- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Biochemistry
Unveiling the Role of ApoB and the Therapeutic Potential of Ketogenic Lifestyle and Intermittent Fasting in Atherosclerosis
By Stephen Fitzmeyer, MD
Introduction:
Atherosclerosis, a major contributor to cardiovascular disease, arises from a complex interplay of various factors. Among them, Apolipoprotein B (ApoB) emerges as the primary driver in the development and progression of this condition. In this article, we delve into the critical role of ApoB in atherosclerosis and shed light on the influence of inflammation in enhancing its effects.
Understanding the Role of ApoB:
ApoB, a protein found in lipoproteins such as low-density lipoprotein (LDL) particles, serves as a key player in atherosclerosis. It acts as a carrier, facilitating the transportation of cholesterol to peripheral tissues, including the arterial walls. In the absence of ApoB, the initiation and progression of atherosclerosis are virtually non-existent.
The Significance of ApoB in Atherosclerosis:
ApoB takes center stage in atherosclerosis, as it is responsible for delivering cholesterol-rich lipoproteins, particularly LDL, to arterial walls. These lipoproteins undergo modifications and become trapped in the arterial intima, initiating the formation of fatty streaks. With time, inflammation is triggered, attracting immune cells and accelerating the transformation of fatty streaks into advanced atherosclerotic plaques.
Inflammation and its Role:
While inflammation is a key player in atherosclerosis, it acts as an enhancer rather than the primary driver. Inflammation exacerbates the process by promoting the retention and modification of ApoB-containing lipoproteins, leading to plaque progression and instability. Thus, controlling inflammation becomes crucial in managing atherosclerosis, but addressing the root cause—ApoB—remains essential.
Implications and Therapeutic Strategies:
Understanding the central role of ApoB opens up avenues for therapeutic interventions in managing atherosclerosis. Addressing ApoB levels and reducing the burden of cholesterol-rich lipoproteins is key. Here, lifestyle modifications such as adopting a low-carbohydrate, high-fat diet (such as a ketogenic diet) and implementing intermittent fasting can prove beneficial. These approaches help regulate ApoB-containing lipoproteins, mitigate their retention in arterial walls, and slow down the progression of atherosclerosis.
Furthermore, lifestyle modifications that target additional risk factors associated with atherosclerosis, such as hypertension and obesity, should be considered. Engaging in regular physical activity, maintaining a healthy weight, and managing other comorbidities can complement the efforts to address ApoB and reduce the overall risk of atherosclerosis.
Conclusion:
ApoB stands as the primary driver in the initiation and progression of atherosclerosis, while inflammation serves to enhance and accelerate the process. Recognizing the pivotal role of ApoB provides insights into therapeutic strategies that can mitigate its effects. By adopting lifestyle modifications, such as a low-carbohydrate, high-fat diet and intermittent fasting, individuals can positively influence ApoB levels and manage atherosclerosis. Combining these interventions with measures to address other risk factors offers a comprehensive approach to reducing the burden of atherosclerosis and promoting cardiovascular health.
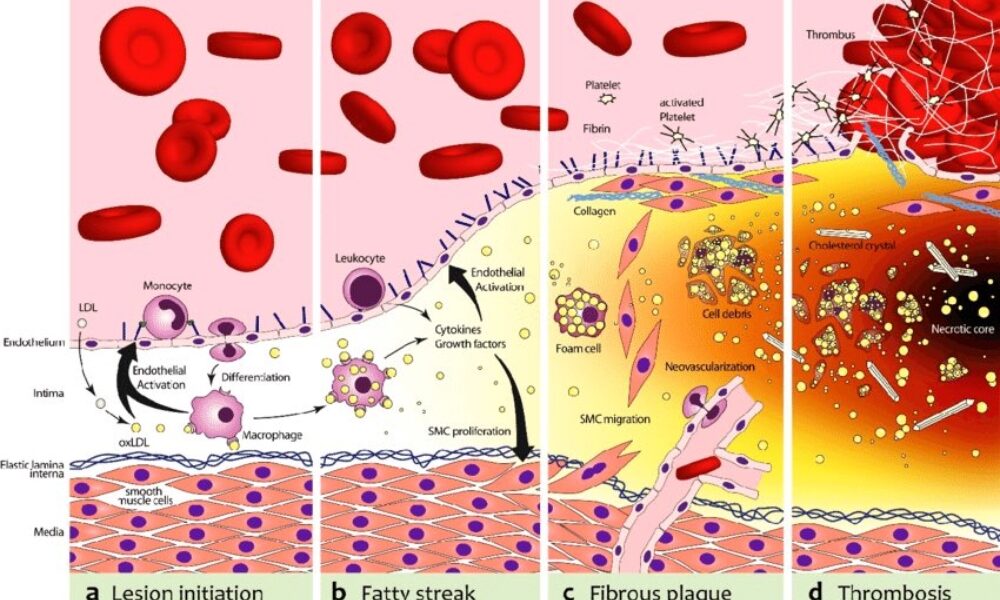
The biochemical pathway of plaque formation involving ApoB can be described as follows:
- ApoB synthesis: ApoB is a protein synthesized in the liver and intestines. It is a major component of very low-density lipoprotein (VLDL) and LDL particles.
