- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Coronary Artery Disease
Protecting and Repairing the Glycocalyx: The Key to Vascular Health
Title: Protecting and Repairing the Glycocalyx: The Key to Vascular Health
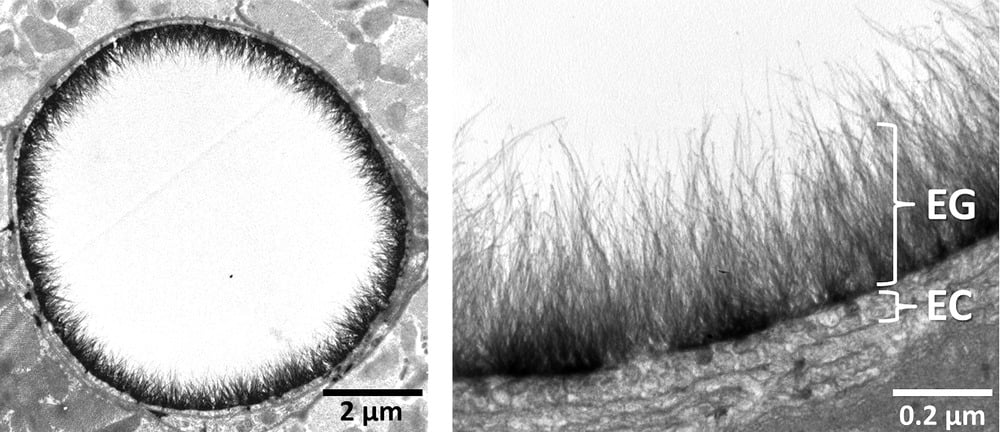
In recent years, the glycocalyx has gained attention in the health and wellness world, especially for its crucial role in vascular health. This thin, gel-like layer on the surface of cells, particularly on the endothelial cells lining our blood vessels, plays a vital role in keeping our blood vessels healthy and free from dangerous plaques. But what exactly is the glycocalyx, how does it get damaged, and, importantly, how can we repair it? Let’s dive into the science and strategies behind protecting this vital structure.
What Is the Glycocalyx?
The glycocalyx is a delicate, sugar-rich coating found on the surface of many cells. It’s particularly abundant on endothelial cells, which form the inner lining of blood vessels. Made of glycoproteins, glycolipids, and proteoglycans, the glycocalyx serves as a protective shield, helping to:
- Maintain smooth blood flow by reducing friction.
- Prevent blood cells and harmful substances like oxidized LDL (low-density lipoprotein) from sticking to vessel walls.
- Act as a barrier against pathogens.
- Enable cellular communication through various signaling molecules.
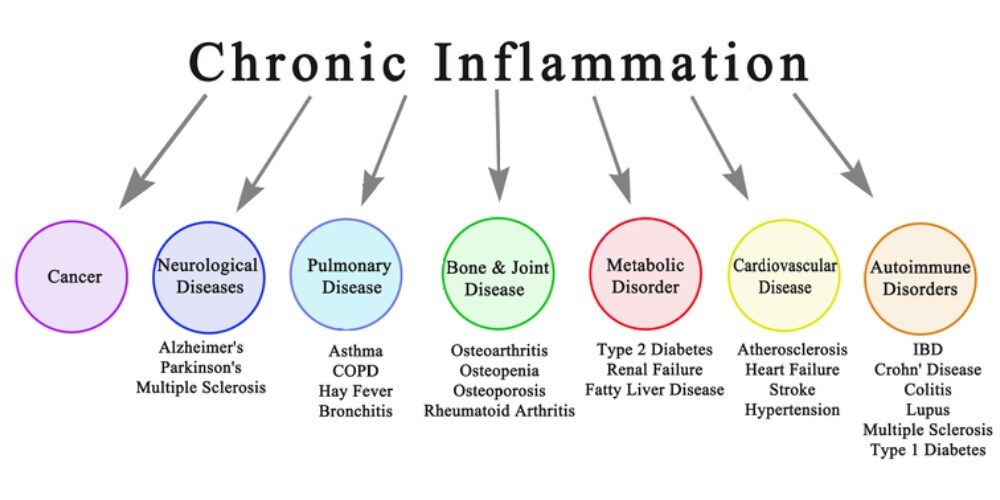
The glycocalyx is essentially the first line of defense for our blood vessels, safeguarding them from inflammation and damage. However, modern lifestyle factors can lead to glycocalyx damage, contributing to vascular diseases such as atherosclerosis.
