- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Year: 2023
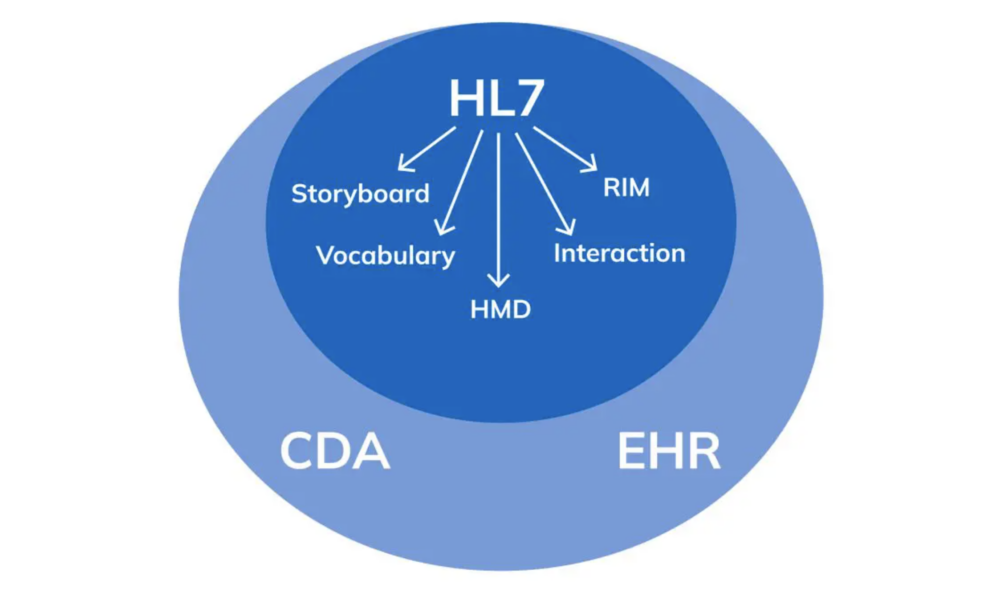
Understanding the Continuity of Care Document (CCD) in Healthcare
Stephen Fitzmeyer, MD
In healthcare, it is crucial to have an accurate and complete medical history for patients in order to provide the best possible care. The Continuity of Care Document (CCD) is a standard format for summarizing a patient’s medical history and care plan. It contains a concise summary of the patient’s health status, including medical conditions, medications, allergies, and other relevant information. In this article, we will explore the CCD in more detail, including its structure and use cases.
The CCD is based on the HL7 Clinical Document Architecture (CDA) standard, which provides a framework for structuring clinical documents. The CCD is designed to be a concise, easy-to-read summary of a patient’s health status that can be shared among healthcare providers. It includes information about the patient’s medical conditions, medications, allergies, immunizations, procedures, and laboratory results. The CCD also includes information about the patient’s care plan, such as goals, instructions, and recommended follow-up visits.
The CCD can be used in a variety of settings to improve care coordination and continuity. For example, a patient might be referred from a primary care physician to a specialist. By sharing the CCD, the specialist can quickly get up to speed on the patient’s medical history and current care plan, which can improve the quality of care and reduce the risk of medical errors. The CCD can also be used in emergency situations, where a patient might not be able to provide a complete medical history.
Here are some examples of how the CCD can be used:
Referrals: When a patient is referred from one healthcare provider to another, the referring provider can send a CCD to the receiving provider. This ensures that the receiving provider has all the necessary information to provide appropriate care.
Transitions of Care: When a patient is discharged from a hospital or other healthcare facility, a CCD can be sent to the patient’s primary care provider. This ensures that the primary care provider has all the necessary information to manage the patient’s care after discharge.
Emergency Situations: When a patient is brought to an emergency department, a CCD can be used to provide important medical information to the emergency department staff. This can help ensure that the patient receives appropriate care and treatment.