- Lipoprotein assembly: VLDL particles are assembled in the liver and contain ApoB-100. They transport triglycerides and cholesterol from the liver to peripheral tissues. During circulation, VLDL particles undergo enzymatic changes, resulting in the conversion of triglycerides into free fatty acids and glycerol.
- LDL formation: As VLDL particles lose triglycerides, they become smaller and denser, transforming into LDL particles. LDL contains a single molecule of ApoB-100 and is the primary carrier of cholesterol in the bloodstream.
- LDL uptake: LDL particles bind to LDL receptors on cell surfaces, allowing the cells to take up cholesterol. These receptors are present in various tissues, including the arterial walls.
- Retention and modification: In the arterial walls, LDL particles can undergo modifications, such as oxidation and glycation, making them more prone to retention. These modified LDL particles interact with extracellular matrix proteins and proteoglycans in the arterial intima, leading to their entrapment within the vessel walls.
- Inflammation and foam cell formation: The retained LDL particles, along with their cholesterol content, trigger an inflammatory response. Immune cells, particularly macrophages, migrate to the site of inflammation. They engulf the cholesterol-rich LDL particles, transforming into foam cells, which are characterized by their lipid-filled cytoplasm.
- Fatty streak formation: The accumulation of foam cells and other immune cells results in the formation of fatty streaks, which are the initial visible signs of plaque development. Fatty streaks consist of foam cells, lipids, inflammatory cells, and smooth muscle cells.
- Advanced plaque formation: Over time, the fatty streaks can progress into more advanced atherosclerotic plaques. These plaques are characterized by a fibrous cap composed of smooth muscle cells and collagen, a lipid-rich core containing foam cells and cholesterol, and a necrotic center.
Throughout this biochemical pathway, ApoB plays a crucial role in the transport of cholesterol to peripheral tissues, including the arterial walls. It facilitates the delivery of cholesterol-rich LDL particles, which, under certain conditions, contribute to the formation of atherosclerotic plaques. Understanding this pathway provides valuable insights into potential therapeutic targets for preventing and managing plaque formation and related cardiovascular diseases.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Biochemical Pathway of Fat Metabolism: Unleashing Ketones as the Ultimate Fuel Source
Introduction:
The human body is a remarkable machine that possesses the ability to adapt and utilize various fuel sources to meet its energy needs. While carbohydrates have traditionally been considered the primary energy source, the biochemical pathway of fat metabolism unlocks a fascinating alternative: the production of ketones. In this article, we will delve into the intricate pathway of fat metabolism and explore how it leads to the production of ketones, making them a potent and efficient fuel source for our bodies.