How Does Glycocalyx Damage Lead to Plaque Buildup?
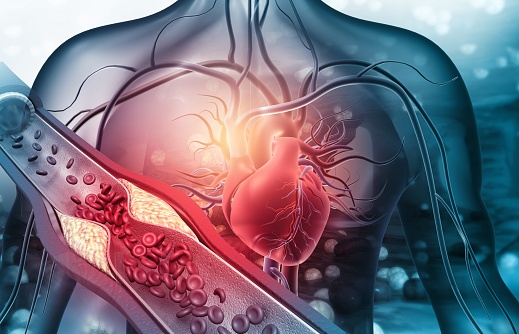
When the glycocalyx is damaged, it loses its integrity, making it easier for harmful molecules like oxidized LDL cholesterol to interact with the endothelial cells underneath. This damage can trigger an inflammatory response in the vessel wall, which can initiate plaque formation. Over time, as plaque builds up, it can restrict blood flow, leading to conditions like heart attacks, strokes, and other cardiovascular issues.
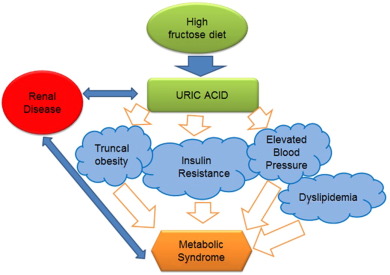
The Impact of High Blood Sugar and Fats on the Glycocalyx
Chronic high blood sugar, often seen in diabetes, and certain types of fats can contribute to glycocalyx damage. Here’s how:
- Oxidative Stress from Hyperglycemia:
- When blood sugar levels remain high, they trigger an overproduction of reactive oxygen species (ROS) in the endothelial cells. These molecules are highly reactive and can damage cellular structures, including the glycocalyx, by breaking down its carbohydrate components.
- Inflammation and Glycation:
- High blood sugar leads to the formation of advanced glycation end products (AGEs), which occur when glucose molecules bind to proteins and fats. These AGEs accumulate in blood vessels, directly interacting with and damaging the glycocalyx. They also activate receptors (RAGE) on endothelial cells, triggering inflammation and further degrading the glycocalyx.
- Excessive Omega-6 Intake and Inflammation:
- A high intake of omega-6 fatty acids, often from seed oils like soybean, corn, and sunflower oils, can shift the body toward a pro-inflammatory state. This imbalance between omega-6 and omega-3 fatty acids can increase inflammation that directly harms the glycocalyx.
- By creating an inflammatory response, omega-6 fatty acids contribute to oxidative stress and enzymatic activity that breaks down glycocalyx components. Replacing seed oils with anti-inflammatory fats, such as those found in olive oil, avocado oil, and fatty fish, can help protect the glycocalyx by reducing these inflammatory triggers.
- Enzymatic Degradation:
- Hyperglycemia and oxidative stress stimulate enzymes like heparanase and hyaluronidase, which break down the glycocalyx components such as heparan sulfate and hyaluronic acid, causing it to thin.
When the glycocalyx is compromised, the blood vessel becomes more permeable to cholesterol and other inflammatory molecules, leading to plaque buildup and increased cardiovascular risk.
The Role of Remnant Cholesterol and TG/HDL Ratios in Glycocalyx Assessment
For primary care providers (PCPs) and general practitioners (GPs), calculating a patient’s Remnant Cholesterol and Triglyceride-to-HDL (TG/HDL) ratio can provide a quick, valuable assessment of cardiovascular risk and potential glycocalyx damage. These indicators offer insight into lipid metabolism and inflammation, both of which affect the glycocalyx.
