Gout Prevention and Management: Gout is a form of arthritis characterized by sudden, severe joint pain, swelling, and redness. It occurs when uric acid crystals accumulate in the joints, leading to inflammation. Monitoring uric acid levels can help identify individuals at risk of developing gout and enable early intervention. By proactively managing uric acid levels through lifestyle modifications and medications, doctors can help prevent recurrent gout attacks and minimize joint damage.
Uric Acid as an Independent Risk Factor: Elevated uric acid levels have been linked to various health conditions independent of gout. Research suggests that high uric acid levels may contribute to the development of hypertension, cardiovascular disease, chronic kidney disease, and metabolic syndrome. By monitoring and managing uric acid levels, doctors can potentially identify individuals at increased risk for these conditions and implement preventive measures accordingly.
Kidney Health Assessment: The kidneys play a vital role in filtering and excreting uric acid from the body. Persistently high uric acid levels can strain the kidneys and increase the risk of kidney stones and kidney disease. Monitoring uric acid levels can serve as an indicator of kidney function and help doctors assess overall kidney health. Identifying and addressing elevated uric acid levels can potentially slow down the progression of kidney disease and reduce the risk of related complications.
Uncovering Underlying Health Conditions: High uric acid levels may indicate an underlying health condition such as metabolic disorders, insulin resistance, or certain types of cancer. Identifying and treating these conditions in their early stages can significantly improve outcomes. Regular monitoring of uric acid levels can provide doctors with a valuable diagnostic clue, prompting further investigations and ensuring timely intervention.
Lifestyle Modification and Patient Education: Monitoring uric acid levels can empower doctors to educate their patients about lifestyle modifications that can help maintain healthy levels. By discussing dietary choices, weight management, alcohol consumption, and the importance of staying hydrated, doctors can assist individuals in making informed decisions and adopting healthier habits to control uric acid levels.
Ketogenic Diet and Uric Acid Levels: Recent studies have indicated that adopting a ketogenic diet, which is low in carbohydrates and high in healthy fats, can contribute to lowering uric acid levels and improving metabolic health. The ketogenic diet promotes weight loss, reduces insulin resistance, and enhances the body’s ability to burn fat for fuel. These metabolic changes can lead to a decrease in uric acid production and improved uric acid clearance from the body.
By recommending a ketogenic diet to patients with elevated uric acid levels, doctors can potentially help them achieve metabolic health and reduce the risk of developing gout, hypertension, cardiovascular disease, and other metabolic disorders. However, it’s important to note that dietary changes should be tailored to individual needs and medical history, and consultation with a healthcare professional is crucial before starting any new dietary regimen.
In conclusion, monitoring uric acid levels goes beyond the management of gout. With growing evidence linking elevated uric acid levels to various health conditions, it is essential for doctors to pay attention to their patients’ uric acid levels during routine medical care. By doing so, doctors can prevent and manage gout, identify individuals at risk for other health conditions,
assess kidney health, uncover underlying medical issues, and promote overall metabolic health. Adopting a ketogenic diet, in conjunction with regular monitoring of uric acid levels, can be a valuable tool in achieving these goals.
It is important to emphasize that any dietary changes, including the adoption of a ketogenic diet, should be done under the guidance of a healthcare professional. They can assess the individual’s medical history, evaluate potential risks and benefits, and provide personalized recommendations. Additionally, it’s crucial to consider the overall nutritional balance and adequacy of the diet to ensure that all essential nutrients are obtained.
In summary, by recognizing the broader health implications of elevated uric acid levels and monitoring them regularly, doctors can play a crucial role in preventing and managing gout, identifying underlying health conditions, and promoting optimal metabolic health. Alongside other lifestyle modifications, such as dietary changes, adopting a ketogenic diet can be a valuable approach to lower uric acid levels and improve overall health outcomes. Working in partnership with a healthcare professional, individuals can take proactive steps toward achieving better health and well-being.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Importance of Sleep Health: Optimizing Your Rest for Overall Well-being
- June 14, 2023
- Sharon Lojun, M.D., M.S.
- No Comments
Getting quality sleep is essential for our overall health and well-being. It not only affects our physical health but also has a significant impact on our mental and emotional well-being. In this article, we’ll explore the importance of sleep health and discuss various factors that can influence the quality of our sleep.