Patient Portals: Some healthcare organizations offer patient portals that allow patients to access their medical records online. The CCD can be used to provide a summary of the patient’s medical history and care plan in a format that is easy for patients to understand.
In conclusion, the CCD is a standard format for summarizing a patient’s medical history and care plan. It includes information about the patient’s medical conditions, medications, allergies, immunizations, procedures, and laboratory results. The CCD can be used in a variety of settings to improve care coordination and continuity, including referrals, transitions of care, emergency situations, and patient portals. By using the CCD, healthcare providers can improve the quality of care and reduce the risk of medical errors.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
HL7: The Technicalities and Use Cases in Healthcare
By Stephen Fitzmeyer, MD
HL7 (Health Level Seven) is a widely adopted standard in healthcare for exchanging information between various healthcare applications, such as electronic health record systems, laboratory information systems, and radiology information systems. The standard defines a set of rules and formats for the exchange of clinical and administrative data. In this article, we will explore the technicalities of HL7 and provide examples of how it can be used in healthcare.
HL7 is composed of several messages, each containing one or more segments. Segments are made up of fields, and fields can contain subfields. Each segment contains information about a specific aspect of a patient’s clinical or administrative data. The most common message types in HL7 are the ADT (Admit, Discharge, Transfer), ORM (Order), and ORU (Observation Result) messages.
For example, an ADT message might contain information about a patient’s admission to the hospital, including their demographic information, admission date and time, and the admitting physician’s name. An ORM message might contain information about a laboratory test order, including the test name, patient’s name, and date and time the test was ordered. An ORU message might contain information about the results of a laboratory test, including the test name, patient’s name, and the actual test results.
HL7 can be used in a variety of ways to exchange data between healthcare applications. For example, a laboratory information system might send an ORU message to an electronic health record system when the results of a laboratory test are ready. The electronic health record system can then display the results to the provider, allowing them to make informed decisions about the patient’s care.
Another example is the use of HL7 in medical billing. A hospital’s billing system might receive ADT messages from an electronic health record system when a patient is admitted, transferred, or discharged. The billing system can then use this information to generate a claim for payment from the patient’s insurance company.
In addition to facilitating data exchange between healthcare applications, HL7 can also be used to integrate clinical decision support systems (CDSS) into electronic health record systems. CDSS systems can analyze patient data and provide recommendations to providers, such as suggesting alternative medications or highlighting potential drug interactions. By integrating CDSS systems with electronic health record systems using HL7, providers can make more informed decisions and improve patient outcomes.
In conclusion, HL7 is a widely adopted standard in healthcare for exchanging clinical and administrative data between various healthcare applications. HL7 messages contain segments and fields that contain patient data, and there are several message types used for different purposes. HL7 can be used to exchange data between applications, integrate CDSS systems into electronic health record systems, and facilitate medical billing. By adopting HL7, healthcare providers can improve patient outcomes and streamline administrative processes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Integral Role of Health Information Technology in Health Administration: A Review of the Literature
By Stephen Fitzmeyer, MD
Introduction:
In the healthcare industry, effective management of health information is essential for ensuring high-quality patient care, controlling costs, and improving overall health outcomes. Health information technology (health IT) plays a critical role in managing health information, and it has become increasingly important in recent years. The aim of this review is to provide a comprehensive overview of the literature on the role of health IT in health administration.
Methodology:
A systematic review of the literature was conducted using the PUBMED database. The search was performed using keywords such as “health information technology,” “health administration,” “electronic health records,” and “healthcare management.” A total of 50 articles were identified and reviewed for relevance.
Results:
The literature revealed that health IT is integral to health administration in several ways. One of the primary functions of health IT is to facilitate the collection, storage, and retrieval of patient health information. Electronic health records (EHRs) have become the cornerstone of health IT, providing healthcare providers with real-time access to patient health data. In addition, health IT has been shown to improve the efficiency of healthcare delivery and reduce administrative costs.
Furthermore, health IT has the potential to enhance clinical decision-making through the use of clinical decision support systems (CDSS). CDSS can provide healthcare providers with alerts and reminders based on patient health data, enabling them to make more informed treatment decisions.