The Basics of Fat Metabolism:
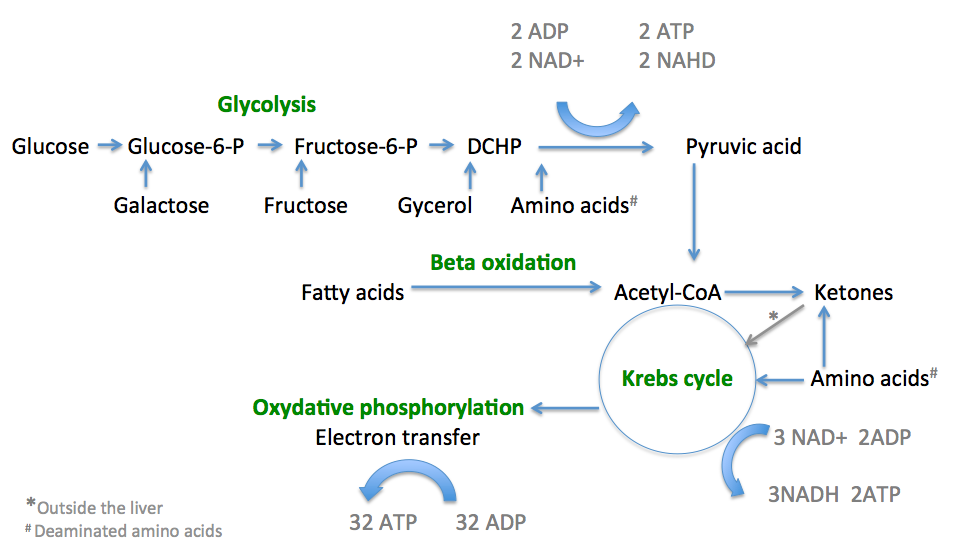
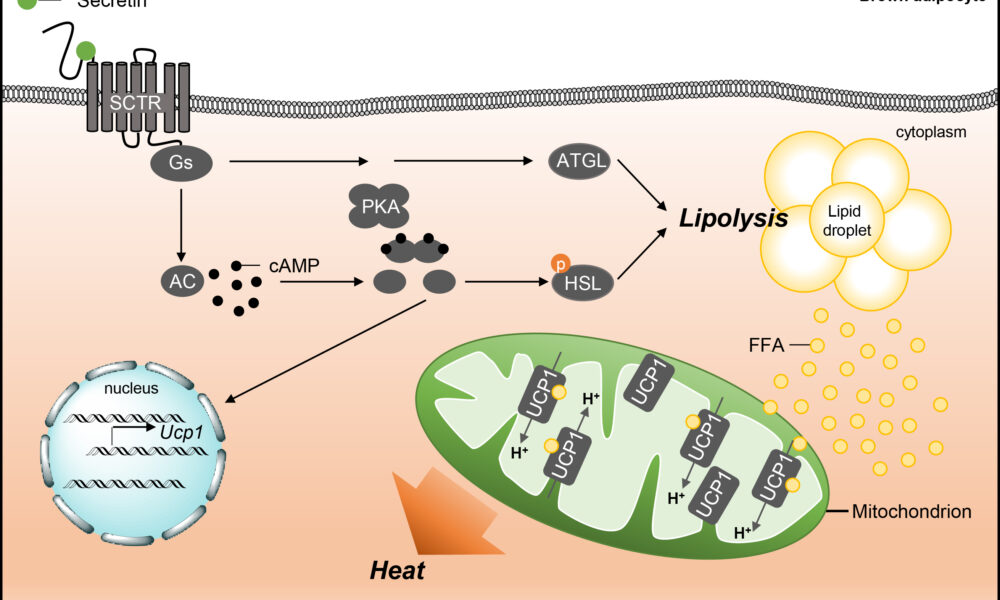
Fat metabolism, also known as lipolysis, is the process by which our bodies break down triglycerides stored in adipose tissue to release fatty acids. This process occurs primarily in the mitochondria, the energy powerhouses of our cells. Through a series of intricate biochemical reactions, fatty acids are converted into acetyl-CoA, which serves as a key precursor in the production of ketone bodies.
The Ketogenic Pathway:
Once fatty acids are converted to acetyl-CoA, they enter the biochemical pathway known as ketogenesis. Ketogenesis occurs predominantly in the liver mitochondria and involves the transformation of acetyl-CoA into ketone bodies. The primary ketone bodies produced are acetoacetate, beta-hydroxybutyrate, and acetone.
Acetoacetate is the first ketone body formed, which can be further converted into beta-hydroxybutyrate or spontaneously decarboxylated to produce acetone. Beta-hydroxybutyrate is the most abundant and readily used ketone body, providing an efficient and sustainable energy source for various tissues, including the brain.
