- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Diabetes
Unveiling the Differences: The Dawn Phenomenon vs. The Somogyi Effect in Diabetes Management
By Stephen Fitzmeyer, MD
Introduction:
Diabetes management encompasses various challenges, including understanding and addressing the intricacies of blood glucose fluctuations. Two phenomena that often perplex individuals with diabetes and healthcare professionals are the dawn phenomenon and the Somogyi effect. While both involve abnormal blood glucose levels, these phenomena differ in their timing, triggers, underlying mechanisms, and management strategies. In this article, we delve into these distinctions to shed light on the unique characteristics of the dawn phenomenon and the Somogyi effect in diabetes management.
The Dawn Phenomenon: An Early Morning Rise in Blood Glucose
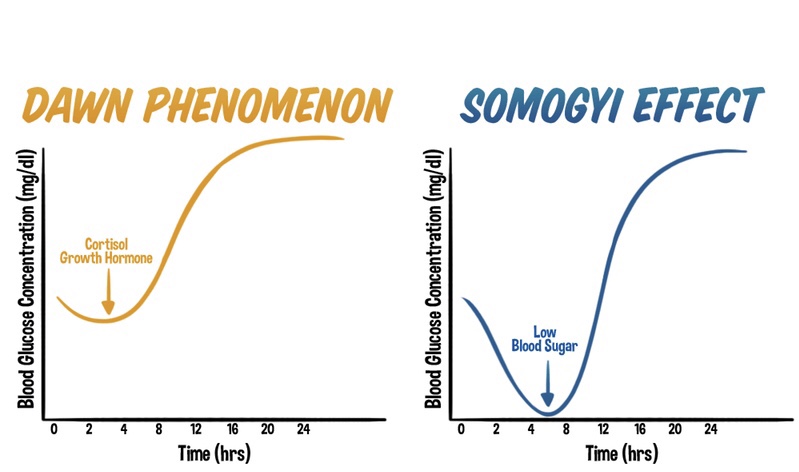
The dawn phenomenon is a well-known phenomenon observed in individuals with diabetes, characterized by an abnormal rise in blood glucose levels during the early morning hours, typically before waking up. Hormonal changes play a significant role in triggering this phenomenon. Increased release of hormones such as cortisol, growth hormone, and glucagon during the early morning hours leads to insulin resistance and stimulates gluconeogenesis. As a result, blood glucose levels rise without any preceding hypoglycemia.
The Somogyi Effect: Rebound Hyperglycemia Following Nocturnal Hypoglycemia
In contrast, the Somogyi effect involves a rebound hyperglycemia following a period of nocturnal hypoglycemia. This phenomenon occurs when blood glucose levels drop too low during the night, often due to excessive insulin administration or inadequate carbohydrate intake before bedtime. Nocturnal hypoglycemia triggers a counterregulatory response in the body, resulting in the release of hormones such as glucagon, cortisol, and growth hormone. These hormones stimulate gluconeogenesis and glycogenolysis, leading to a rebound rise in blood glucose levels during the morning or throughout the day.
Distinguishing Factors: Timing, Triggers, and Underlying Mechanisms
One of the primary distinctions between the dawn phenomenon and the Somogyi effect lies in their timing and triggers. The dawn phenomenon occurs during the early morning hours, driven by natural hormonal changes, while the Somogyi effect occurs as a response to nocturnal hypoglycemia.
Underlying mechanisms also differ between the two phenomena. The dawn phenomenon involves overactive gluconeogenesis as a contributing factor, as the liver produces glucose from non-carbohydrate sources. In contrast, the Somogyi effect encompasses a complex interplay of factors, including the release of counterregulatory hormones that stimulate both gluconeogenesis and glycogenolysis.
Management Strategies:
Effective management of the dawn phenomenon and the Somogyi effect requires tailored approaches based on their unique characteristics.
Managing the dawn phenomenon involves adjusting insulin regimens, specifically optimizing basal insulin doses during the early morning hours. Lifestyle modifications, including regular exercise, a balanced diet, and adequate sleep, can also aid in stabilizing blood glucose levels.
The management of the Somogyi effect requires identifying patterns of nocturnal hypoglycemia through consistent blood glucose monitoring. Adjusting insulin doses, timing, or types can prevent hypoglycemia and subsequent rebound hyperglycemia. Ensuring sufficient carbohydrate intake before bedtime and maintaining consistent sleep patterns are essential strategies in managing the Somogyi effect.
