- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Author: Stephen Fitzmeyer, MD
M.D. with two postdocs in Clinical Informatics, one as the Ruth L. Kirschstein NIH NRSA Informatics Fellows at Boston Medical Center and the other as an Advanced Medical Informatics Fellow at the Boston VA Healthcare system. Dr. Fitzmeyer is the founder of Warp Core Health and Jax Code Academy.
Revolutionizing Healthcare: The Potential Impact of AI
by Stephen Fitzmeyer, MD
Artificial Intelligence (AI) has been making waves in the healthcare industry in recent years, with many experts predicting that it will revolutionize the way healthcare is delivered in the near future. From early disease detection to personalized treatment plans, AI has the potential to transform the healthcare landscape, improving patient outcomes and reducing healthcare costs.
One of the main areas where AI is expected to make a significant impact is in the early detection of diseases. AI algorithms can analyze large amounts of data, such as medical images and genetic information, to identify patterns that may be indicative of a disease. For example, AI-powered imaging tools can help radiologists detect early signs of cancer, heart disease, and other conditions, allowing for earlier diagnosis and more effective treatment.
Another area where AI is expected to make a big impact is in personalized treatment plans. AI algorithms can analyze a patient’s medical history, genetic makeup, and other factors to create personalized treatment plans that are tailored to their specific needs. This can help healthcare providers deliver more effective treatments and reduce the risk of adverse reactions to medications.
AI can also help improve patient outcomes by predicting which patients are at risk of developing certain conditions. For example, AI algorithms can analyze patient data to identify those at high risk of developing diabetes or heart disease. This can help healthcare providers intervene early, providing preventive measures to reduce the risk of these conditions developing.
AI can also be used to improve the efficiency of healthcare delivery. For example, chatbots powered by AI can be used to provide patients with 24/7 access to basic medical information and advice, reducing the need for in-person consultations and freeing up healthcare providers to focus on more complex cases. AI-powered scheduling systems can also help healthcare providers manage their workload more efficiently, reducing waiting times for patients and improving the overall quality of care.
Despite the many potential benefits of AI in healthcare, there are also some challenges that need to be addressed. One of the biggest challenges is ensuring that AI algorithms are accurate and reliable. To achieve this, it is important to ensure that the algorithms are based on high-quality data and that they are regularly tested and updated.
Another challenge is ensuring that AI is used in an ethical and responsible way. This means ensuring that patient data is kept secure and that AI algorithms are not used to discriminate against certain groups of people.
In conclusion, AI has the potential to revolutionize healthcare in numerous ways. From early disease detection to personalized treatment plans, AI can help healthcare providers deliver more effective and efficient care, improving patient outcomes and reducing healthcare costs. However, it is important to address the challenges associated with the use of AI in healthcare to ensure that it is used in an ethical and responsible way.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Essential Fat and Protein Sources for Vegans and Vegetarians on a Keto Diet
By Stephen Fitzmeyer, MD
Introduction: Following a ketogenic diet as a vegan or vegetarian can be challenging, as the focus on high fat and low carb intake requires careful consideration of food choices. However, with a wide range of nutrient-dense options available, it is possible to meet your fat and protein needs while adhering to a plant-based keto lifestyle. In this article, we will explore the best sources of fat and protein for vegans and vegetarians, with a special emphasis on keto-friendly choices.
Avocado: Nature’s Creamy Powerhouse (Keto-friendly) Avocado, the beloved green fruit, is not only a keto-friendly option but also a nutritional powerhouse. Packed with healthy monounsaturated fats, avocados provide a rich and creamy texture to dishes. They are also a source of dietary fiber, vitamins, and minerals, making them an excellent addition to a vegan or vegetarian ketogenic diet.
Nuts and Seeds: Crunchy Delights (Keto-friendly) Nuts and seeds are versatile and satisfying options for obtaining both healthy fats and protein. Almonds, walnuts, cashews, chia seeds, flaxseeds, and hemp seeds are all keto-friendly choices. These crunchy delights are not only great for snacking but can also be incorporated into recipes, such as nut butters or as toppings for salads and smoothies.
Nut and Seed Butters: Spreads of Goodness (Keto-friendly) Nut and seed butters, such as peanut butter, almond butter, and tahini, are delectable spreads that offer a generous dose of healthy fats and protein. They can be enjoyed on their own, added to smoothies, used as a dip for vegetables, or incorporated into keto-friendly baking recipes.
