- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Health Informatics
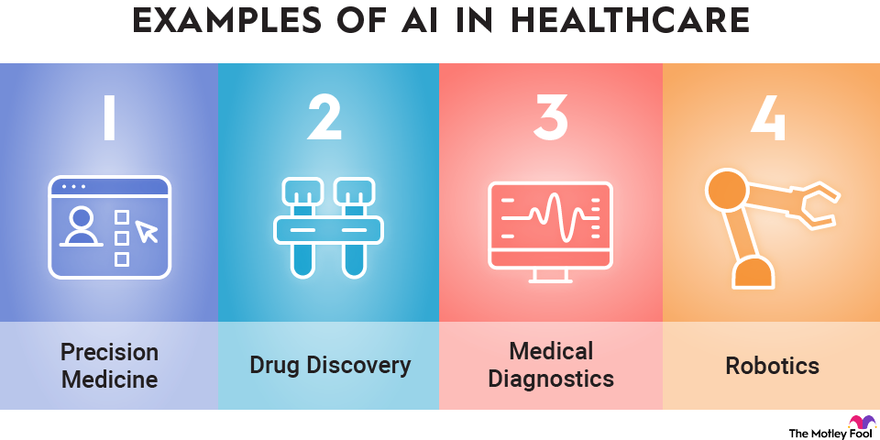
The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
Healthcare is at a pivotal moment in history, where technological innovation is redefining how care is delivered, managed, and optimized. At the core of this revolution are Artificial Intelligence (AI), Clinical Informatics, and Machine Learning (ML), fields that intersect to create a paradigm shift in the way we approach health and wellness. This confluence has the potential to enhance decision-making, streamline operations, and improve patient outcomes.
1. Transforming Healthcare Through
AI brings an unprecedented ability to process and analyze large datasets with speed and accuracy that no human could match. In healthcare, AI is being applied to areas such as:
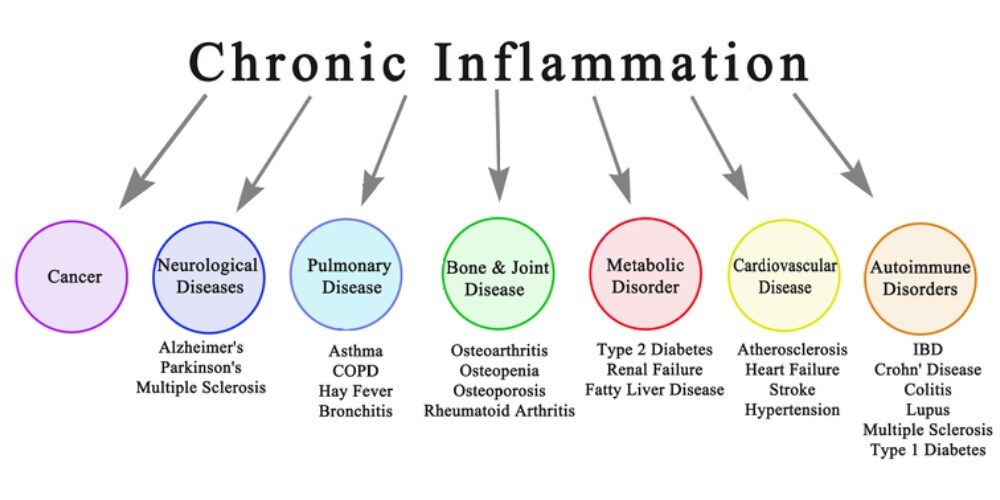
- Predictive Analytics: AI algorithms can predict patient outcomes based on historical data, enabling proactive intervention. For example, models trained on electronic health record (EHR) data can forecast hospital readmissions or identify patients at risk for chronic diseases.
- Medical Imaging: AI-powered tools can analyze X-rays, MRIs, and CT scans, often detecting anomalies with greater precision than human radiologists.
- Personalized Medicine: AI tailors treatment plans by analyzing genetic, lifestyle, and environmental factors. This ensures therapies are as effective as possible for individual patients.
2. The Role of Clinical Informatics
Clinical Informatics is the backbone of data-driven decision-making in healthcare. It focuses on the optimal use of information and technology to improve patient care and health outcomes. Informatics integrates with AI and ML in several ways:
- Data Integration: Informatics ensures the seamless aggregation and harmonization of diverse healthcare data sources, from EHRs to wearable devices.