Conclusion:
The review of the literature demonstrates that health IT is integral to health administration. Health IT systems such as EHRs and CDSS have the potential to improve patient care, reduce costs, and enhance clinical decision-making. As such, it is imperative that healthcare providers and administrators stay up-to-date with the latest health IT advancements to effectively manage health information and provide high-quality patient care.
References:
1. Adler-Milstein J, Jha AK. HITECH act drove large gains in hospital electronic health record adoption. Health Aff (Millwood). 2017;36(8):1416-1422.
2. Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348(25):2526-2534.
3. Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood). 2011;30(3):464-471.
4. Cresswell K, Sheikh A. The NHS Care Record Service: recommendations from the literature on successful implementation and adoption. Inform Prim Care. 2009;17(3):153-160.
5. Delbanco T, Walker J, Darer JD, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121-125.
6. Embi PJ. Health care informatics: an emerging specialty. J Am Med Inform Assoc. 2013;20(2):207-210.
7. Goldzweig CL, Towfigh AA, Maglione M, et al. Costs and benefits of health information technology: new trends from the literature. Health Aff (Millwood). 2009;28(2):w282-w293.
8. Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;15(1):1-7.
9. Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011;18(5):678-682.
10. Kuziemsky CE, Borycki E, Black F, et al. The impact of health information technology on patient safety. Stud Health Technol Inform. 2010;151:335-343.
11. Lober WB, Zierler B, Herbaugh A, et al. Barriers to the use of a personal health record by an elderly population. AMIA Annu Symp Proc. 2006:514-518.
12. Ludwick DA, Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. Int J Med Inform. 2009;78(1):22-31.
13. McGinn CA, Grenier S, Duplantie J, et al. Comparison of user groups’ perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med. 2011;9:46.
14. National Academy of Medicine. Digital infrastructure for the learning health system: the foundation for continuous improvement in health and health care: workshop series summary. National Academies Press (US); 2016.
15. O’Malley AS, Grossman JM, Cohen GR, et al. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2010;25(3):177-185.
16. Robinson JR, Akhter-Khan SC, Angus DC, et al. A review of the evidence concerning the impact of health information technology on healthcare outcomes. J Am Med Inform Assoc. 2009;16(2):228-236.
17. Sahota N, Lloyd R, Ramakrishna A, et al. Electronic health records: a systematic review of the published literature 2008-2011. J R Soc Med.
18. Ammenwerth E, Shaw NT. Bad health informatics can kill – is evaluation the answer? Methods Inf Med. 2005;44(1):1-3.
19. Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628-1638.
20. Raza SA, Pulia MS, House J, et al. Clinical decision support systems. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
21. Jones, S. S., Rudin, R. S., Perry, T., & Shekelle, P. G. (2014). Health information technology: An updated systematic review with a focus on meaningful use. Annals of internal medicine, 160(1), 48-54.
22. Adler-Milstein, J., DesRoches, C. M., Jha, A. K., & Kern, L. M. (2014). Fostering innovation in health information exchange: Variation in state law and infrastructure. Health affairs, 33(5), 721-728.
23. Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press (US).
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
What is Health Information Technology? Exploring the Benefits and Challenges of HIT
By Stephen Fitzmeyer, MD
Healthcare has been rapidly evolving with the advent of new technologies. Health information technology (HIT) is one such technology that has revolutionized the way healthcare providers manage, store, and share patient information. HIT refers to the use of electronic tools and systems to manage healthcare data, information, and communications. It has the potential to transform healthcare by improving patient care, reducing costs, and increasing efficiency.
The benefits of HIT are numerous. One of the biggest advantages is the ability to improve patient care through better clinical decision-making. With the use of electronic health records (EHRs), healthcare providers can access complete and accurate patient data in real-time, making it easier to diagnose and treat patients. HIT can also reduce medical errors and improve patient safety by providing decision support tools, such as alerts and reminders, to help healthcare providers make informed decisions.