Coconut and Coconut Oil: Tropical Treasures (Keto-friendly) Coconut and its derivatives are keto-friendly options that bring a tropical twist to your meals. Coconut meat, coconut oil, and coconut milk are rich in healthy fats and can be used in various keto recipes, from curries to smoothies. Coconut milk, with its creamy texture, can be a great base for vegan ketogenic dishes.
Olive Oil: Liquid Gold (Keto-friendly) Olive oil, a staple in the Mediterranean diet, is a source of heart-healthy monounsaturated fats. It is ideal for cooking or as a dressing for salads and vegetables, adding flavor and healthy fats to your meals.
Plant-Based Oils: A Flavorful Spectrum (Keto-friendly) Other plant-based oils, such as avocado oil, flaxseed oil, and sesame oil, offer a diverse range of flavors and are excellent sources of healthy fats for a vegan or vegetarian keto diet. These oils can be used for sautéing, roasting, and dressing to enhance the taste and nutritional profile of your dishes.
Legumes: Protein Powerhouses While not strictly keto-friendly due to their higher carb content, legumes such as beans, lentils, and chickpeas are still valuable sources of plant-based protein for vegans and vegetarians. They can be included in moderation, considering individual carb limits and dietary preferences.
Tofu and Tempeh: Plant-Based Protein Staples Tofu and tempeh, derived from soybeans, are versatile plant-based protein sources. They can be used in a variety of dishes, including stir-fries, salads, and curries. These options provide protein while keeping carbohydrate intake relatively low, making them suitable for a vegan or vegetarian keto diet.
Seitan: Meaty Texture, Plant-Based Protein Seitan, made from wheat gluten, is a high-protein option for those following a vegan or vegetarian keto diet. With its meaty texture and ability to absorb flavors, seitan is a versatile ingredient that can be used to create delicious and satisfying plant-based dishes.
Quinoa: The Complete Protein Grain Quinoa, though higher in carbs compared to other options, is a complete protein source that contains all essential amino acids. While it should be consumed in moderation on a ketogenic diet, quinoa can be a nutritious addition to a vegan or vegetarian keto meal plan when carefully portioned.
Conclusion: Maintaining a well-rounded vegan or vegetarian ketogenic diet requires careful consideration of fat and protein sources. Fortunately, there is a wide array of options available that cater to these needs. Avocado, nuts, seeds, coconut, olive oil, plant-based oils, legumes in moderation, tofu, tempeh, seitan, and quinoa (in limited amounts) offer a range of essential fats and protein for individuals following a plant-based keto lifestyle.
Remember to personalize your food choices according to your specific dietary goals and preferences. Consult with a healthcare professional or registered dietitian to ensure that your nutrient intake aligns with your needs and to optimize your health while following a vegan or vegetarian ketogenic diet. Embrace the diversity of these plant-based options, and enjoy the benefits of a well-balanced and nourishing diet.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
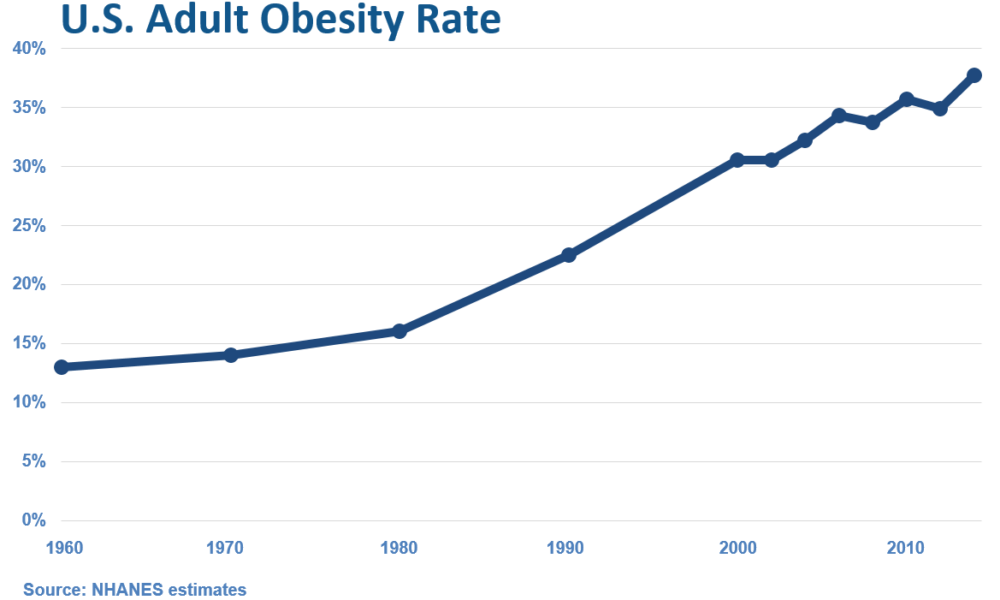
The Rise of Overweight/Obesity in the U.S.: Examining the Influence of Dietary Guidelines, the Food Pyramid, and Ancel Keys
By Stephen Fitzmeyer, MD
Introduction: The United States has experienced a significant increase in overweight and obesity rates over the past few decades, leading to serious health concerns. It is intriguing to examine the correlation between the rise in overweight/obesity and the transformation of the American diet, particularly with the introduction of dietary guidelines and the prominent role played by Ansel Keys. In this article, we delve into the historical context and explore how the shift away from fresh whole foods, influenced by Keys’ research, may have inadvertently contributed to the obesity epidemic in the United States.