- Remnant Cholesterol: Calculated as total cholesterol minus LDL and HDL cholesterol, remnant cholesterol reflects the amount of triglyceride-rich lipoproteins. High levels are associated with increased risk of atherosclerosis and glycocalyx degradation, as these remnant particles can penetrate the endothelium and contribute to plaque formation.
- TG/HDL Ratio: The TG/HDL ratio is an easy-to-calculate marker of insulin resistance and metabolic health. High TG and low HDL levels often correlate with higher oxidative stress and systemic inflammation, both of which damage the glycocalyx. A TG/HDL ratio above 3.0 can indicate increased cardiovascular risk and a compromised glycocalyx.
Incorporating these markers into regular check-ups can help PCPs and GPs identify patients with higher glycocalyx damage risk, guiding preventive measures such as dietary adjustments, lifestyle changes, and early intervention.
Can the Glycocalyx Be Repaired?
The good news is that, while fragile, the glycocalyx can be repaired and maintained with the right dietary, lifestyle, and medical interventions. Here are some of the most effective strategies:
1. Control Blood Sugar Levels
- Dietary Changes: Reducing refined carbohydrates and sugars is essential for maintaining blood sugar levels. A diet focused on whole, unprocessed foods with a low glycemic index can minimize blood sugar spikes and the resulting oxidative stress.
- Exercise: Physical activity improves insulin sensitivity, helping regulate blood glucose and reduce glycocalyx damage from hyperglycemia.
- Medications: For individuals with diabetes, medications like metformin can help keep blood glucose within a healthy range, reducing the risk of glycocalyx damage.
2. Boost Antioxidants
- Vitamin C and E: These antioxidants help neutralize ROS, protecting the glycocalyx from oxidative damage.
- Polyphenols: Found in foods like berries, green tea, and dark chocolate, polyphenols have anti-inflammatory properties and protect the glycocalyx from ROS. Resveratrol, a specific polyphenol in red wine, is known for supporting vascular health and glycocalyx repair.
- Omega-3 Fatty Acids: Known for their anti-inflammatory effects, omega-3s (found in fatty fish and fish oil supplements) help reduce inflammation and protect the glycocalyx from enzymatic degradation. They also help stabilize the endothelial cells, reducing breakdown of glycocalyx components.
3. Support Glycocalyx Health with Key Nutrients
- L-arginine: This amino acid boosts nitric oxide production, which improves endothelial function and supports glycocalyx repair.
- Hyaluronic Acid and Chondroitin Sulfate: These are essential building blocks of the glycocalyx, often found in joint supplements. They support glycocalyx structure and help it retain moisture, keeping it intact and functional.
- Sulfur-Rich Foods: Garlic, onions, and cruciferous vegetables contain sulfur, which supports the synthesis of glycosaminoglycans, vital components of the glycocalyx.
4. Adopt a Low-Carb Lifestyle and Eliminate Inflammatory Foods
A low-carb lifestyle, with the elimination of seed oils, grains, and sugars, is especially beneficial for glycocalyx health:
- Reduced Blood Sugar Spikes: Limiting carbohydrate intake stabilizes blood sugar, preventing the oxidative stress associated with high blood glucose. This lowers the formation of AGEs and reduces direct damage to the glycocalyx.
- Improved Insulin Sensitivity: A low-carb approach, often combined with exercise, enhances insulin sensitivity, allowing cells to better utilize glucose, thereby keeping blood sugar stable and minimizing glycocalyx damage.
- Eliminating Seed Oils: Seed oils, high in omega-6 fatty acids, are inflammatory when consumed in excess. By replacing these oils with healthy fats (like olive oil, avocado oil, and butter), inflammation can be reduced, preserving glycocalyx health.
- Removing Grains and Sugars: High-glycemic grains and sugars contribute to glycation, leading to AGEs that harm the glycocalyx. Focusing on nutrient-dense vegetables and quality proteins provides energy without causing the blood sugar spikes that damage vascular health.
5. Avoid Harmful Substances
- Reduce Inflammatory Fats: Trans fats and excessive omega-6 fats (commonly found in processed seed oils) contribute to inflammation that damages the glycocalyx. Focusing on anti-inflammatory fats like olive oil, avocado oil, and omega-3-rich foods can support vascular health.