- Interoperability: The field promotes standards and protocols that allow AI systems to access and utilize data across different platforms and institutions.
- Clinical Decision Support Systems (CDSS): Informatics integrates AI-driven insights into clinician workflows, enabling smarter, faster, and more accurate decisions at the point of care.
3. Machine Learning as the Engine of Innovation
Machine Learning, a subset of AI, excels at identifying patterns in data and making predictions. In healthcare, ML applications are advancing at a rapid pace:
- Drug Discovery: ML accelerates drug development by predicting how compounds interact with biological systems, reducing the time and cost of bringing new medications to market.
- Operational Efficiency: Hospitals are using ML to optimize staffing, predict supply needs, and improve resource allocation, reducing waste and enhancing patient experiences.
- Natural Language Processing (NLP): ML-powered NLP systems analyze unstructured clinical notes, turning them into actionable insights. This has implications for billing, compliance, and clinical documentation.
4. Ethical and Practical Considerations
While the potential of AI, ML, and Clinical Informatics in healthcare is vast, it is not without challenges:
- Data Privacy and Security: With vast amounts of sensitive health data being processed, ensuring robust cybersecurity measures is critical.
- Bias in Algorithms: AI systems trained on biased datasets can perpetuate disparities in care. Diverse data representation is essential to mitigate this risk.
- Clinician Adoption: Integrating AI tools into clinical practice requires buy-in from healthcare professionals. These tools must be user-friendly and provide clear, actionable insights.
5. The Future of Healthcare
The intersection of AI, Clinical Informatics, and ML is laying the groundwork for a healthcare system that is:
- More Predictive: By identifying health issues before they become critical, we can move from reactive to preventive care.
- More Personalized: Treatments will be increasingly tailored to the unique characteristics of each patient.
- More Efficient: Automation of administrative tasks will allow clinicians to focus more on patient care.
Conclusion
The synergy between AI, Clinical Informatics, and Machine Learning is transforming healthcare into a smarter, more adaptive system. These technologies are not merely tools but catalysts for innovation, enabling a future where healthcare is not only more efficient but also more human.
As we navigate this new frontier, the focus must remain on ensuring ethical implementation, fostering trust among stakeholders, and keeping the patient at the center of every innovation.
How AI Can Transform Healthcare Applications
How AI Can Transform Healthcare Applications
As a developer of healthcare applications, you’re constantly looking for ways to improve functionality, efficiency, and user experience. Artificial Intelligence (AI) offers a transformative opportunity to enhance healthcare apps, making them smarter, more user-friendly, and impactful. Here’s how AI can elevate your healthcare applications to the next level.
1. Enhancing Patient Care and Management
- Personalized Treatment Recommendations: AI algorithms analyze patient data like lab results, genetic information, and medical history to suggest tailored treatment plans.
- Virtual Assistants: Chatbots powered by natural language processing (NLP) can answer common patient questions, help schedule appointments, and remind patients about medications.
- Predictive Analytics: AI models predict potential health issues, such as diabetes or cardiovascular disease, allowing for early intervention and better patient outcomes.
2. Supporting Clinical Decision-Making
- AI Diagnosis Tools: Machine learning can analyze medical images, lab tests, or patient-reported symptoms to help identify conditions quickly and accurately.
- Drug Interaction Alerts: AI systems can flag potential drug interactions or contraindications based on a patient’s medication history.
- Risk Assessment Models: Predictive models assess patient risks for conditions like stroke or sepsis, enabling proactive care.
3. Optimizing Workflow
- Automated Documentation: NLP tools transcribe and summarize doctor-patient conversations, reducing administrative burdens.
- Intelligent Scheduling: AI-powered tools optimize staff and appointment scheduling, minimizing wait times and maximizing resource utilization.
- Claims Automation: Automate insurance claim reviews with AI, reducing errors and speeding up reimbursement processes.
4. Enhancing Telemedicine and Remote Monitoring
- AI Diagnostics: Enhance telehealth platforms with tools that analyze patient-reported data or uploaded images during virtual consultations.
- Wearable Data Integration: Develop AI algorithms to process data from wearables, offering actionable insights into patient health.