The Era of Fresh Whole Foods: Before the introduction of dietary guidelines in the 1980s, the American diet primarily consisted of fresh, whole foods. Meals were often prepared from scratch, using ingredients sourced directly from farms and local markets. Fresh fruits and vegetables, meats, and unprocessed grains were the foundation of everyday eating, providing a nutrient-dense and balanced approach to nutrition.
Ansel Keys and Dietary Fat: Ansel Keys, a prominent scientist, conducted influential research in the mid-20th century that examined the relationship between dietary fat and heart disease. His work, known as the “Seven Countries Study,” suggested a correlation between high-fat diets and increased risk of cardiovascular issues. However, Keys’ study focused on selected countries, disregarding nations with contrasting dietary patterns that contradicted his findings.
The Impact of Keys’ Findings: Keys’ research gained significant attention and led to a shift in nutritional thinking. Dietary fat, particularly saturated fat, became vilified, and the notion that a low-fat diet was crucial for maintaining heart health took root. As a result, dietary guidelines and recommendations began emphasizing the reduction of fat intake, leading to the promotion of low-fat and fat-free products in the market.
The Emergence of Processed Foods: The low-fat movement led to a surge in processed food products marketed as healthy alternatives. With the focus on reducing fat, manufacturers started formulating products with reduced fat content but compensated by adding excessive amounts of sugar, artificial additives, and refined carbohydrates. This shift in the food industry coincided with the introduction of dietary guidelines, further driving the consumption of processed foods among Americans.
Unintended Consequences: The shift away from fresh whole foods towards processed, low-fat alternatives had unintended consequences. These processed foods were often calorie-dense, nutrient-poor, and contributed to overconsumption. The replacement of dietary fats with refined carbohydrates and added sugars not only affected overall calorie intake but also disrupted metabolic processes, leading to weight gain and related health issues.
Reevaluating Dietary Choices: In recent years, there has been a growing realization that the previous low-fat paradigm may have played a role in the obesity epidemic. Many experts advocate for a return to a more balanced approach, focusing on the consumption of whole, unprocessed foods and reevaluating the role of dietary fats. This includes embracing healthy fats such as those found in avocados, nuts, olive oil, fatty meats, eggs, butter, and cheeses.
Empowering Individuals through Education: To combat the rise of overweight/obesity, it is essential to empower individuals with knowledge and encourage them to make informed dietary choices. By educating ourselves about the benefits of fresh whole foods, understanding the potential pitfalls of processed foods, and reevaluating the role of dietary fats, we can make strides towards improving our overall health and well-being.
Conclusion: The rise of overweight and obesity in the United States coincides with the transformation of the American diet, influenced by the introduction of dietary guidelines and the impact of Ansel Keys’ research. While Keys’ findings had noble intentions, the emphasis on low-fat diets and the
proliferation of processed, low-fat alternatives may have inadvertently contributed to the obesity epidemic. It is important to acknowledge the historical context and the role played by fresh whole foods in the American diet before the era of dietary guidelines. By revisiting and embracing a diet centered around whole, unprocessed foods, we can reclaim a healthier approach to nutrition.