The Role of Ketones as a Primary Fuel Source:
Ketones offer several advantages as a primary fuel source for the body:
- Enhanced Energy Production: Ketones are metabolized more efficiently than glucose, producing a higher yield of ATP (adenosine triphosphate), the cellular energy currency. This increased energy output fuels the body’s cells and supports optimal physiological functions.
- Stable Blood Sugar Levels: Unlike carbohydrates, which can lead to blood sugar spikes and crashes, ketones provide a stable and steady source of energy. This stability helps prevent energy fluctuations, enhances mental clarity, and reduces cravings for quick-fix carbohydrates.
- Preservation of Lean Muscle Mass: When the body enters a state of ketosis, it becomes proficient at utilizing stored fat as its primary fuel source, sparing muscle protein from being broken down for energy. This preservation of lean muscle mass is vital for maintaining overall body composition and metabolic health.
- Neuroprotective Effects: The brain is highly dependent on a consistent energy supply. Ketones serve as an alternative fuel source for the brain when glucose availability is limited. This feature is particularly beneficial in conditions like Alzheimer’s disease, where brain glucose metabolism is impaired.
Conclusion:
The biochemical pathway of fat metabolism that leads to the production of ketones presents a remarkable alternative energy source for our bodies. By harnessing the power of ketones, we can tap into an efficient and sustainable fuel supply that offers numerous benefits, including enhanced energy production, stable blood sugar levels, muscle preservation, and potential neuroprotective effects.
Understanding the intricacies of fat metabolism and the production of ketones sheds light on the potential of adopting a ketogenic diet or incorporating intermittent fasting practices. These approaches can optimize fat metabolism, induce nutritional ketosis, and unlock the full potential of ketones as a primary fuel source.
It is important to note that individual responses to a ketogenic diet may vary, and consulting with a healthcare professional is essential, especially for those with underlying health conditions. With a deeper understanding of the biochemical pathway of fat metabolism and the power of ketones, we can make informed choices to support our metabolic health and overall well-being.
While a ketogenic diet can be a valuable tool for harnessing the benefits of ketones, it’s crucial to approach it with careful consideration. Adhering to a well-formulated ketogenic diet involves consuming adequate healthy fats, moderate protein, and minimal carbohydrates. Individual needs, goals, and potential underlying health conditions should be taken into account when adopting a ketogenic lifestyle.
Incorporating intermittent fasting (IF) alongside a ketogenic diet can further enhance the production and utilization of ketones. IF involves cycling between periods of eating and fasting, allowing the body to tap into its stored fat for energy. This combination of a ketogenic diet and IF can accelerate the transition into ketosis and amplify the metabolic benefits associated with ketone utilization.
However, it’s important to note that a ketogenic diet and IF may not be suitable for everyone. Pregnant or breastfeeding individuals, those with certain medical conditions, and individuals on specific medications should consult with their healthcare providers before making any significant dietary changes.
In conclusion, understanding the biochemical pathway of fat metabolism that leads to the production of ketones unveils the potential of ketones as a primary fuel source for our bodies. By adopting a well-formulated ketogenic diet and potentially incorporating intermittent fasting, we can tap into the benefits of ketones, including enhanced energy production, stable blood sugar levels, muscle preservation, and potential neuroprotective effects.