Adaptive and Maladaptive Cortisol: The Impact of Stress Hormones Cortisol, commonly known as the stress hormone, plays a crucial role in our sleep-wake cycle. In healthy individuals, cortisol levels naturally rise in the morning to help us wake up and stay alert throughout the day. However, problems arise when cortisol levels become dysregulated, leading to maladaptive responses that can disrupt our sleep patterns. Excessive exposure to stress, screen time, and constant alerts can exacerbate cortisol levels, making it challenging to unwind and fall asleep at night.
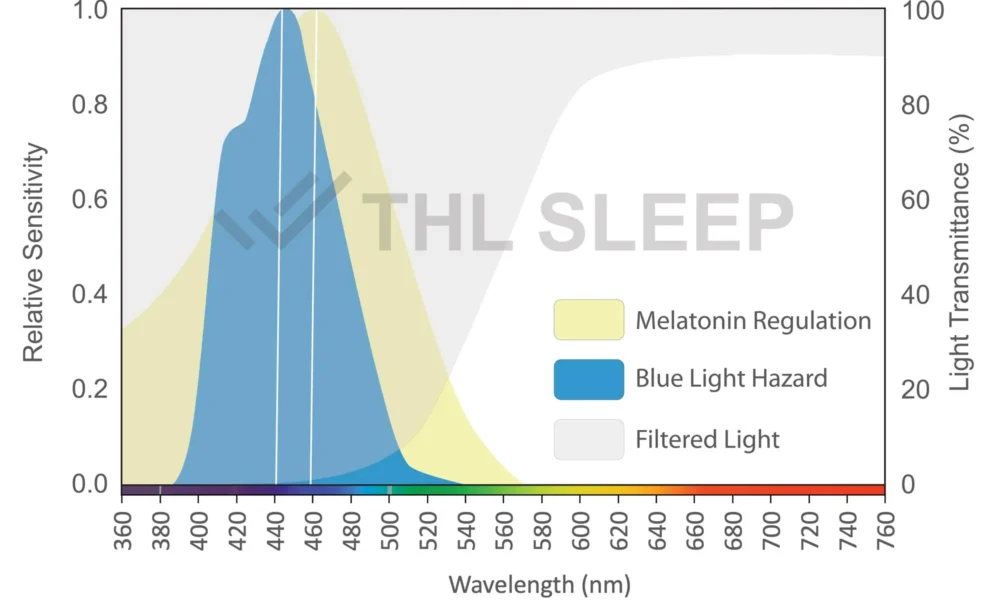
Blue Light and Silence: Creating a Sleep-Conducive Environment In today’s digital age, we are constantly exposed to screens emitting blue light, which can interfere with our natural sleep rhythms. To counteract this, it’s beneficial to establish a blue light curfew by avoiding screens for at least an hour before bed. Additionally, creating a quiet and peaceful environment can help signal to your body that it’s time to rest. Consider incorporating relaxation techniques such as meditation or gentle stretching before bedtime to promote a calm state of mind.
Sleep Problems and Night Shifts: Finding Balance Night shift work can disrupt our body’s natural circadian rhythm, making it difficult to achieve restful sleep during the day. If you find yourself working night shifts, it’s crucial to prioritize your sleep by creating a dark and quiet sleeping environment. Invest in blackout curtains or a sleep mask to block out sunlight, and use earplugs or white noise machines to minimize distractions. Establishing a consistent sleep schedule, even on your days off, can also help regulate your body’s internal clock.
Mental Health and Sleep: A Bidirectional Relationship The relationship between mental health and sleep is bidirectional – poor sleep can contribute to mental health issues, and mental health issues can disrupt sleep patterns. If you’re experiencing difficulties sleeping due to stress, anxiety, or depression, it’s essential to address these underlying concerns. Seek support from healthcare professionals who can help you develop coping strategies, such as cognitive-behavioral therapy for insomnia (CBT-I), which can improve both sleep and mental well-being.
Exercise Patterns: Promoting Restful Sleep Regular exercise can significantly impact the quality of our sleep. Engaging in physical activity, especially earlier in the day, can help regulate our body’s internal clock and promote restful sleep at night. However, intense exercise close to bedtime may have stimulating effects, making it harder to fall asleep. Find a balance that works for you and consider incorporating activities such as yoga, stretching, or low-impact exercises in the evening to unwind and prepare your body for a good night’s sleep.