Moving forward, it is crucial to continue educating individuals about the importance of a balanced diet that includes nutrient-dense foods and minimizes reliance on processed and refined options. By fostering a culture of mindful eating and promoting the consumption of fresh, whole foods, we can work towards reversing the alarming trends of overweight and obesity and promoting a healthier future for all.
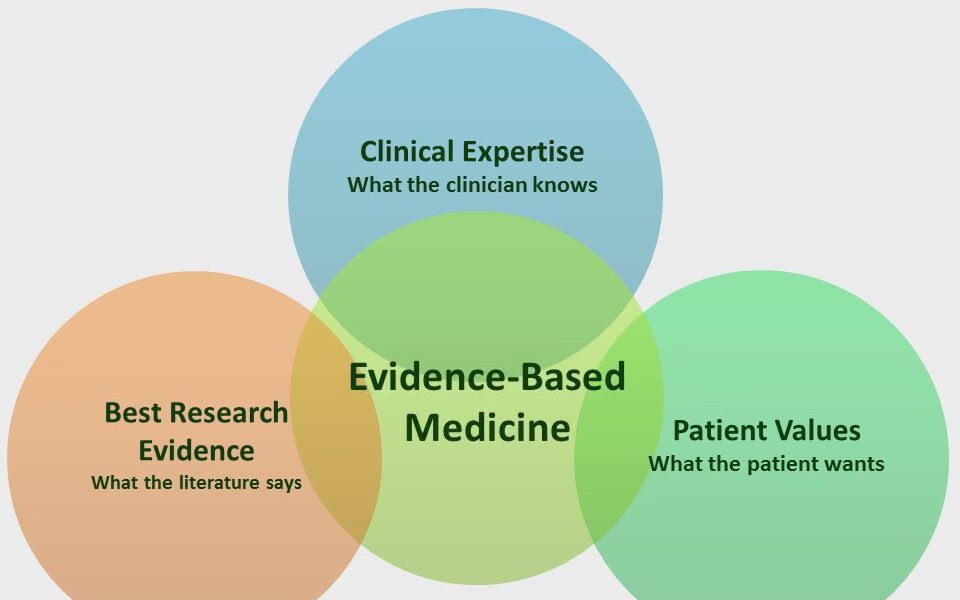
Coding Evidence-Based Medicine into Web-Based Applications
By Stephen Fitzmeyer, MD
Evidence-based medicine (EBM) is a medical approach that involves using the best available evidence to make informed clinical decisions. The goal of EBM is to improve the quality of patient care by integrating research evidence, clinical expertise, and patient preferences into clinical decision making. In recent years, there has been a growing interest in using technology to support EBM and help clinicians make evidence-based decisions. Web-based applications are a popular way to accomplish this goal.
Web-based applications that incorporate EBM can provide clinicians with easy access to the latest research evidence, as well as clinical practice guidelines and other relevant resources. These applications can help clinicians make informed decisions about diagnosis, treatment, and management of a wide range of medical conditions.
The process of building a web-based EBM application involves several steps. The first step is to identify the target audience and determine the specific clinical needs that the application will address. This may involve conducting a needs assessment and identifying gaps in current clinical practice.
The second step is to identify relevant EBM resources and integrate them into the application. This may involve using electronic databases, such as PubMed or Cochrane Library, to search for the latest research evidence. It may also involve incorporating clinical practice guidelines, systematic reviews, and other evidence-based resources into the application.
Once the relevant EBM resources have been identified, the next step is to design the application’s user interface. The application should be easy to navigate, intuitive to use, and provide users with relevant information at the appropriate time. The design of the application should be based on user-centered design principles, which involve actively involving users in the design process and incorporating their feedback into the final product.
After the application has been designed, the next step is to develop the application using web development languages and frameworks such as HTML, CSS, JavaScript, and React. The application may also incorporate server-side programming languages such as PHP or Python, and databases such as MongoDB or MySQL to store and retrieve data.
Finally, the application should be tested and validated to ensure that it is functioning as intended and providing accurate and reliable information to users. This may involve user testing, where the application is tested by actual users, as well as usability testing, where the application is tested for ease of use and effectiveness.