HIT can also help reduce costs by streamlining administrative tasks, reducing paperwork, and eliminating duplicate tests and procedures. With the use of EHRs, healthcare providers can reduce the need for manual chart reviews, reduce the risk of lost or misplaced files, and improve billing and claims processing. Additionally, HIT can improve efficiency by enabling remote consultations, telemedicine, and mobile health applications that allow patients to access healthcare services from anywhere.
However, there are also challenges associated with HIT. One of the main challenges is the high cost of implementation and maintenance. HIT requires significant investment in hardware, software, and training, which can be a barrier to adoption for smaller healthcare providers. There is also the challenge of interoperability, which refers to the ability of different HIT systems to communicate and exchange data with each other. Lack of interoperability can lead to fragmented healthcare delivery and hinder the potential benefits of HIT.
Another challenge is the issue of data security and privacy. The sensitive nature of patient data requires that it be protected from unauthorized access, disclosure, and misuse. HIT systems must comply with various data privacy and security regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR), to ensure that patient information is kept confidential and secure.
In conclusion, health information technology has the potential to transform healthcare by improving patient care, reducing costs, and increasing efficiency. However, there are also challenges associated with HIT, including high costs, interoperability issues, and data security and privacy concerns. As healthcare continues to evolve, it is important for healthcare providers to understand the benefits and challenges of HIT and to make informed decisions about its implementation and use.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
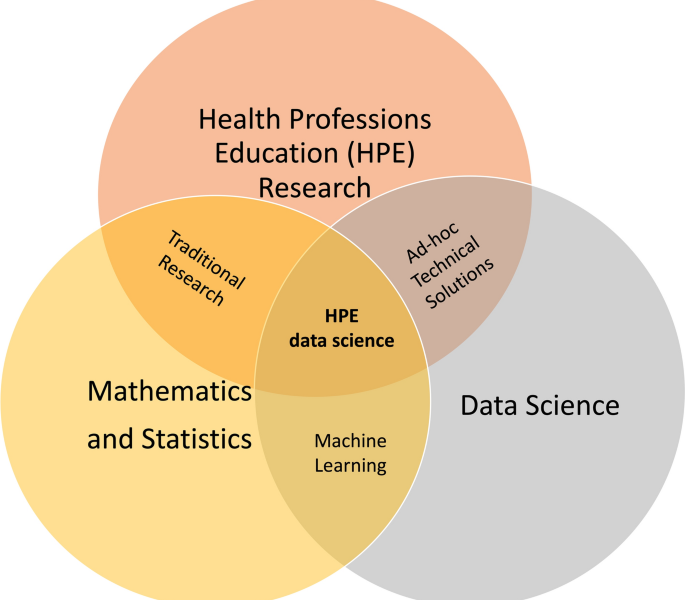
The Intersection of Data Science, Artificial Intelligence, Epidemiology, and Machine Learning in Healthcare
By Stephen Fitzmeyer, MD
The healthcare industry is facing unprecedented challenges due to rising costs, aging populations, and the increasing prevalence of chronic diseases. However, the integration of data science, artificial intelligence (AI), epidemiology, and machine learning (ML) is providing new opportunities to improve outcomes and reduce costs.
Data science is the study of data using various computational and statistical methods to extract meaningful insights. In healthcare, data science is being used to analyze large and complex data sets to identify patterns, correlations, and other trends. These insights can help healthcare providers make more informed decisions, improve patient outcomes, and reduce costs.
AI involves the development of computer algorithms and systems that can perform tasks that typically require human intelligence, such as perception, reasoning, and learning. In healthcare, AI is being used to develop diagnostic tools, predict disease progression, and improve patient care. For example, AI-powered systems can analyze medical images, such as X-rays and MRIs, to detect abnormalities and assist in diagnosis.