- Limit Smoking and Alcohol: Both smoking and excessive alcohol increase oxidative stress and inflammation, damaging the glycocalyx. Avoiding these substances is key for vascular and overall health.
6. Explore Emerging Therapies and Supplements
- Glycocalyx-Targeted Supplements: Some supplements aim to support glycocalyx health directly with compounds like glycosaminoglycans, which are essential to its structure. These “endocalyx” supplements may help repair and strengthen the glycocalyx.
- Stem Cell and Regenerative Therapies: Though still in experimental stages, stem cell and regenerative therapies hold promise for repairing damaged glycocalyx in severe cases.
- Nitric Oxide (NO) Enhancing Therapies: Therapies that boost NO production in the endothelium are being researched for their potential to help restore glycocalyx health and improve overall vascular function.
The Path Forward for Glycocalyx Health
Protecting and repairing the glycocalyx is crucial for maintaining vascular health and preventing the progression of plaque buildup. By focusing on blood sugar control, boosting antioxidants, incorporating essential nutrients, and utilizing key indicators like Remnant Cholesterol and TG/HDL ratios, we can help assess, repair, and protect this delicate structure to support cardiovascular wellness. A low-carb lifestyle, especially one that excludes seed oils, grains, and sugars, provides even greater protection, creating conditions that allow the glycocalyx to repair and thrive.
As research continues, our understanding of the glycocalyx and its role in health will expand, unlocking even more ways to protect this remarkable structure and the vital functions it supports. By nurturing the glycocalyx, we’re investing in the foundation of our cardiovascular health, giving us a powerful tool for longevity and well-being.
Unveiling the Role of ApoB and the Therapeutic Potential of Ketogenic Lifestyle and Intermittent Fasting in Atherosclerosis
By Stephen Fitzmeyer, MD
Introduction:
Atherosclerosis, a major contributor to cardiovascular disease, arises from a complex interplay of various factors. Among them, Apolipoprotein B (ApoB) emerges as the primary driver in the development and progression of this condition. In this article, we delve into the critical role of ApoB in atherosclerosis and shed light on the influence of inflammation in enhancing its effects.
Understanding the Role of ApoB:
ApoB, a protein found in lipoproteins such as low-density lipoprotein (LDL) particles, serves as a key player in atherosclerosis. It acts as a carrier, facilitating the transportation of cholesterol to peripheral tissues, including the arterial walls. In the absence of ApoB, the initiation and progression of atherosclerosis are virtually non-existent.
The Significance of ApoB in Atherosclerosis:
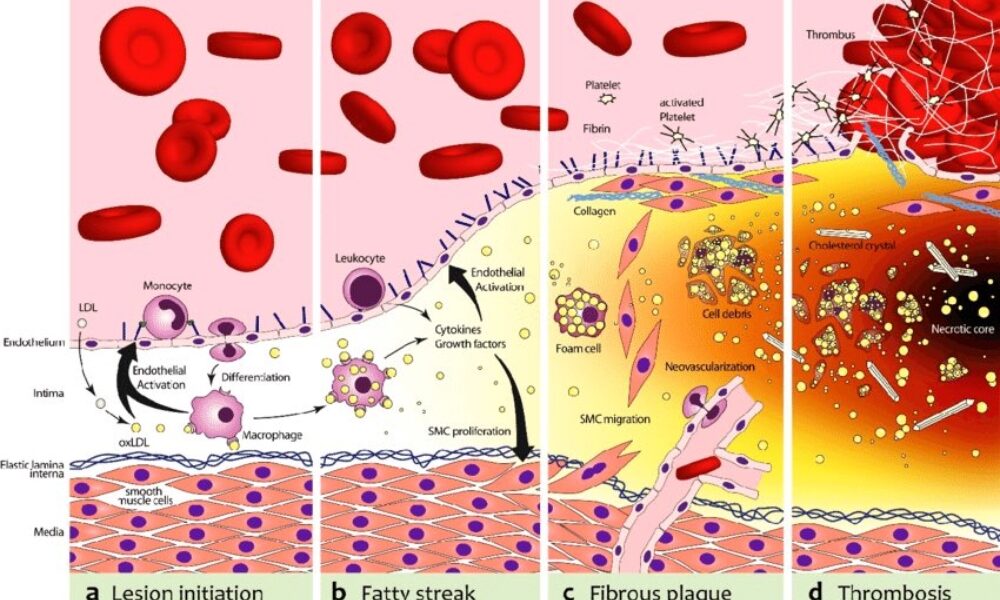
ApoB takes center stage in atherosclerosis, as it is responsible for delivering cholesterol-rich lipoproteins, particularly LDL, to arterial walls. These lipoproteins undergo modifications and become trapped in the arterial intima, initiating the formation of fatty streaks. With time, inflammation is triggered, attracting immune cells and accelerating the transformation of fatty streaks into advanced atherosclerotic plaques.