- Symptom Checkers: AI-driven tools allow patients to input symptoms and receive preliminary assessments, streamlining triage.
5. Delivering Data Insights and Analytics
- Patient Cohort Analysis: AI identifies patterns in patient populations, improving treatment strategies and research.
- Health Trend Forecasting: Analyze big data to predict public health trends or disease outbreaks.
- Operational Efficiency: Use AI to optimize inventory, staffing, and resource allocation in clinical settings.
6. Improving Patient Engagement
- Conversational Interfaces: Enable patients to interact with your app through natural language queries, making healthcare more accessible.
- Gamification: Use AI to personalize gamified elements, encouraging adherence to treatment plans or healthy behaviors.
- Educational Content: Deliver tailored educational materials based on a patient’s condition or interests.
7. Ensuring Compliance and Security
- Data Anonymization: AI can de-identify sensitive patient data for compliance with regulations like HIPAA and GDPR.
- Fraud Detection: AI detects anomalies in billing or prescriptions that may indicate fraud.
- Secure Data Sharing: Facilitate secure and efficient sharing of patient records among healthcare providers.
8. Facilitating Research and Development
- Clinical Trial Matching: Match eligible patients to clinical trials using AI-driven analysis of their medical profiles.
- Drug Discovery: Use AI models to simulate and analyze potential drug compounds.
- Real-World Evidence: Generate insights from patient data to support post-market surveillance and drug efficacy studies.
9. Expanding Accessibility
- Language Translation: Offer multilingual support for diverse patient populations with AI translation tools.
- Accessibility Features: Build AI-driven speech-to-text and text-to-speech features for patients with disabilities.
10. Elevating User Experience
- Predictive Navigation: Anticipate user actions to streamline navigation and improve usability.
- Behavioral Nudges: Deliver proactive reminders or nudges, such as medication adherence prompts, based on user behavior.
- Dynamic Interfaces: Personalize app interfaces based on user preferences and engagement patterns.
Example: Implementing an AI-Powered Symptom Checker
Here’s an example of how you might structure an app to include a symptom checker using AI:
- Input Collection: The app asks users to input symptoms via text or voice.
- Natural Language Processing (NLP): AI processes the input to extract relevant medical terms and symptoms.
- Symptom Analysis: The app uses a machine learning model trained on a medical dataset to compare the user’s symptoms with known patterns of illnesses.
- Recommendation Engine: Based on the analysis, the app provides possible conditions and suggests whether the user should seek immediate care, consult a doctor, or try home remedies.
- Continuous Learning: The app collects anonymized feedback from user interactions to improve the accuracy of the model over time.
Example Code for NLP Symptom Processing:
from transformers import pipeline
# Load a pre-trained NLP model for healthcare applications
nlp_model = pipeline("text-classification", model="bert-base-healthcare")
# Example user input
user_input = "I have a persistent cough and shortness of breath."
# Process the input
analysis = nlp_model(user_input)
# Output AI-generated insights
print("Potential conditions:", analysis)
This code snippet demonstrates how to use a pre-trained NLP (Natural Language Processing) model from the Hugging Face transformers library to classify text related to healthcare applications. Here’s a breakdown of what each part of the code does:
1. Importing pipeline from the transformers library
from transformers import pipelineThe pipeline function provides an easy interface to use pre-trained models for various NLP tasks like text classification, question answering, translation, etc.
2. Loading a Pre-trained NLP Model
nlp_model = pipeline("text-classification", model="bert-base-healthcare")pipeline("text-classification"): This specifies that the task is text classification, where input text will be categorized into predefined classes or labels.model="bert-base-healthcare": Refers to a pre-trained BERT (Bidirectional Encoder Representations from Transformers) model fine-tuned for healthcare-related text classification. This specific model would likely be trained to understand healthcare vocabulary and contexts.
3. Processing User Input
user_input = "I have a persistent cough and shortness of breath."
analysis = nlp_model(user_input)The pipeline processes the input text using the loaded model to predict potential conditions or categories related to the input.
4. Outputting Results
print("Potential conditions:", analysis)The analysis variable contains the model’s predictions, such as potential health conditions or relevant categories for the provided symptoms.
Example Output
Potential conditions: [{'label': 'Respiratory Issue', 'score': 0.95}]- label: The predicted category (e.g., “Respiratory Issue”).