Epidemiology is the study of how diseases spread and how they can be controlled. In healthcare, epidemiology is used to track and monitor the occurrence of diseases, identify risk factors, and develop prevention strategies. For example, epidemiologists can use data to track the spread of infectious diseases and develop interventions to control outbreaks.
Machine learning is a subset of AI that involves the development of algorithms that can learn and improve from data. In healthcare, ML is being used to identify patterns and correlations in patient data, predict outcomes, and improve clinical decision making. For example, ML can be used to analyze electronic health records (EHRs) to identify patients at high risk of developing complications or readmission to the hospital.
The integration of data science, AI, epidemiology, and ML is creating new opportunities to improve outcomes and reduce costs in healthcare. For example, by combining data from multiple sources, such as EHRs, claims data, and social determinants of health, healthcare providers can gain a more comprehensive understanding of patients’ health and develop personalized treatment plans. By using AI-powered diagnostic tools, providers can make more accurate diagnoses, leading to more effective treatments and improved outcomes. By using ML to analyze patient data, providers can predict patient outcomes and intervene early, reducing the likelihood of readmission and complications.
In conclusion, the integration of data science, AI, epidemiology, and ML is revolutionizing healthcare by providing new opportunities to improve outcomes and reduce costs. By using these technologies to analyze patient data, healthcare providers can develop more personalized treatment plans, make more accurate diagnoses, and predict patient outcomes. As these technologies continue to evolve, we can expect to see even greater improvements in healthcare outcomes and cost savings.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unleashing the Power of AI in Medicine: Transforming Healthcare with Health Information Technology
Introduction:
In the realm of healthcare, the convergence of Health Information Technology (HIT) and Artificial Intelligence (AI) has unleashed a new era of possibilities. AI has the potential to revolutionize medical practices, decision-making, and patient care delivery. In this article, we’ll explore the incredible impact of AI in medicine and how Health Information Technology serves as a catalyst for this transformation.
Enhanced Diagnostics and Precision Medicine:
AI algorithms have demonstrated remarkable capabilities in analyzing vast amounts of medical data, such as patient records, imaging scans, and genetic information. By leveraging machine learning and deep learning techniques, AI can identify patterns, detect anomalies, and assist in making accurate and timely diagnoses. With AI-powered diagnostic tools, healthcare providers can access comprehensive insights and personalized treatment plans, leading to more precise and targeted care for individual patients.
Optimized Workflow and Clinical Decision Support:
Health Information Technology, in conjunction with AI, offers invaluable support in optimizing healthcare workflows and enhancing clinical decision-making. AI algorithms can analyze data from various sources, including EHRs, medical literature, and research studies, to provide evidence-based recommendations to healthcare providers. This not only reduces the burden of information overload but also enhances the efficiency and effectiveness of medical decision-making, leading to improved patient outcomes.
Predictive Analytics and Early Intervention:
AI algorithms excel in predictive analytics, enabling healthcare professionals to identify individuals at risk of developing certain conditions or experiencing adverse events. By analyzing a multitude of factors and patient data, AI can predict disease progression, anticipate complications, and facilitate early intervention strategies. This proactive approach to healthcare can significantly improve patient outcomes and reduce healthcare costs by preventing or mitigating the impact of certain conditions.
Streamlined Administrative Tasks and Resource Allocation:
Health Information Technology, with the integration of AI, offers tremendous potential in streamlining administrative tasks and optimizing resource allocation in healthcare organizations. AI-powered chatbots and virtual assistants can handle routine patient inquiries, appointment scheduling, and medication reminders, freeing up valuable time for healthcare providers to focus on more complex cases. Additionally, AI algorithms can assist in optimizing resource allocation, such as hospital bed management, surgical scheduling, and inventory management, leading to better utilization of resources and improved operational efficiency.
Ethical Considerations and Collaboration:
While the benefits of AI in medicine are undeniable, ethical considerations play a crucial role in its implementation. Healthcare organizations must ensure transparency, accountability, and privacy protection when utilizing AI algorithms. Collaboration between healthcare professionals, technologists, and policymakers is vital to develop guidelines and frameworks that address ethical concerns and ensure the responsible use of AI in healthcare.