Inflammation and its Role:
While inflammation is a key player in atherosclerosis, it acts as an enhancer rather than the primary driver. Inflammation exacerbates the process by promoting the retention and modification of ApoB-containing lipoproteins, leading to plaque progression and instability. Thus, controlling inflammation becomes crucial in managing atherosclerosis, but addressing the root cause—ApoB—remains essential.
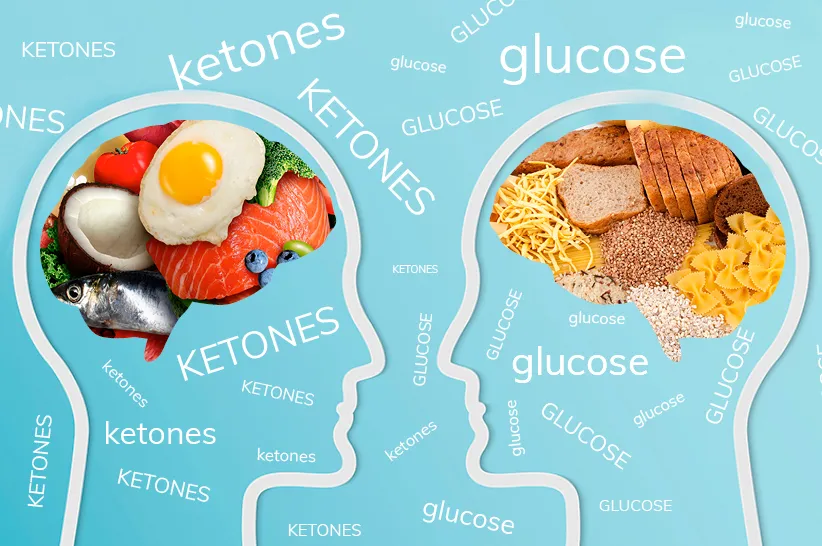
Implications and Therapeutic Strategies:
Understanding the central role of ApoB opens up avenues for therapeutic interventions in managing atherosclerosis. Addressing ApoB levels and reducing the burden of cholesterol-rich lipoproteins is key. Here, lifestyle modifications such as adopting a low-carbohydrate, high-fat diet (such as a ketogenic diet) and implementing intermittent fasting can prove beneficial. These approaches help regulate ApoB-containing lipoproteins, mitigate their retention in arterial walls, and slow down the progression of atherosclerosis.
Furthermore, lifestyle modifications that target additional risk factors associated with atherosclerosis, such as hypertension and obesity, should be considered. Engaging in regular physical activity, maintaining a healthy weight, and managing other comorbidities can complement the efforts to address ApoB and reduce the overall risk of atherosclerosis.
Conclusion:
ApoB stands as the primary driver in the initiation and progression of atherosclerosis, while inflammation serves to enhance and accelerate the process. Recognizing the pivotal role of ApoB provides insights into therapeutic strategies that can mitigate its effects. By adopting lifestyle modifications, such as a low-carbohydrate, high-fat diet and intermittent fasting, individuals can positively influence ApoB levels and manage atherosclerosis. Combining these interventions with measures to address other risk factors offers a comprehensive approach to reducing the burden of atherosclerosis and promoting cardiovascular health.