- score: The confidence score for this prediction (e.g., 0.95, indicating 95% confidence).
Use Case
This code can be part of a healthcare chatbot, clinical decision support system, or any application designed to provide preliminary insights based on patient symptoms. However, these AI-generated insights should not replace professional medical advice.
Getting Started with AI Integration
To start incorporating AI into your healthcare applications:
- Start Small: Begin with a single AI feature, such as a chatbot or predictive analytics, to test feasibility and user acceptance.
- Prioritize Data Quality: Ensure clean, accurate data to power your AI models effectively.
- Focus on Ethics: Build trust by maintaining transparency, privacy, and fairness in AI algorithms.
- Iterate and Scale: Use feedback to refine AI functionalities and expand capabilities over time.
AI is reshaping healthcare, offering exciting opportunities to create more impactful applications. By leveraging AI, you can provide better care, improve efficiency, and drive innovation in healthcare technology.
From Cholera to COVID-19: The Role of Epidemiology in Disease Outbreaks
By Stephen Fitzmeyer, MD
The cholera outbreak in 1854 in London, and the work of John Snow, is considered a turning point in the field of epidemiology. The outbreak caused thousands of deaths and was traced back to contaminated water from the Broad Street pump. Snow’s investigation led him to identify the source of the outbreak, and he subsequently recommended measures to prevent the spread of cholera.
Fast forward to modern times, and we are facing a new epidemic – COVID-19. The similarities between the two outbreaks are striking, and so are the differences. Like cholera, COVID-19 is a highly contagious disease that spreads through contact with infected individuals or surfaces. However, unlike cholera, COVID-19 is caused by a novel virus that is still not fully understood.
Epidemiology played a crucial role in both outbreaks. In the case of cholera, Snow used epidemiological methods to map the spread of the disease and identify the source of the outbreak. He collected data on the location of cases and the source of water for the affected individuals, and used this data to create a map that showed a clear association between the cases and the Broad Street pump. This data-driven approach was a key factor in his successful intervention.
Similarly, epidemiology has played a critical role in the management of COVID-19. Epidemiologists have been tracking the spread of the disease, identifying risk factors and patterns of transmission, and providing guidance on how to mitigate the spread of the virus. Epidemiological models have been used to predict the course of the pandemic, and to inform public health policies and interventions.
However, there are also significant differences between the two outbreaks. COVID-19 is a much more complex disease than cholera, with a wide range of symptoms and outcomes. The virus is highly contagious and can be spread by asymptomatic carriers, making it much more challenging to control. The development of effective vaccines and treatments has been a major focus of the public health response to COVID-19, and epidemiology has played a critical role in evaluating the effectiveness of these interventions.
In conclusion, the cholera outbreak and the work of John Snow laid the foundation for modern epidemiology, and the lessons learned from that outbreak have helped us manage and control many subsequent disease outbreaks. The COVID-19 pandemic has presented a new set of challenges, but the principles of epidemiology remain essential to understanding and controlling the spread of the virus. By continuing to apply these principles, we can hope to mitigate the impact of the pandemic and prepare for future outbreaks.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Healing Power of Algorithms: Unleashing the Potential of Artificial Intelligence in Medicine
Introduction
Artificial Intelligence (AI) has emerged as a game-changer in the field of medicine, offering new horizons for diagnosis, treatment, and healthcare management. With the ability to process vast datasets and perform complex tasks at speeds unimaginable for humans, AI is poised to revolutionize the healthcare industry. In this article, we explore the tremendous potential of artificial intelligence in medicine and its transformative impact on patient care.
Disease Diagnosis and Early Detection
AI algorithms are becoming proficient at identifying patterns and anomalies in medical images, such as X-rays, MRIs, and CT scans. This capacity can lead to earlier and more accurate diagnoses, ultimately improving patient outcomes. For instance, AI can detect early signs of diseases like cancer, heart conditions, and neurological disorders, allowing for timely intervention.
Personalized Treatment Plans
AI analyzes patient data, including genetic information, medical history, and lifestyle factors, to create personalized treatment plans. By tailoring therapies to individual patients, healthcare providers can optimize the effectiveness of treatment and minimize adverse effects.
Drug Discovery and Development
AI accelerates drug discovery by simulating complex molecular interactions and predicting potential drug candidates. This reduces the time and cost involved in bringing new drugs to market, offering hope for more effective treatments for various diseases.