In conclusion, prioritizing sleep health is crucial for our overall well-being. By understanding the impact of cortisol, implementing strategies to reduce screen time and exposure to blue light, and creating a sleep-conducive environment, we can improve our sleep quality. Additionally, recognizing the challenges of night shifts, addressing mental health concerns, and incorporating exercise patterns that support restful sleep can all contribute to a healthy sleep routine.
Remember, sleep is a vital component of a healthy lifestyle, and if you consistently struggle with sleep problems, it’s important to consult with a healthcare professional who can provide personalized guidance and support.
Author: Sharon Lojun, M.D., M.S.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Probiotics as Adjunctive Treatment for Depression: A Promising Frontier
- May 28, 2023
- Stephen Fitzmeyer, MD
- No Comments
Introduction
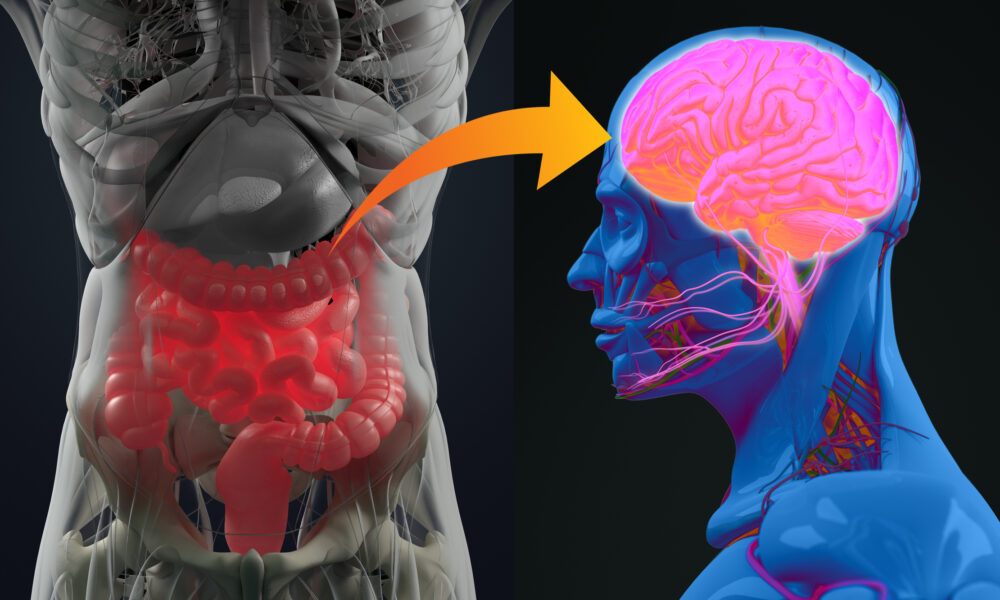
Depression is a prevalent and debilitating mental health disorder that affects millions of people worldwide. While current treatment options such as antidepressant medication and psychotherapy can be effective, a significant proportion of individuals with depression do not experience a satisfactory response. This has led researchers to explore novel approaches to treatment, and one such area of investigation is the use of probiotics. Probiotics, which are live microorganisms that confer health benefits when consumed, have shown promise in influencing the microbiota-gut-brain axis and improving depressive symptoms. A recent pilot randomized clinical trial published in JAMA Psychiatry by Nikolova et al. (2023) investigated the acceptability, tolerability, and potential efficacy of probiotics as an adjunctive treatment for depression. The study’s findings shed light on the potential benefits of probiotics and provide a basis for further investigation in larger efficacy trials.
Study Overview
The study conducted by Nikolova et al. included 49 participants with major depressive disorder (MDD) who had an incomplete response to antidepressant medication. The participants were randomly assigned to receive either a multistrain probiotic or a placebo in addition to their ongoing antidepressant treatment. The trial lasted for 8 weeks, during which the researchers assessed various outcomes, including depressive and anxiety symptoms, treatment adherence, tolerability, and adverse reactions.
Key Findings
The results of the study revealed several important findings. Firstly, the probiotic group demonstrated greater improvements in depressive and anxiety symptoms compared to the placebo group. This was evident from the reduction in scores on rating scales such as the Hamilton Depression Rating Scale (HAMD-17), Inventory of Depressive Symptomatology (IDS), Hamilton Anxiety Rating Scale (HAMA), and General Anxiety Disorder (GAD-7). Secondly, the probiotic intervention was well-tolerated, with a high adherence rate and no serious adverse reactions reported. The dropout rate was low, further highlighting the acceptability of probiotics as a treatment option. Finally, the effect sizes observed in the probiotic group were moderate, suggesting a potential therapeutic benefit.