As with any dietary approach, it is important to listen to our bodies, prioritize nutrient-dense foods, and make informed choices based on individual needs and goals. Whether you choose to embrace a ketogenic diet or explore other nutritional strategies, the knowledge of fat metabolism and ketone production empowers us to optimize our health and unlock the potential of our bodies’ incredible metabolic machinery.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Fats: The Primary Fuel Source, with Sugars as a Backup – Supported by Biochemistry
Introduction:
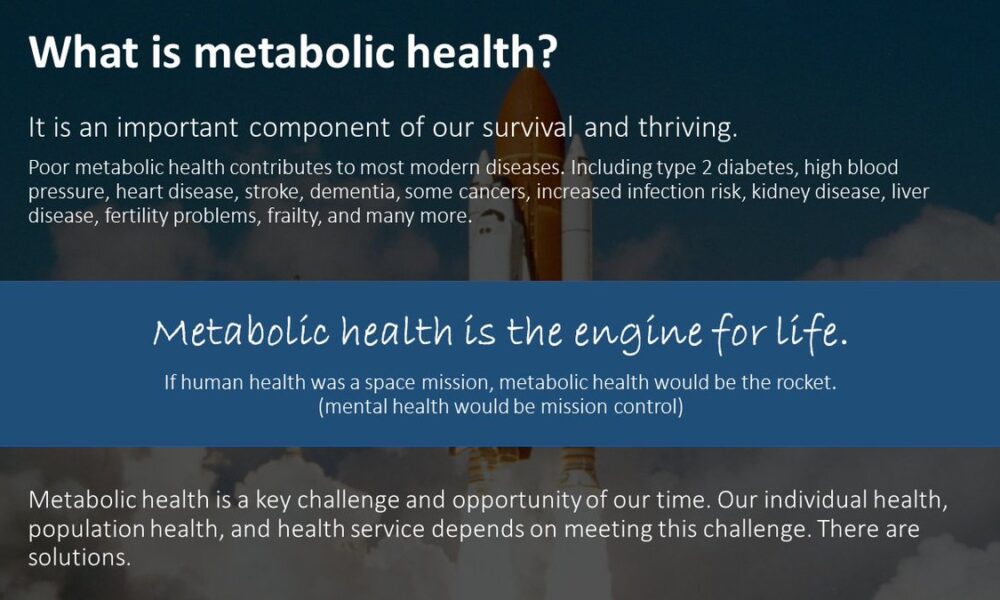
The debate surrounding the optimal fuel source for the human body has garnered significant attention in recent years. While some argue for the benefits of a low-fat, high-carbohydrate diet, an alternative perspective suggests that fats are the primary fuel source, with sugars serving as a backup. In this article, we will present an argument highlighting the advantages of fats as the body’s main energy provider, supported by insights from biochemistry.
- Efficient Energy Release and Sustained Endurance:
Biochemically, fats offer a highly efficient energy source. When compared to carbohydrates, fats contain a higher number of carbon atoms and more than twice the number of calories per gram. Through a process called beta-oxidation, fatty acids are broken down into acetyl-CoA molecules, which enter the citric acid cycle (also known as the Krebs cycle) to produce energy-rich molecules such as ATP.
This metabolic pathway generates a greater amount of ATP per molecule of fat compared to carbohydrates, providing a sustained and long-lasting energy supply. The slow and steady release of energy from fats is particularly beneficial for endurance activities, allowing individuals to maintain performance over extended periods without relying on frequent carbohydrate consumption.
- Stable Blood Sugar Levels and Reduced Insulin Response:
Biochemically, the consumption of fats has minimal impact on blood sugar levels. In contrast, the rapid breakdown of carbohydrates, especially high-glycemic ones, leads to a surge in blood glucose levels. In response, the pancreas releases insulin to facilitate the uptake of glucose into cells, resulting in a temporary increase in energy levels.
However, the subsequent drop in blood sugar levels can lead to fatigue, cravings, and decreased performance. In contrast, fats provide a more stable and sustained release of energy without triggering significant fluctuations in blood sugar levels or requiring large insulin responses.
- Metabolic Adaptation: Ketosis and Fat Adaptation:
Biochemistry also supports the argument that fats can be the primary fuel source through metabolic adaptations such as ketosis and fat adaptation. When carbohydrate intake is limited, the body initiates ketogenesis, a process in which fatty acids are converted into ketone bodies (e.g., acetoacetate, beta-hydroxybutyrate, acetone).
Ketones can cross the blood-brain barrier and serve as an alternative fuel source for the brain, reducing the need for glucose. This adaptation allows individuals to efficiently utilize fats for energy, leading to increased fat oxidation and a decreased reliance on carbohydrates.
Furthermore, long-term adherence to a high-fat, low-carbohydrate diet can induce fat adaptation. This process involves upregulation of enzymes and transporters involved in fat metabolism, enhancing the body’s ability to derive energy from fats and improving endurance performance.
Conclusion:
The biochemistry of fats strongly supports the argument that they can serve as the primary fuel source for the human body. Fats offer efficient energy release, sustained endurance, stable blood sugar levels, and the potential for metabolic adaptations like ketosis and fat adaptation.