In conclusion, web-based applications that incorporate EBM can provide clinicians with easy access to the latest research evidence and clinical practice guidelines, helping them make informed decisions about patient care. The development of these applications involves identifying the target audience and their clinical needs, integrating relevant EBM resources, designing an intuitive user interface, developing the application using web development languages and frameworks, and testing and validating the application to ensure that it is effective and reliable. By following these steps, developers can build web-based EBM applications that improve patient care and support evidence-based decision making in clinical practice.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
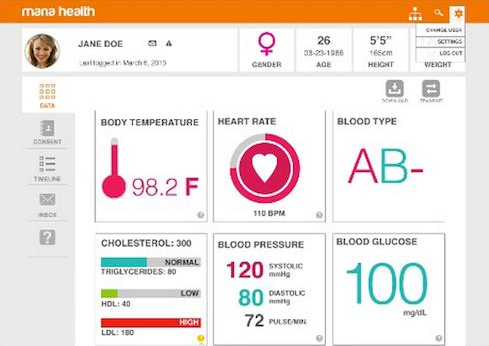
A Step-by-Step Guide to Coding a Personal Health Record
By Stephen Fitzmeyer, MD
A personal health record (PHR) is a digital tool that allows individuals to maintain and manage their health information in a secure and accessible way. PHRs can be created by healthcare providers or individuals themselves. In this article, we will discuss the steps to coding a PHR.
Step 1: Define the data model
The first step in coding a PHR is to define the data model. This involves identifying the different types of health information that will be stored in the PHR. The data model should include the patient’s demographic information, medical history, medications, allergies, immunizations, laboratory results, and other relevant health information. The data model should also define the relationships between different types of information.
Step 2: Choose a programming language
The next step is to choose a programming language for coding the PHR. There are many programming languages to choose from, including Java, Python, Ruby, and PHP. The choice of programming language will depend on the developer’s expertise, the features required, and the platform on which the PHR will be deployed.
Step 3: Design the user interface
The user interface (UI) is the part of the PHR that patients will interact with. The UI should be intuitive and easy to use. It should allow patients to input and view their health information, as well as update and share it with healthcare providers. The design of the UI should be based on best practices for user experience (UX) and accessibility.
Step 4: Develop the back-end
The back-end of the PHR is the part of the application that handles the storage and retrieval of data. The back-end should be designed to ensure the security and confidentiality of patient health information. It should also be scalable and efficient, to handle large volumes of data and support future expansion.
Step 5: Integrate with other systems
PHRs need to integrate with other healthcare systems, such as electronic health records (EHRs), health information exchanges (HIEs), and patient portals. Integration with these systems will allow patients to access their health information from different sources, and share it with healthcare providers as needed.
Step 6: Test and deploy
Before deploying the PHR, it is essential to test it thoroughly to ensure that it works as expected and meets the needs of patients and healthcare providers. Testing should include functionality testing, performance testing, security testing, and user acceptance testing. Once testing is complete, the PHR can be deployed on a secure platform, such as a cloud-based server or a local server.