Clinical Decision Support
AI provides healthcare professionals with real-time decision support by analyzing patient data, suggesting treatment options, and predicting outcomes. It can assist in making informed decisions, reducing medical errors, and ensuring the best possible care.
Healthcare Automation
AI-powered chatbots and virtual assistants are becoming increasingly common in healthcare. They can answer patient queries, schedule appointments, and provide information on medications and post-treatment care, thus freeing up healthcare professionals’ time.
Predictive Analytics and Population Health Management
AI can analyze patient data to identify at-risk populations, predict disease outbreaks, and improve preventive care. This is particularly valuable for public health initiatives and the management of chronic conditions.
Telemedicine and Remote Monitoring
AI enhances telemedicine by enabling remote monitoring of patients’ vital signs, medication adherence, and general well-being. This approach is especially beneficial for patients with chronic conditions who require continuous care.
Radiology and Pathology Assistance
AI can assist radiologists and pathologists in interpreting medical images by highlighting areas of concern, reducing the chance of oversight, and expediting diagnosis.
Natural Language Processing (NLP) for Medical Records
NLP technologies extract valuable information from unstructured medical records. This aids in clinical research, quality improvement, and more accurate coding for billing and insurance purposes.
Patient Engagement and Wellness
AI-driven health apps and wearables help patients manage their health by tracking vital signs, providing health tips, and sending medication reminders. They also encourage a proactive approach to wellness.
Conclusion
Artificial intelligence has the potential to reshape the landscape of medicine in profound ways. Its ability to analyze data, make predictions, and assist healthcare providers empowers medical professionals to deliver more accurate diagnoses and effective treatments, while also enhancing the patient experience. As AI continues to evolve and integrate into healthcare systems, it holds the promise of improving patient outcomes, reducing healthcare costs, and addressing some of the most pressing challenges in the medical field. The future of medicine is increasingly intelligent, and it is poised to benefit both healthcare providers and patients alike.
Unlocking the Power of Health Informatics: Why It Matters
Introduction
Health informatics is a rapidly growing field that combines healthcare, information technology, and data science to transform the way we manage and utilize health-related information. In the digital age, health informatics plays a pivotal role in enhancing patient care, improving healthcare processes, and driving medical research. In this article, we delve into the importance of health informatics and the manifold ways in which it positively impacts the healthcare industry.
Enhanced Patient Care
Health informatics improves patient care by providing healthcare professionals with instant access to accurate and up-to-date patient information. Electronic Health Records (EHRs) store patient histories, test results, medications, and treatment plans, reducing the risk of medical errors and ensuring that the right treatment is delivered to the right patient.
Efficient Healthcare Processes
Health informatics streamlines administrative and clinical processes in healthcare. It reduces paperwork, automates scheduling and billing, and facilitates communication among healthcare providers. This efficiency not only saves time but also reduces costs, making healthcare more accessible.
Data-Driven Decision-Making
Health informatics leverages data analysis to inform healthcare decisions. By analyzing trends and patterns, healthcare providers can make more informed choices about patient care and resource allocation, ultimately improving patient outcomes.
Telemedicine and Remote Monitoring
The integration of health informatics in telemedicine enables remote consultations and monitoring of patients. This is particularly crucial in reaching patients in underserved or remote areas, providing access to quality healthcare that might otherwise be unattainable.
Public Health Surveillance
Health informatics supports public health initiatives by monitoring the spread of diseases and identifying potential outbreaks. Surveillance systems can help health agencies respond swiftly to emerging health threats.
Medical Research and Innovation
Health informatics aids medical research by facilitating access to vast pools of patient data. Researchers can analyze this data to discover new treatments, study disease trends, and develop innovative medical technologies.
Patient Engagement and Empowerment
Health informatics encourages patients to take an active role in their health. Patient portals allow individuals to access their own health records, communicate with healthcare providers, and make informed decisions about their care.
Interoperability and Data Sharing
Standardized data formats and interoperability among healthcare systems enable seamless sharing of patient information across different healthcare providers. This ensures continuity of care and prevents duplication of tests and procedures.