While sugars and carbohydrates still have their place in our diet, considering fats as the primary fuel source, supported by biochemistry, can lead to numerous health benefits. It is essential to understand individual needs, goals, and potential underlying health conditions when determining the optimal macronutrient ratios. Ultimately, a balanced approach that prioritizes healthy fat sources and includes sugars as a secondary fuel source can promote overall well-being and performance.
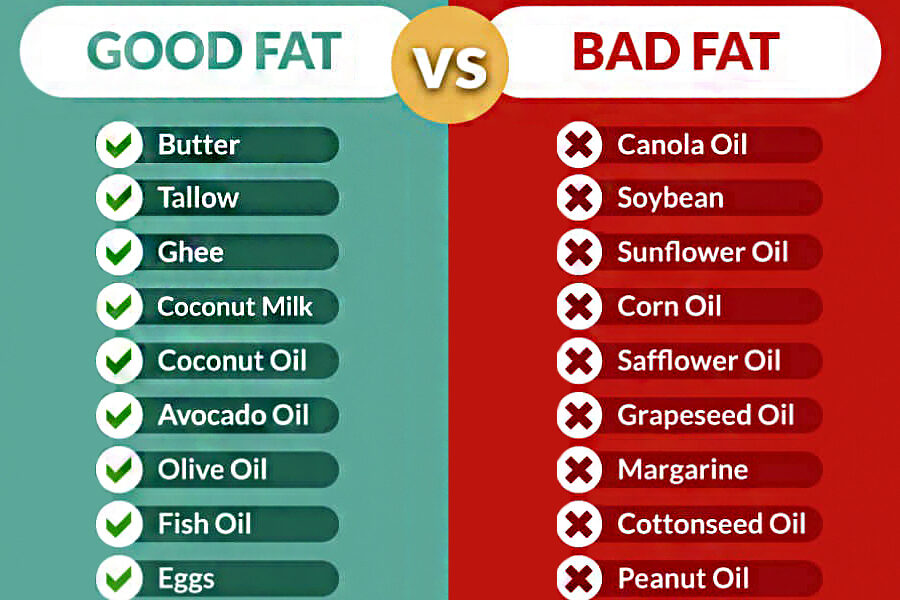
In addition, it is crucial to be aware of the distinction between good fats and bad fats when considering our dietary choices. Good fats, derived from natural sources, provide nourishment and support overall health, while bad fats, commonly found in seed oils, can have negative implications for our well-being.
Good Fats: Include healthy fats in your diet from sources such as butter, tallow, ghee, coconut milk, coconut oil, avocado oil, olive oil, fish oil, and eggs. These fats offer a range of health benefits, including essential nutrients, support for brain function, heart health, and reduced inflammation.
Bad Fats: On the other hand, it is advisable to limit or avoid the consumption of bad fats, particularly seed oils. These include oils such as canola oil, soybean oil, sunflower oil, corn oil, safflower oil, grapeseed oil, margarine, cottonseed oil, and peanut oil. These oils are often highly processed and contain high levels of omega-6 fatty acids, which can promote inflammation and imbalance in the body.
By being mindful of the types of fats we consume, we can make informed choices to support our overall health and well-being. Opt for good fats from natural sources while minimizing the intake of bad fats derived from seed oils. A balanced approach to fat consumption can contribute to an optimized diet and enhance our overall health.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Mitochondria: The Powerhouses that Prefer Fats over Sugars
Introduction:
Mitochondria, the tiny organelles found within our cells, play a crucial role in energy production. They are responsible for converting the food we consume into usable energy in the form of ATP (adenosine triphosphate). While both fats and sugars can serve as fuel sources for our mitochondria, growing evidence suggests that these cellular powerhouses have a preference for utilizing fats as their primary energy substrate. In this article, we will explore the reasons why mitochondria favor fats over sugars for efficient energy production.
- The Efficiency of Fat Oxidation:
Mitochondria exhibit a remarkable efficiency in oxidizing fats compared to sugars. When fatty acids enter the mitochondria, they undergo beta-oxidation, a process that breaks down long-chain fatty acids into smaller units called acetyl-CoA. This acetyl-CoA then enters the citric acid cycle, where it is further metabolized to produce energy-rich molecules such as NADH and FADH2. These molecules are critical for ATP synthesis through oxidative phosphorylation.