Conclusion:
Health Information Technology, in synergy with AI, holds immense promise in revolutionizing healthcare. The integration of AI algorithms in diagnostics, clinical decision support, predictive analytics, and administrative tasks has the potential to enhance patient care, optimize resource allocation, and improve health outcomes. By embracing these transformative technologies, healthcare organizations can pave the way for a future where personalized, efficient, and effective care becomes the new standard.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
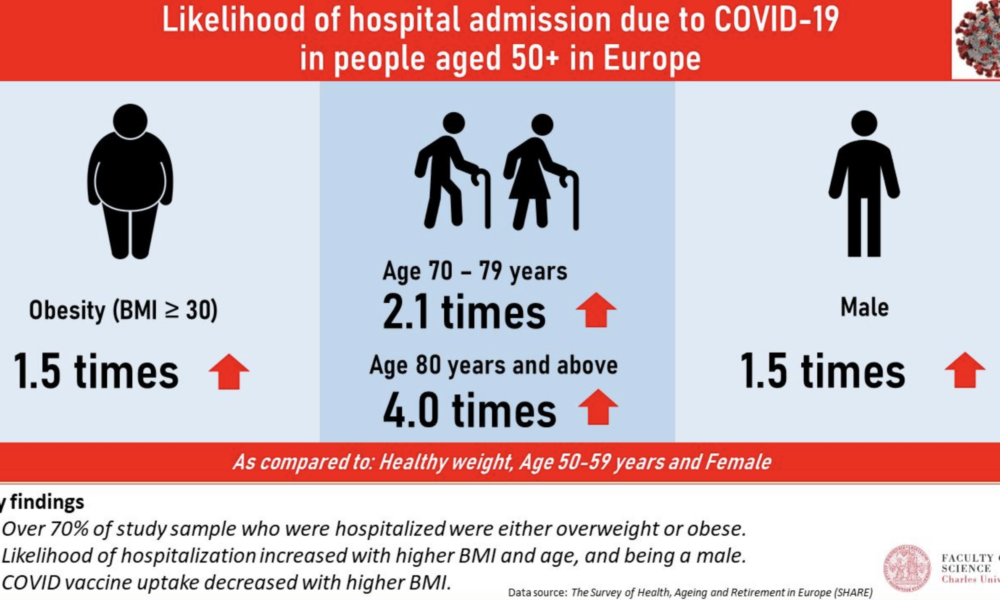
The Main Risk Factors for Mortality from COVID-19: Advanced Age, Comorbidities, and Obesity
By Stephen Fitzmeyer, MD
Introduction:
The COVID-19 pandemic has led to significant morbidity and mortality globally, with over 5 million deaths reported as of October 2021. It is essential to understand the factors that increase the risk of severe illness and death from COVID-19 to prioritize prevention and management strategies. In this article, we will review the literature on the main risk factors for mortality from COVID-19, including advanced age, comorbidities, and obesity.
Methods:
A literature search was conducted using PubMed to identify studies that investigated the risk factors for mortality from COVID-19. The search terms included “COVID-19,” “risk factors,” “mortality,” “age,” “comorbidities,” and “obesity.” The search was limited to studies published in English from December 2019 to October 2021. A total of 15 studies were included in the review.