Implications and Future Directions
The findings of this pilot trial provide a solid foundation for further investigation of probiotics as adjunctive treatment for individuals with major depressive disorder. The acceptability, tolerability, and estimated effect sizes on key clinical outcomes indicate that probiotics may offer a promising avenue for improving depressive symptoms. However, it is important to note that this study was a pilot trial with a relatively small sample size, and thus, larger efficacy trials are needed to confirm and build upon these preliminary findings.
The potential mechanisms through which probiotics exert their effects on depressive symptoms are still being explored. The microbiota-gut-brain axis is thought to play a crucial role in influencing mood and behavior, and probiotics may modulate this axis by promoting a healthy gut microbiome. Further research is required to elucidate the specific strains and dosages of probiotics that are most effective in treating depression, as well as to identify the patient subgroups that may benefit the most from this intervention.
Conclusion
Depression is a complex and multifaceted condition that demands innovative treatment approaches. The study by Nikolova et al. contributes to the growing body of evidence supporting the potential use of probiotics as adjunctive treatment for depression. The results demonstrate the acceptability, tolerability, and estimated effect sizes of probiotics in improving depressive and anxiety symptoms. These findings underscore the need for larger, well-designed efficacy trials to confirm the therapeutic potential of probiotics and inform clinical practice. If future studies continue to show promising results, probiotics could represent a safe, accessible, and scalable treatment option for individuals with depression, complementing existing interventions and improving patient outcomes.
Reference Article:
Title: Acceptability, Tolerability, and Estimates of Putative Treatment Effects of Probiotics as Adjunctive Treatment in Patients With Depression: A Randomized Clinical Trial Journal: JAMA Psychiatry Date: June 14, 2023
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Eggs: The Superfood for a Ketogenic Diet
- May 21, 2023
- Stephen Fitzmeyer, MD
- No Comments
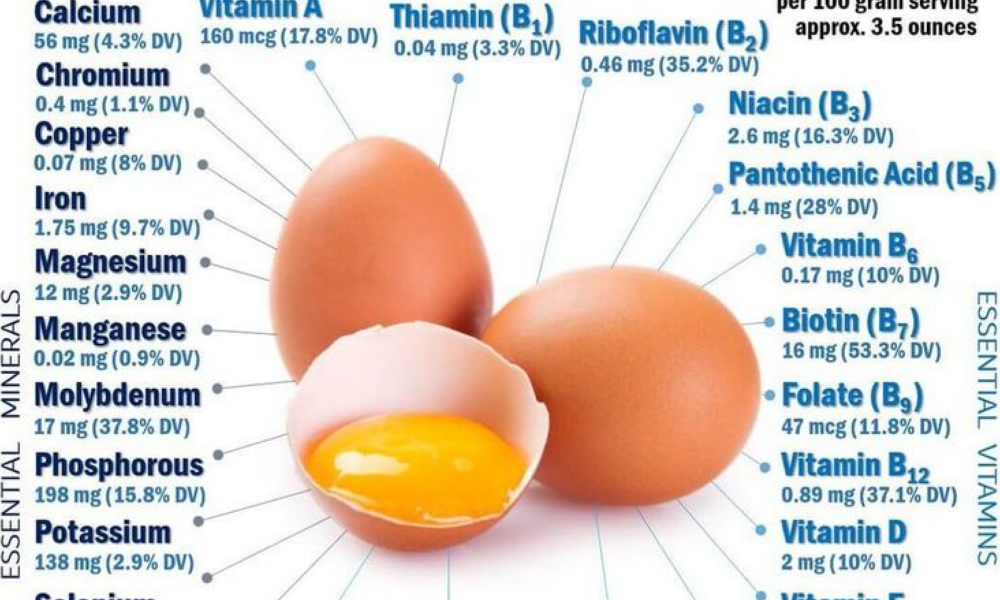
When it comes to the ketogenic diet, few foods are as versatile and beneficial as eggs. These little powerhouses are packed with essential nutrients and can play a significant role in your journey towards achieving ketosis and optimizing your health. From providing high-quality protein to a wealth of vitamins and minerals, eggs offer numerous benefits that make them an ideal choice for those following a ketogenic lifestyle.