Conclusion
Coding a PHR requires careful planning and attention to detail. By following the steps outlined in this article, developers can create a PHR that is secure, scalable, and user-friendly. A well-designed PHR can empower patients to take control of their health information, improve healthcare outcomes, and support the delivery of personalized and coordinated healthcare services.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
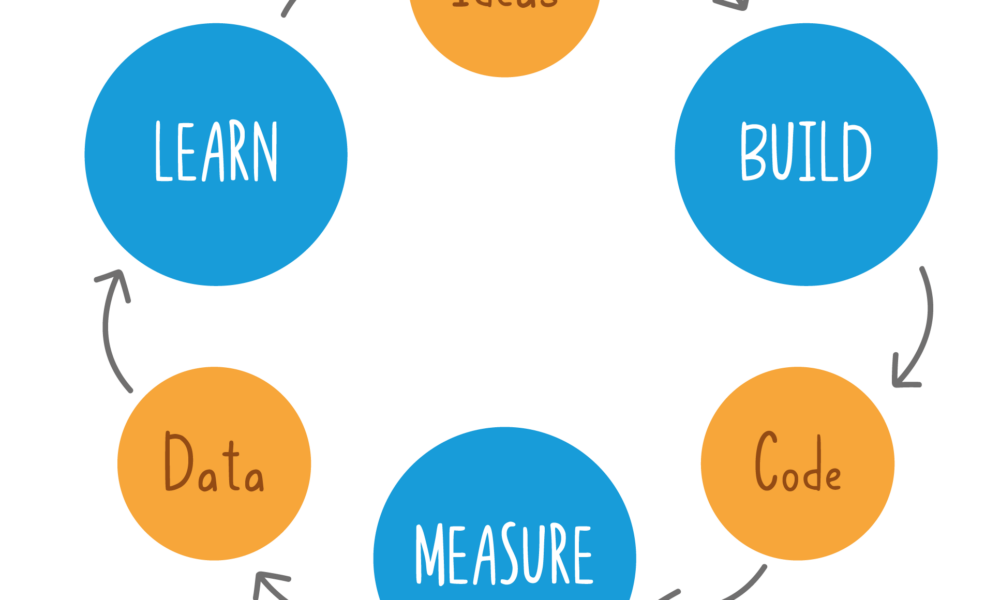
Building Prototypes for Healthcare Using HTML, CSS, JavaScript, PHP, React, Python, MongoDB, and MySQL
By Stephen Fitzmeyer, MD
Building prototypes is an essential step in the healthcare software development process. It allows developers to test and refine their ideas, improve user experience, and identify potential issues before investing significant time and resources into building a fully functional application. In this article, we will discuss how to build prototypes for healthcare using HTML, CSS, JavaScript, PHP, React, Python, MongoDB, and MySQL.
HTML, CSS, and JavaScript
HTML, CSS, and JavaScript are the three fundamental technologies used to build prototypes for web applications. HTML is used to define the structure and content of web pages, CSS is used to style and format the pages, and JavaScript is used to add interactivity and functionality. These technologies are used to create the front-end of a web application, which is the part of the application that users interact with.
PHP
PHP is a server-side scripting language that is used to build dynamic web applications. It is commonly used in healthcare software development to build web applications that interact with databases and other server-side components. PHP is used to create the back-end of a web application, which is the part of the application that is responsible for processing user input, interacting with databases, and generating dynamic content.
React
React is a popular front-end JavaScript library that is used to build user interfaces. It is used to create interactive and responsive user interfaces that can be easily updated and modified. React is commonly used in healthcare software development to build web applications that provide a modern and user-friendly interface.
Python
Python is a versatile programming language that is widely used in healthcare software development. It is used to build server-side components, machine learning models, data analysis tools, and more. Python is commonly used in healthcare software development to build web applications that perform complex data analysis and provide advanced features such as natural language processing and machine learning.
MongoDB and MySQL
MongoDB and MySQL are two popular database management systems used in healthcare software development. MongoDB is a document-based NoSQL database that is used to store and retrieve large amounts of unstructured data. MySQL is a relational database management system that is used to store and retrieve structured data. Both databases are commonly used in healthcare software development to store patient data, medical records, and other healthcare-related information.
Conclusion
Building prototypes for healthcare using HTML, CSS, JavaScript, PHP, React, Python, MongoDB, and MySQL is an effective way to test and refine healthcare software ideas before investing significant time and resources into building a fully functional application. By using these technologies, healthcare software developers can create modern and user-friendly web applications that provide advanced features such as data analysis, machine learning, and natural language processing. With the right tools and skills, healthcare software developers can build prototypes that provide value to patients, healthcare providers, and healthcare organizations.
The Role of Health Informatics in Healthcare: Why Healthcare Providers Should Become Proficient
by Stephen Fitzmeyer, MD
Health informatics is a rapidly growing field that combines healthcare, information technology, and data analysis to improve the quality and efficiency of healthcare delivery. It involves the use of technology and information systems to collect, store, and analyze patient data, enabling healthcare providers to make informed decisions about patient care. In this article, we will discuss what health informatics is, how it is useful, and why healthcare providers should become proficient in it.
What is Health Informatics?
Health informatics is the field of study that focuses on the use of technology and information systems to manage healthcare data. It involves the collection, storage, analysis, and dissemination of healthcare data to support decision-making in healthcare delivery. Health informatics professionals are responsible for developing and implementing information systems that support healthcare providers in delivering high-quality care to patients.