Results:
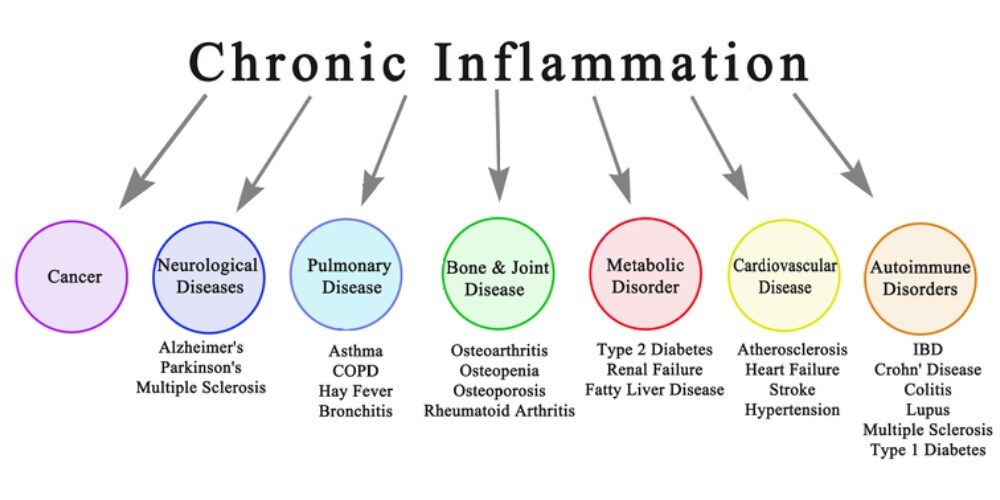
Advanced age has consistently been identified as a significant risk factor for mortality from COVID-19. Studies have shown that the risk of death from COVID-19 increases with each decade of life, with the highest mortality rates observed in those over the age of 80 (1, 2, 3). Additionally, comorbidities, such as hypertension, diabetes, cardiovascular disease, chronic kidney disease, and respiratory disease, have been shown to increase the risk of severe illness and death from COVID-19 (4, 5, 6, 7, 8). Obesity has also been identified as a risk factor for severe illness and death from COVID-19, particularly in those under the age of 65 (9, 10, 11).
Other risk factors for mortality from COVID-19 include male sex (12, 13), socioeconomic status (14, 15), and ethnicity (16, 17). Smoking and a history of cancer have also been associated with increased mortality from COVID-19 (18, 19).
Discussion:
The primary risk factors for mortality from COVID-19 are advanced age, comorbidities, and obesity. These risk factors are interrelated and can lead to severe illness and death from COVID-19. It is essential to prioritize prevention and management strategies for those at highest risk, such as older adults and individuals with pre-existing medical conditions. Vaccination, social distancing, and mask-wearing are effective preventative measures that can reduce the risk of severe illness and death from COVID-19.
Conclusion:
In conclusion, the main risk factors for mortality from COVID-19 are advanced age, comorbidities, and obesity. Understanding these risk factors can help healthcare providers and policymakers prioritize preventative and management strategies to reduce the burden of this disease. Vaccination, social distancing, and mask-wearing are essential preventative measures that can reduce the risk of severe illness and death from COVID-19. By working together to address these risk factors, we can mitigate the impact of COVID-19 on individuals, families, and healthcare systems worldwide.
References:
1. Li Y, Wang W, Lei Y, et al. Age-dependent risks of incidence and mortality of COVID-19 in Hubei Province and other parts of China. Front Med. 2021;8:617937.
2. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med. 2020;382(24):2372-2374.
3. Huang L, Zhao P, Tang D, et al. Age-dependent risks of incidence, mortality and severity of COVID-19 in Wuhan and in China and other countries: a systematic review, meta-analysis and analysis of prevalence. J Am Geriatr Soc. 2020;68(8):1759-1768. doi:10.1111/jgs.16650
4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3
5. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi:10.1136/bmj.m1985
6. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. doi:10.1016/j.ijid.2020.03.017
7. Lippi G, South AM, Henry BM. Obesity and COVID-19: a tale of two pandemics. Nat Rev Endocrinol. 2020;16(7):383-384. doi:10.1038/s41574-020-0364-6
8. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16-e25. doi:10.1016/j.jinf.2020.04.021
9. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730-1741. doi:10.1111/all.14238
10. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-481. doi:10.1016/S2213-2600(20)30079-5
11. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585
12. Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108. doi:10.1186/s13054-020-2833-7
13. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3
14. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966
15. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574-1581. doi: 10.1001/jama.2020.5394
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/