The biochemical pathway of plaque formation involving ApoB can be described as follows:
- ApoB synthesis: ApoB is a protein synthesized in the liver and intestines. It is a major component of very low-density lipoprotein (VLDL) and LDL particles.
- Lipoprotein assembly: VLDL particles are assembled in the liver and contain ApoB-100. They transport triglycerides and cholesterol from the liver to peripheral tissues. During circulation, VLDL particles undergo enzymatic changes, resulting in the conversion of triglycerides into free fatty acids and glycerol.
- LDL formation: As VLDL particles lose triglycerides, they become smaller and denser, transforming into LDL particles. LDL contains a single molecule of ApoB-100 and is the primary carrier of cholesterol in the bloodstream.
- LDL uptake: LDL particles bind to LDL receptors on cell surfaces, allowing the cells to take up cholesterol. These receptors are present in various tissues, including the arterial walls.
- Retention and modification: In the arterial walls, LDL particles can undergo modifications, such as oxidation and glycation, making them more prone to retention. These modified LDL particles interact with extracellular matrix proteins and proteoglycans in the arterial intima, leading to their entrapment within the vessel walls.
- Inflammation and foam cell formation: The retained LDL particles, along with their cholesterol content, trigger an inflammatory response. Immune cells, particularly macrophages, migrate to the site of inflammation. They engulf the cholesterol-rich LDL particles, transforming into foam cells, which are characterized by their lipid-filled cytoplasm.
- Fatty streak formation: The accumulation of foam cells and other immune cells results in the formation of fatty streaks, which are the initial visible signs of plaque development. Fatty streaks consist of foam cells, lipids, inflammatory cells, and smooth muscle cells.
- Advanced plaque formation: Over time, the fatty streaks can progress into more advanced atherosclerotic plaques. These plaques are characterized by a fibrous cap composed of smooth muscle cells and collagen, a lipid-rich core containing foam cells and cholesterol, and a necrotic center.
Throughout this biochemical pathway, ApoB plays a crucial role in the transport of cholesterol to peripheral tissues, including the arterial walls. It facilitates the delivery of cholesterol-rich LDL particles, which, under certain conditions, contribute to the formation of atherosclerotic plaques. Understanding this pathway provides valuable insights into potential therapeutic targets for preventing and managing plaque formation and related cardiovascular diseases.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
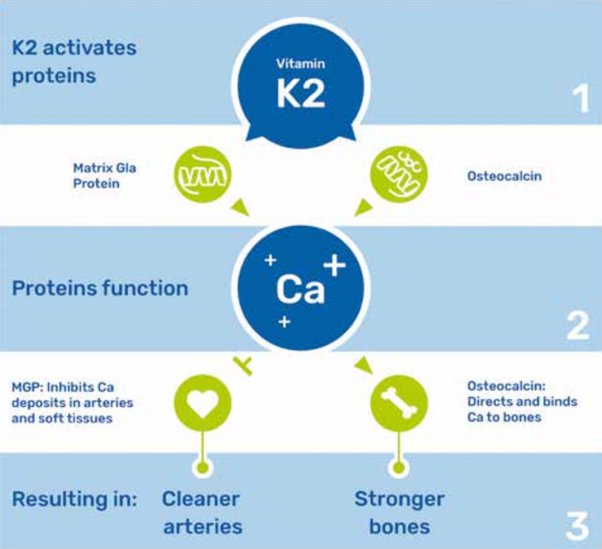
Unlocking the Benefits of Vitamin K2: Clearing Arterial Calcium and Achieving a CAC Score of Zero
by Stephen Fitzmeyer
Introduction: Maintaining cardiovascular health is a top priority for many individuals seeking to lead a long and vibrant life. While regular exercise, a balanced diet, and a healthy lifestyle are crucial elements, recent research has shed light on the potential benefits of vitamin K2 in promoting arterial health. In this article, we delve into the role of vitamin K2 in clearing calcium from arteries, leading to the desirable achievement of a coronary artery calcium (CAC) score of zero.