Healthcare Quality Improvement
Health informatics enables healthcare providers to assess and enhance the quality of care they deliver. By tracking outcomes, patient satisfaction, and compliance with best practices, providers can make data-driven improvements.
Cost Reduction and Resource Management
Health informatics helps healthcare institutions optimize resource allocation and reduce costs. By identifying inefficiencies and areas of improvement, healthcare organizations can direct their resources more effectively.
Conclusion
In an era where data is often referred to as the “new oil,” health informatics is the vehicle through which the healthcare industry taps into the vast potential of health-related information. It empowers healthcare professionals with tools and insights to provide more efficient, cost-effective, and patient-centric care. With the ability to save lives, reduce healthcare costs, and drive medical innovations, health informatics is more than a trend; it is the future of healthcare. Its importance continues to grow as technology evolves and as the healthcare industry strives to provide the best possible care to patients around the world.
Using Python to Parse HL7 and CCD Documents in Healthcare
By Stephen Fitzmeyer, MD
Python is a powerful programming language that can be used to parse and manipulate healthcare data in the HL7 and CCD formats. In this article, we will explore how to use Python to extract and process data from HL7 and CCD documents.
First, let’s start by understanding the structure of HL7 and CCD documents. HL7 messages are comprised of segments, which contain fields and subfields that represent different types of data. CCD documents, on the other hand, are based on the HL7 Clinical Document Architecture (CDA) standard and use XML to represent the data.
To parse HL7 messages in Python, we can use the hl7apy library, which is an open-source Python library for working with HL7 messages. Here’s an example of how to use hl7apy to extract patient demographic information from an HL7 message:
from hl7apy.parser import parse_message
# Parse the HL7 message
msg = parse_message(‘MSH|^~\&|HIS|BLG|LIS|BLG|20200528163415||ADT^A04|MSG0001|P|2.3||||||UNICODE’)
# Get the patient name
patient_name = msg.pid[5][0].value
# Get the patient date of birth
dob = msg.pid[7].value
# Get the patient sex
sex = msg.pid[8].value
# Print the patient information
print(“Patient Name: ” + patient_name)
print(“Date of Birth: ” + dob)
print(“Sex: ” + sex)
##########
In this example, we’re using the parse_message() method from the hl7apy library to parse the HL7 message. We then use the message object to extract the patient name, date of birth, and sex from the PID segment.
To parse CCD documents in Python, we can use the ElementTree library, which is included in the Python standard library. Here’s an example of how to use ElementTree to extract medication information from a CCD document:
import xml.etree.ElementTree as ET
# Parse the CCD document
tree = ET.parse(‘ccd.xml’)
# Get the medication section
medications = tree.findall(‘.//{urn:hl7-org:v3}section[@code=”10160-0″]/{urn:hl7-org:v3}entry/{urn:hl7-org:v3}substanceAdministration’)
# Print the medication information
for med in medications:
drug_name = med.find(‘{urn:hl7-org:v3}consumable/{urn:hl7-org:v3}manufacturedProduct/{urn:hl7-org:v3}manufacturedMaterial/{urn:hl7-org:v3}name/{urn:hl7-org:v3}part’).text
dosage = med.find(‘{urn:hl7-org:v3}doseQuantity/{urn:hl7-org:v3}value’).text
start_date = med.find(‘{urn:hl7-org:v3}effectiveTime/{urn:hl7-org:v3}low’).attrib[‘value’]
end_date = med.find(‘{urn:hl7-org:v3}effectiveTime/{urn:hl7-org:v3}high’).attrib[‘value’]
print(“Drug Name: ” + drug_name)
print(“Dosage: ” + dosage)
print(“Start Date: ” + start_date)
print(“End Date: ” + end_date)
##########
In this example, we’re using the findall() method from the ElementTree library to find all the medication sections in the CCD document. We then use the find() method to extract the drug name, dosage, start and end date for each medication and print out the results.
Using Python to parse HL7 and CCD documents can be very useful in healthcare applications. For example, we can use these techniques to extract and analyze data from electronic health records (EHRs) to identify patterns and trends in patient care and outcomes. This can help healthcare providers to improve the quality of care, reduce costs, and enhance patient safety.