Conclusion:
Understanding the distinctions between the dawn phenomenon and the Somogyi effect is crucial in diabetes management. While both phenomena involve abnormal blood glucose fluctuations, their timing, triggers, underlying mechanisms, and management strategies differ significantly. Healthcare professionals play a vital role in recognizing these differences and tailoring individualized care plans to optimize blood glucose control. By comprehending the unique characteristics of the dawn phenomenon and the Somogyi effect, individuals with diabetes can work with their healthcare teams to effectively manage these phenomena and achieve improved overall well-being.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Navigating the Ketogenic Diet with Intermittent Fasting for Type 1 Diabetics: A Safe Approach to Managing Blood Sugar with Modern Technology
Introduction: Embracing a ketogenic diet, characterized by low carbohydrate intake and high fat consumption, along with intermittent fasting (IF), holds potential health benefits. But what about individuals with Type 1 Diabetes who rely on insulin for blood sugar management? Can they safely adopt a ketogenic lifestyle? In this article, we will explore how individuals with Type 1 Diabetes can safely navigate a ketogenic diet with the inclusion of intermittent fasting, ensuring stable blood sugar control and optimized health outcomes. With modern technology, such as the t:slim X2 Insulin Pump, monitoring blood sugars has become easier than ever.
Understanding Type 1 Diabetes and the Ketogenic Diet: Type 1 Diabetes is an autoimmune condition where the pancreas fails to produce sufficient insulin, resulting in high blood sugar levels. Traditionally, carbohydrate counting and insulin dosing have been vital for managing blood sugar. However, the ketogenic diet offers an alternative approach by minimizing carbohydrate intake, which can help stabilize blood sugar levels and reduce the need for large insulin doses.
Safely Adopting the Ketogenic Diet:
- Consult with Healthcare Professionals: Seek guidance from your healthcare team, including a registered dietitian and endocrinologist, to ensure a safe and effective transition to a ketogenic diet with intermittent fasting. They can provide personalized advice and help adjust insulin doses accordingly.
- Utilize Modern Technology: Take advantage of modern technology, such as the t:slim X2 Insulin Pump, which makes monitoring blood sugars easier than ever. This pump offers advanced features like continuous glucose monitoring (CGM) integration, insulin delivery adjustments, and data tracking, allowing for better management of blood sugar levels.
- Monitor Blood Sugar: Regularly monitor your blood sugar levels, especially during the initial stages of transitioning to a ketogenic diet. Frequent testing, combined with the convenience of devices like the t:slim X2 Insulin Pump, helps identify trends, make necessary insulin dose adjustments, and modify your diet accordingly.
- Individualized Carbohydrate Intake: Work with a registered dietitian experienced in managing diabetes to determine the appropriate carbohydrate limit for your specific needs, considering factors such as insulin sensitivity, activity levels, and overall health.
- Timing of Meals and Insulin: Intermittent fasting can be incorporated into the ketogenic diet, but it requires careful planning. Collaborate closely with your healthcare team to determine the best fasting and eating windows while considering insulin requirements and blood sugar control.
Benefits of Ketogenic Diet with IF for Type 1 Diabetics:
- Blood Sugar Stability: By reducing carbohydrate intake, individuals with Type 1 Diabetes may experience more stable blood sugar levels, reducing the risk of extreme highs and lows.
- Improved Insulin Sensitivity: The combination of a ketogenic diet and intermittent fasting may improve insulin sensitivity, making it easier to manage blood sugar levels and potentially reducing the need for high insulin doses.
- Weight Management: The ketogenic diet, coupled with intermittent fasting, may aid in weight management, which is beneficial for individuals with Type 1 Diabetes who may be at a higher risk of weight fluctuations.
- Potential for Fewer Complications: Maintaining stable blood sugar levels and reducing the need for high insulin doses may lower the risk of long-term complications associated with Type 1 Diabetes.
Conclusion: While the ketogenic diet and intermittent fasting hold potential benefits for individuals with Type 1 Diabetes, it is crucial to approach them with caution and under the guidance of healthcare professionals. With modern technology, such as the t:slim X2 Insulin Pump, monitoring blood sugars has become easier than ever, allowing for better control and management. Working closely with your healthcare team, including a registered dietitian and endocrinologist, will ensure a safe and effective transition to a ketogenic diet with intermittent fasting. Together, you can develop an individualized plan that considers your insulin requirements, blood sugar levels, and overall health goals. With the right support and modern tools at your disposal, it is possible for individuals with Type 1 Diabetes to safely embrace a ketogenic lifestyle and experience the potential benefits it offers in blood sugar management and overall well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
- ‹ Previous
- 1
- 2