Understanding the Role of Calcium in Arteries: Calcium is an essential mineral for our body, contributing to the formation and strength of bones and teeth. However, when calcium starts accumulating in arterial walls, it can lead to the formation of plaque, narrowing the arteries and hindering blood flow. This process, known as arterial calcification, is a significant risk factor for cardiovascular diseases, including heart attacks and strokes.
Vitamin K2: A Key Player in Arterial Health: Emerging research suggests that vitamin K2 plays a crucial role in maintaining arterial health by effectively managing calcium levels in the body. Vitamin K2 activates proteins that shuttle calcium away from arteries and deposit it in bones, where it is needed. By doing so, vitamin K2 helps to prevent and even reverse arterial calcification.
Clearing Arterial Calcium with Vitamin K2: One of the most remarkable aspects of vitamin K2 is its potential to clear existing arterial calcium deposits. Studies have shown that by ensuring an adequate intake of vitamin K2, individuals with arterial calcification may experience a reduction in the severity of plaque buildup over time. This can lead to improved arterial flexibility and reduced cardiovascular risks.
Achieving a CAC Score of Zero: A coronary artery calcium (CAC) score is a measure of the amount of calcium buildup in the coronary arteries. A score of zero indicates no detectable calcium, which is considered an optimal outcome. While multiple factors contribute to achieving a CAC score of zero, including lifestyle choices and genetics, incorporating vitamin K2 into your routine may play a significant role in promoting arterial health and minimizing calcium deposits.
How to Incorporate Vitamin K2 into Your Routine: To maximize the potential benefits of vitamin K2, it is important to ensure an adequate intake of this nutrient. Vitamin K2 can be found in certain foods, including fermented dairy products, organ meats, and certain cheeses. However, for those who may have limited access to these sources or have dietary restrictions, vitamin K2 supplements are widely available and offer a convenient way to meet the recommended daily intake.
Consult with a Healthcare Professional: As with any dietary change or supplement regimen, it is important to consult with a healthcare professional before incorporating vitamin K2 into your routine. They can assess your individual health needs, provide guidance on appropriate dosages, and help monitor the progress of arterial health through regular check-ups and assessments.
Conclusion: Achieving optimal arterial health and aiming for a CAC score of zero is a significant goal for cardiovascular well-being. While there are multiple factors at play, emerging research highlights the potential of vitamin K2 in promoting arterial health and clearing arterial calcium. By incorporating vitamin K2 into your routine and consulting with a healthcare professional, you can take proactive steps towards supporting your cardiovascular health and enjoying a life free from the burden of arterial calcification.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
CAC: The Ultimate Test for Assessing Health and Why You Need One Now!
By Stephen Fitzmeyer, MD
Introduction
In the realm of healthcare, staying proactive and prioritizing preventive measures is key to maintaining optimal health. The Coronary Artery Calcium (CAC) scoring test has recently emerged as a groundbreaking tool in health assessment, providing invaluable insights into cardiovascular health. This article highlights the significance of CAC as the ultimate test for assessing health and emphasizes why individuals should consider getting one now to safeguard their well-being. Additionally, we’ll explore how patients can easily obtain a CAC scan for themselves.
Understanding CAC Scoring
The Coronary Artery Calcium (CAC) scoring test employs non-invasive computed tomography (CT) scans to detect the presence and extent of calcified plaque in the coronary arteries. By quantifying the amount of calcium present, it calculates a CAC score, effectively gauging the overall burden of atherosclerosis in the arteries. This score serves as a crucial predictor of cardiovascular disease (CVD), empowering individuals to take preventive action.
The Urgency of CAC as a Health Indicator
- Early Detection of Silent Risks: CAC scoring enables early detection of potential cardiovascular issues, even before symptoms manifest. By identifying calcified plaque deposits, healthcare professionals can determine an individual’s risk of experiencing a heart attack or developing coronary artery disease (CAD). Seeking a CAC test now can help unveil hidden risks and prompt timely interventions to prevent disease progression.
- Personalized Risk Assessment: Unlike traditional risk assessment tools, CAC scoring provides a precise evaluation of atherosclerosis. Through quantitative analysis, it offers a more accurate estimation of an individual’s risk of developing CVD. Obtaining a CAC score now empowers healthcare providers to devise personalized treatment plans tailored to an individual’s level of risk, enabling timely interventions and better health outcomes.