How is Health Informatics Useful?
Health informatics is useful in healthcare in several ways. First, it enables healthcare providers to collect and store patient data electronically, reducing the risk of errors and improving the accuracy of patient records. This also allows for easier and faster access to patient data, enabling healthcare providers to make informed decisions about patient care.
Second, health informatics facilitates communication and collaboration among healthcare providers. Electronic health records (EHRs) and other health information systems allow healthcare providers to share patient data with each other, enabling them to work together more effectively to develop and implement treatment plans.
Third, health informatics supports evidence-based practice. By analyzing patient data, healthcare providers can identify patterns and trends that can inform clinical decision-making and improve patient outcomes. Health informatics also enables healthcare providers to access the latest research and best practices, supporting evidence-based practice.
Why Should Healthcare Providers Become Proficient in Health Informatics?
Healthcare providers should become proficient in health informatics for several reasons. First, proficiency in health informatics enables healthcare providers to make informed decisions about patient care. By understanding how to access and analyze patient data, healthcare providers can develop treatment plans that are tailored to individual patient needs and are based on the latest research and best practices.
Second, proficiency in health informatics supports collaboration and communication among healthcare providers. By understanding how to use health information systems, healthcare providers can share patient data with each other more effectively, enabling them to work together to develop and implement treatment plans.
Third, proficiency in health informatics supports the transition to value-based care. As healthcare moves towards a value-based care model, healthcare providers need to understand how to use health information systems to collect and analyze data on patient outcomes. By understanding how to use health informatics to support evidence-based practice and measure patient outcomes, healthcare providers can demonstrate the value of their services and improve patient outcomes.
In conclusion, health informatics is a rapidly growing field that plays a critical role in healthcare delivery. Healthcare providers who become proficient in health informatics can improve the quality and efficiency of healthcare delivery, supporting evidence-based practice and the transition to value-based care. By investing in health informatics education and training, healthcare providers can position themselves to provide high-quality care and improve patient outcomes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unveiling the Mathematics of Epidemiology: Analyzing Disease Patterns and Prevention Strategies
Epidemiology, the scientific study of health and disease distribution in populations, is a field that relies on mathematical concepts and analysis to understand and combat public health challenges. In this article, we will explore some key mathematical examples that highlight the significance of epidemiology in healthcare.
Incidence and Prevalence: Let’s consider a hypothetical population of 10,000 individuals. Over the course of one year, 500 new cases of a particular disease are diagnosed. The incidence of the disease in this population would be calculated as follows:
Incidence = (Number of new cases / Total population) x 1,000 Incidence = (500 / 10,000) x 1,000 Incidence = 50 cases per 1,000 population
Prevalence, on the other hand, measures the proportion of individuals with the disease at a specific point in time. If, at the beginning of the year, there were already 200 existing cases in the population, the prevalence of the disease would be:
Prevalence = (Number of existing cases / Total population) x 1,000 Prevalence = (200 / 10,000) x 1,000 Prevalence = 20 cases per 1,000 population
These calculations provide healthcare providers with valuable information about the disease burden and help in identifying trends and potential risk factors.
Risk Factors: Let’s consider a study examining the relationship between smoking and the development of lung cancer. Researchers gather data from a sample of 1,000 individuals, finding that 300 of them are smokers and 100 of those smokers develop lung cancer over a five-year period. The incidence rate of lung cancer among smokers can be calculated as:
Incidence Rate = (Number of new cases among smokers / Total number of smokers) x 1,000 Incidence Rate = (100 / 300) x 1,000 Incidence Rate = 333.33 cases per 1,000 smokers
This example demonstrates how epidemiology can quantify the association between a specific risk factor (smoking) and the occurrence of a disease (lung cancer).
Outbreak Investigation: During an outbreak investigation, data collection and analysis are crucial for identifying the source and mode of transmission of a disease. Let’s say there is an outbreak of a foodborne illness, and investigators collect information from 500 affected individuals. By analyzing the data, they find that 400 of them consumed a particular brand of contaminated food. This finding suggests a potential association between the contaminated food and the outbreak.