Protein Powerhouse: One of the key components of a ketogenic diet is consuming an adequate amount of protein to support muscle growth, repair, and overall health. Eggs are a complete protein source, containing all nine essential amino acids that our bodies need but cannot produce on their own. Adding eggs to your ketogenic meal plan ensures you’re getting a high-quality protein source to nourish your body.
Healthy Fats: While the ketogenic diet is known for its emphasis on fats, it’s crucial to choose healthy sources. Eggs provide a perfect balance of fats, including heart-healthy monounsaturated and polyunsaturated fats. They are also an excellent source of omega-3 fatty acids, which have anti-inflammatory properties and are essential for brain health.
Micronutrient Marvels: Eggs are a nutrient-dense food, offering a wide range of essential vitamins and minerals that support overall well-being. They are rich in:
- Vitamin A: Essential for eye health and immune function.
- Vitamin D: Important for bone health and immune system support.
- Vitamin E: An antioxidant that protects cells from damage.
- Vitamin B12: Vital for brain function and energy production.
- Vitamin B6: Helps convert food into energy and supports brain health.
- Riboflavin (Vitamin B2): Plays a key role in energy metabolism.
- Folate (Vitamin B9): Important for DNA synthesis and cell growth.
- Iron: Essential for oxygen transport and energy production.
- Selenium: Acts as an antioxidant and supports thyroid function.
Appetite Control: One of the advantages of eggs on a ketogenic diet is their ability to keep you feeling full and satisfied. Due to their high protein and healthy fat content, eggs help curb hunger and prevent overeating. Incorporating eggs into your meals can assist in appetite control, making it easier to adhere to your ketogenic eating plan.
Versatility in Cooking: Eggs are incredibly versatile and can be enjoyed in numerous ways. From scrambled and poached to boiled and omelets, there’s a variety of delicious ways to incorporate eggs into your ketogenic meals. You can also use eggs as a binding agent in recipes or create low-carb keto-friendly baked goods.
In addition to their nutritional benefits, eggs offer the advantage of being a food you can enjoy without concern about quantity. Unlike many other foods, you can eat eggs in larger quantities without worrying about derailing your ketogenic goals. Their high protein and healthy fat content make them a satisfying choice that can help you stay on track with your dietary plan.
So go ahead and embrace the wonders of eggs on your ketogenic journey! Enjoy them as part of your meals, snacks, and recipes, knowing that they provide an array of essential nutrients to support your health and well-being. Whether you prefer them scrambled, boiled, or in an omelet, eggs are a guilt-free choice that can be savored without limits.
Remember, if you have any specific health concerns or dietary restrictions, it’s always a good idea to consult with a healthcare professional or registered dietitian for personalized guidance.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
- ‹ Previous
- 1
- 2
- 3
- 4
- Next ›
Recent Posts
- Protected: Warp Core Health: Building a Custom AI Model for Transforming Healthcare
- The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
- Accessing Siloed EMR Systems with FHIR: Connecting to Multiple EMRs
- How AI and Informatics Are Transforming Healthcare
- How AI Can Transform Healthcare Applications
Categories
- ApoB
- Artificial Intelligence
- Autophagy
- Biochemistry
- Biomedical Informatics
- Biostatistics
- Blood Glucose
- CAC
- Carbs
- CCD
- CDA
- Clinical Informatics
- Coding Bootcamp
- Coronary Artery Disease
- COVID-19
- Cybersecurity
- Data Science
- Diabetes
- Diet
- EHS
- EMR
- Epidemiology
- Evidence Based Medicine
- Fats
- FHIR
- Fiber
- Generative AI
- Global Health
- Health Administration
- Health Informatics
- Health IT
- HIPAA
- HL7
- Hyperglycemia
- Hypoglycemia
- ICD 10
- Intermittent Fasting
- Ketogenic Diet
- Machine Learning
- Macronutrients
- MCT Oil
- Metabolic Health
- Metabolic Syndrome
- Minerals
- Mitochondria
- MySQL
- Neurology
- Nutritional Ketosis
- Nutritional Neurology
- Nutritional Psychiatry
- PHP
- PHR
- Programming
- Prompt Engineering
- Proteins
- Prototypes
- Public Health
- Python
- Recipes
- Sleep Health
- Stroke
- Uric Acid
- Vegan and Vegetarians
- Vitamin D
- Vitamin K2
- Vitamins