- Empowerment for Lifestyle Changes: CAC scoring serves as a powerful motivator for individuals to adopt healthier lifestyles. Witnessing the presence and extent of calcified plaque acts as a visual reminder of the importance of positive changes in diet, exercise, and stress management. By getting a CAC test now, you can proactively take charge of your health, making informed decisions and fostering long-term adherence to beneficial lifestyle modifications.
- Preventive Measures for Long-Term Health: CAC scoring facilitates proactive preventive measures by categorizing individuals into different risk groups based on their CAC scores. This allows healthcare providers to implement appropriate treatments and interventions to reduce the risk of CVD. Taking action now, based on your CAC score, can significantly improve your long-term cardiovascular health and well-being.
How to Obtain a CAC Scan
To obtain a CAC scan, you can follow these steps:
- Consult Your Healthcare Provider: Schedule an appointment with your healthcare provider to discuss your interest in getting a CAC scan. They will evaluate your medical history, risk factors, and overall health to determine if a CAC scan is appropriate for you.
- Referral and Imaging Facility: If your healthcare provider determines that a CAC scan is necessary, they will provide you with a referral to an imaging facility or radiology center equipped to perform the scan.
- Schedule the Scan: Contact the recommended imaging facility and schedule your CAC scan appointment. They will provide you with any necessary instructions, such as fasting requirements or medication restrictions before the test.
- The CAC Scan Procedure: During the CAC scan, you will lie on a table that moves through a CT scanner. The scan is quick and painless, typically taking only a few minutes to complete.
- Results and Follow-up: Once the scan is complete, the radiologist will analyze the images and calculate your CAC score. Your healthcare provider will then review the results with you. They will explain the implications of your CAC score, discuss any necessary lifestyle modifications or medical interventions, and develop a personalized plan to mitigate your cardiovascular risk.
Conclusion
The Coronary Artery Calcium (CAC) scoring test is a powerful tool for assessing cardiovascular health and preventing future complications. By identifying silent risks, providing personalized risk assessment, motivating lifestyle changes, and enabling proactive preventive measures, CAC scoring empowers individuals to take control of their well-being. To obtain a CAC scan, consult your healthcare provider, obtain a referral to an imaging facility, schedule the scan, and discuss the results and follow-up plan with your healthcare provider. Take the proactive step towards optimizing your health and consider getting a CAC scan now. Your heart and overall well-being will thank you for it.
CAC Score
After undergoing a CAC scan, you will receive a CAC score that falls within a specific range. Here are the general ranges and their corresponding meanings:
- CAC Score of 0: A CAC score of 0 indicates the absence of detectable calcified plaque in the coronary arteries. This suggests a very low risk of cardiovascular events, and individuals in this range often have a favorable prognosis.
- CAC Score of 1-99: A CAC score between 1 and 99 indicates the presence of mild calcification in the coronary arteries. This range signifies a low to moderate risk of cardiovascular disease, and it is an opportunity for individuals to implement preventive measures to reduce the progression of plaque formation.
- CAC Score of 100-399: A CAC score between 100 and 399 represents the presence of moderate calcification in the coronary arteries. This range suggests a significant risk of cardiovascular disease, and it necessitates more aggressive preventive strategies and medical interventions to reduce the risk of future complications.
- CAC Score of 400 or Higher: A CAC score of 400 or higher indicates extensive calcification in the coronary arteries. This range represents a high risk of cardiovascular disease, including heart attacks and strokes. It necessitates immediate and intensive medical interventions, including lifestyle modifications and potential medication therapies, to mitigate the risk and prevent further progression.
By understanding the range of CAC scores and their implications, individuals can work closely with their healthcare providers to develop a personalized plan that addresses their specific risk level.
To obtain a CAC scan, consult your healthcare provider, obtain a referral to an imaging facility, schedule the scan, and discuss the results and follow-up plan with your healthcare provider. Take the proactive step towards optimizing your health and consider getting a CAC scan now. Your heart and overall well-being will thank you for it.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/