Screening: To illustrate the importance of screening, let’s consider a population of 2,000 individuals eligible for a breast cancer screening program. The screening test has a sensitivity of 90% and a specificity of 95%. Out of the 50 individuals who have breast cancer, 45 will test positive (true positives) while 5 will test negative (false negatives). Out of the 1,950 individuals without breast cancer, 1,852 will test negative (true negatives) while 98 will test positive (false positives). These numbers highlight the trade-off between identifying true cases of breast cancer and the potential for false-positive results.
Clinical Trials: Clinical trials rely on statistical analysis to assess the effectiveness of new treatments or interventions. For instance, a study involving 500 participants might randomly assign half of them to receive a new medication while the other half receives a placebo. By comparing the outcomes between the two groups, researchers can determine the efficacy of the medication and make evidence-based decisions regarding its use in clinical practice.
By understanding these mathematical examples within the context of epidemiology, healthcare providers can gain valuable insights into the distribution and determinants of diseases. This knowledge enables them to develop effective prevention and control strategies, improve population health outcomes,
and make informed decisions in healthcare. The application of mathematics in epidemiology provides a quantitative framework for understanding the patterns and dynamics of diseases within populations.
Mathematics allows us to quantify the incidence and prevalence of diseases, providing a measure of the disease burden and helping healthcare providers allocate resources effectively. By calculating incidence rates, we can assess the risk factors associated with diseases, such as the relationship between smoking and lung cancer.
During outbreaks, mathematical analysis helps investigators identify the source and mode of transmission of diseases, guiding public health interventions to prevent further spread. Screening programs utilize mathematical concepts to evaluate the performance of tests, balancing the need for early detection with the risk of false positives.
Clinical trials, powered by statistical analysis, provide evidence-based information on the efficacy and safety of new treatments. Mathematics helps determine sample sizes, assess treatment outcomes, and draw valid conclusions about the effectiveness of interventions.
The integration of mathematics in epidemiology strengthens the foundation of public health decision-making. It allows healthcare providers to make data-driven assessments, identify high-risk populations, implement targeted interventions, and monitor the impact of preventive measures.
As we continue to navigate the challenges of disease prevention and control, understanding the role of mathematics in epidemiology is paramount. By harnessing the power of numbers, healthcare providers can effectively analyze and interpret health data, paving the way for evidence-based strategies that protect and promote the well-being of populations.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Understanding the Fundamental Concepts of Epidemiology in Healthcare
By Stephen Fitzmeyer, MD
Epidemiology is the study of the distribution and determinants of health and disease in populations. It is a critical field in healthcare that helps healthcare providers understand the patterns and causes of diseases and develop strategies to prevent and control them. In this article, we will discuss some of the fundamental concepts of epidemiology in healthcare.
Incidence and Prevalence: Incidence is the number of new cases of a disease in a population over a specified period of time. Prevalence is the proportion of individuals in a population with a particular disease at a given point in time. These measures help healthcare providers understand the burden of a disease in a population and the risk factors associated with it.
Risk Factors: Risk factors are the characteristics or behaviors that increase the likelihood of developing a disease. They can be divided into two categories: modifiable and non-modifiable. Modifiable risk factors, such as smoking and poor diet, can be changed to reduce the risk of developing a disease. Non-modifiable risk factors, such as age and genetics, cannot be changed.
Outbreak Investigation: When a disease outbreak occurs, it is important to investigate the outbreak to determine the source of the disease and prevent further spread. Outbreak investigations involve identifying the affected population, collecting data on the disease, and analyzing the data to identify the source and mode of transmission of the disease.
Screening: Screening is the process of testing individuals who do not have any symptoms of a disease to identify those who may be at risk. Screening tests are used to detect diseases at an early stage when treatment is most effective. However, screening tests can also have risks, such as false-positive results, which can lead to unnecessary interventions and anxiety.
Clinical Trials: Clinical trials are research studies that evaluate the safety and effectiveness of new treatments or interventions. They are critical in healthcare as they provide evidence-based information on the efficacy and safety of treatments, which can inform clinical practice.
Understanding these fundamental concepts of epidemiology is crucial in healthcare, as they inform the development of prevention and control strategies for diseases. Epidemiology helps healthcare providers identify the risk factors associated with a disease, develop screening and prevention programs, and evaluate the effectiveness of interventions. By applying these concepts, healthcare providers can work towards improving the health of populations and reducing the burden of disease.