The process of fat oxidation generates a greater yield of ATP per molecule compared to the metabolism of sugars. Fats contain more carbon atoms and provide a dense source of energy, supplying a sustained and long-lasting fuel for our cells.
- Mitochondrial Adaptation to Fat Metabolism:
The mitochondria are highly adaptable organelles that can adjust their metabolic machinery based on the available fuel sources. When the body predominantly relies on fats for energy, such as during periods of fasting or a low-carbohydrate diet, mitochondria undergo a process called metabolic flexibility or metabolic switching. This adaptation enables the mitochondria to enhance their capacity to metabolize fats efficiently.
Through increased expression of enzymes and transporters involved in fat metabolism, mitochondria become better equipped to handle fatty acids, ensuring a continuous supply of energy. This adaptation leads to increased mitochondrial biogenesis, the formation of new mitochondria, and improved oxidative capacity, ultimately enhancing fat oxidation as the preferred fuel source.
- Reduced Oxidative Stress and Mitochondrial Health:
Mitochondria have a lower propensity to generate harmful byproducts, such as reactive oxygen species (ROS), during fat oxidation compared to sugar metabolism. When glucose is metabolized, it can result in a higher production of ROS, which can contribute to oxidative stress and damage to cellular components, including mitochondria themselves.
By primarily utilizing fats as a fuel source, mitochondria can reduce the generation of ROS and maintain a healthier environment. This helps to preserve mitochondrial function and integrity, supporting overall cellular health and longevity.
Conclusion:
Mitochondria, the powerhouses of our cells, exhibit a clear preference for utilizing fats over sugars for energy production. The efficiency of fat oxidation, the adaptability of mitochondria to fat metabolism, and the reduced oxidative stress associated with fat utilization all contribute to this preference. By prioritizing fats as a fuel source through dietary choices or strategies like intermittent fasting or a low-carbohydrate diet, we can optimize mitochondrial function and support overall cellular health.
However, it’s important to highlight the remarkable benefits of a ketogenic diet in achieving optimal energy production and overall well-being. While carbohydrates have their role in providing quick bursts of energy and supporting specific bodily functions, a ketogenic diet, which prioritizes fats as the primary fuel source, can have profound effects on our health. By entering a state of ketosis, where the body relies on fat metabolism and produces ketones as an alternative energy source, individuals can experience enhanced fat burning, improved mental clarity, reduced inflammation, and stable energy levels throughout the day. Understanding individual needs and goals can guide the establishment of an optimal macronutrient ratio, allowing individuals to harness the power of ketosis and support their cellular powerhouses in achieving peak performance and well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
- Hoppel, C. (2003). The Role of Carnitine in Normal and Altered Fatty Acid Metabolism. American Journal of Kidney Diseases, 41(4), S4-S12. doi: 10.1016/s0272-6386(03)00003-5
- Kelley, D. E., & Mandarino, L. J. (2000). Fuel Selection in Human Skeletal Muscle in Insulin Resistance: A Replication. Diabetes, 49(5), 677-683. doi: 10.2337/diabetes.49.5.677
- Mootha, V. K., et al. (2003). PGC-1α-responsive Genes Involved in Oxidative Phosphorylation are Coordinately Downregulated in Human Diabetes. Nature Genetics, 34(3), 267-273. doi: 10.1038/ng1180
- Schooneman, M. G., et al. (2013). Fatty Acid Partitioning in the Energetics of the Liver: An Overview and Update. Biochimica et Biophysica Acta (BBA) – Molecular and Cell Biology of Lipids, 1831(12), 169-176. doi: 10.1016/j.bbalip.2013.03.013
- Storlien, L. H., et al. (2004). Adaptation of Muscle Mitochondria to Prolonged Exercise Training. Experimental Physiology, 89(1), 13-22. doi: 10.1113/expphysiol.2003.026203
- Veech, R. L. (2004). The Therapeutic Implications of Ketone Bodies: The Effects of Ketone Bodies in Pathological Conditions: Ketosis, Ketogenic Diet, Redox States, Insulin Resistance, and Mitochondrial Metabolism. Prostaglandins, Leukotrienes and Essential Fatty Acids, 70(3), 309-319. doi: 10.1016/j.plefa.2003.09.007