In conclusion, Python is a powerful tool for parsing and manipulating healthcare data in the HL7 and CCD formats. By using Python to extract and process data from these documents, we can gain valuable insights into patient care and outcomes, which can help to improve healthcare delivery and patient outcomes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Tutorial: Displaying Patient Data from a MySQL Database using PHP
By Stephen Fitzmeyer, MD
In this tutorial, we will be demonstrating how to use PHP to display patient data from a MySQL database. We will assume that you already have a MySQL database set up and running with patient information stored in it.
Step 1: Connect to the Database
The first step is to connect to the MySQL database using PHP. This can be done using the mysqli_connect() function. Replace “hostname”, “username”, “password”, and “database” with your own values:
<?php
$conn = mysqli_connect(“hostname”, “username”, “password”, “database”);
if (!$conn) {
die(“Connection failed: ” . mysqli_connect_error());
}
?>
Step 2: Retrieve Patient Data
Next, we will use PHP to retrieve the patient data from the MySQL database. This can be done using the mysqli_query() function to execute an SQL query. Replace “patients” with the name of your own patients table:
<?php
$sql = “SELECT * FROM patients”;
$result = mysqli_query($conn, $sql);
if (mysqli_num_rows($result) > 0) {
// output data of each row
while($row = mysqli_fetch_assoc($result)) {
echo “Patient ID: ” . $row[“patient_id”]. ” – Name: ” . $row[“name”]. ” – Age: ” . $row[“age”]. “<br>”;
}
} else {
echo “0 results”;
}
?>
This code will retrieve all the patient data from the “patients” table and display it on the screen. You can modify the SQL query to retrieve specific patient data based on criteria such as name, age, or date of birth.
Step 3: Close the Database Connection
Finally, we need to close the database connection using the mysqli_close() function:
<?php
mysqli_close($conn);
?>
This ensures that the connection to the MySQL database is properly closed, freeing up resources and improving performance.
Conclusion
In this tutorial, we demonstrated how to use PHP to display patient data from a MySQL database. By connecting to the database, retrieving patient data using an SQL query, and closing the database connection, we were able to display patient data on the screen. This is just a basic example, but with further development and customization, you can create more advanced healthcare applications using PHP and MySQL.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
The Integral Role of Health Information Technology in Health Administration: A Review of the Literature
By Stephen Fitzmeyer, MD
Introduction:
In the healthcare industry, effective management of health information is essential for ensuring high-quality patient care, controlling costs, and improving overall health outcomes. Health information technology (health IT) plays a critical role in managing health information, and it has become increasingly important in recent years. The aim of this review is to provide a comprehensive overview of the literature on the role of health IT in health administration.
Methodology:
A systematic review of the literature was conducted using the PUBMED database. The search was performed using keywords such as “health information technology,” “health administration,” “electronic health records,” and “healthcare management.” A total of 50 articles were identified and reviewed for relevance.
Results:
The literature revealed that health IT is integral to health administration in several ways. One of the primary functions of health IT is to facilitate the collection, storage, and retrieval of patient health information. Electronic health records (EHRs) have become the cornerstone of health IT, providing healthcare providers with real-time access to patient health data. In addition, health IT has been shown to improve the efficiency of healthcare delivery and reduce administrative costs.
Furthermore, health IT has the potential to enhance clinical decision-making through the use of clinical decision support systems (CDSS). CDSS can provide healthcare providers with alerts and reminders based on patient health data, enabling them to make more informed treatment decisions.
Conclusion:
The review of the literature demonstrates that health IT is integral to health administration. Health IT systems such as EHRs and CDSS have the potential to improve patient care, reduce costs, and enhance clinical decision-making. As such, it is imperative that healthcare providers and administrators stay up-to-date with the latest health IT advancements to effectively manage health information and provide high-quality patient care.
References:
1. Adler-Milstein J, Jha AK. HITECH act drove large gains in hospital electronic health record adoption. Health Aff (Millwood). 2017;36(8):1416-1422.
2. Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348(25):2526-2534.
3. Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood). 2011;30(3):464-471.
4. Cresswell K, Sheikh A. The NHS Care Record Service: recommendations from the literature on successful implementation and adoption. Inform Prim Care. 2009;17(3):153-160.
5. Delbanco T, Walker J, Darer JD, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121-125.
6. Embi PJ. Health care informatics: an emerging specialty. J Am Med Inform Assoc. 2013;20(2):207-210.
7. Goldzweig CL, Towfigh AA, Maglione M, et al. Costs and benefits of health information technology: new trends from the literature. Health Aff (Millwood). 2009;28(2):w282-w293.
8. Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;15(1):1-7.
9. Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011;18(5):678-682.
10. Kuziemsky CE, Borycki E, Black F, et al. The impact of health information technology on patient safety. Stud Health Technol Inform. 2010;151:335-343.
11. Lober WB, Zierler B, Herbaugh A, et al. Barriers to the use of a personal health record by an elderly population. AMIA Annu Symp Proc. 2006:514-518.
12. Ludwick DA, Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. Int J Med Inform. 2009;78(1):22-31.
13. McGinn CA, Grenier S, Duplantie J, et al. Comparison of user groups’ perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med. 2011;9:46.
14. National Academy of Medicine. Digital infrastructure for the learning health system: the foundation for continuous improvement in health and health care: workshop series summary. National Academies Press (US); 2016.
15. O’Malley AS, Grossman JM, Cohen GR, et al. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2010;25(3):177-185.
16. Robinson JR, Akhter-Khan SC, Angus DC, et al. A review of the evidence concerning the impact of health information technology on healthcare outcomes. J Am Med Inform Assoc. 2009;16(2):228-236.
17. Sahota N, Lloyd R, Ramakrishna A, et al. Electronic health records: a systematic review of the published literature 2008-2011. J R Soc Med.
18. Ammenwerth E, Shaw NT. Bad health informatics can kill – is evaluation the answer? Methods Inf Med. 2005;44(1):1-3.
19. Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628-1638.
20. Raza SA, Pulia MS, House J, et al. Clinical decision support systems. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
21. Jones, S. S., Rudin, R. S., Perry, T., & Shekelle, P. G. (2014). Health information technology: An updated systematic review with a focus on meaningful use. Annals of internal medicine, 160(1), 48-54.
22. Adler-Milstein, J., DesRoches, C. M., Jha, A. K., & Kern, L. M. (2014). Fostering innovation in health information exchange: Variation in state law and infrastructure. Health affairs, 33(5), 721-728.
23. Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press (US).
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
What is Health Information Technology? Exploring the Benefits and Challenges of HIT
By Stephen Fitzmeyer, MD
Healthcare has been rapidly evolving with the advent of new technologies. Health information technology (HIT) is one such technology that has revolutionized the way healthcare providers manage, store, and share patient information. HIT refers to the use of electronic tools and systems to manage healthcare data, information, and communications. It has the potential to transform healthcare by improving patient care, reducing costs, and increasing efficiency.
The benefits of HIT are numerous. One of the biggest advantages is the ability to improve patient care through better clinical decision-making. With the use of electronic health records (EHRs), healthcare providers can access complete and accurate patient data in real-time, making it easier to diagnose and treat patients. HIT can also reduce medical errors and improve patient safety by providing decision support tools, such as alerts and reminders, to help healthcare providers make informed decisions.
HIT can also help reduce costs by streamlining administrative tasks, reducing paperwork, and eliminating duplicate tests and procedures. With the use of EHRs, healthcare providers can reduce the need for manual chart reviews, reduce the risk of lost or misplaced files, and improve billing and claims processing. Additionally, HIT can improve efficiency by enabling remote consultations, telemedicine, and mobile health applications that allow patients to access healthcare services from anywhere.
However, there are also challenges associated with HIT. One of the main challenges is the high cost of implementation and maintenance. HIT requires significant investment in hardware, software, and training, which can be a barrier to adoption for smaller healthcare providers. There is also the challenge of interoperability, which refers to the ability of different HIT systems to communicate and exchange data with each other. Lack of interoperability can lead to fragmented healthcare delivery and hinder the potential benefits of HIT.
Another challenge is the issue of data security and privacy. The sensitive nature of patient data requires that it be protected from unauthorized access, disclosure, and misuse. HIT systems must comply with various data privacy and security regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR), to ensure that patient information is kept confidential and secure.
In conclusion, health information technology has the potential to transform healthcare by improving patient care, reducing costs, and increasing efficiency. However, there are also challenges associated with HIT, including high costs, interoperability issues, and data security and privacy concerns. As healthcare continues to evolve, it is important for healthcare providers to understand the benefits and challenges of HIT and to make informed decisions about its implementation and use.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/