- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Clinical Informatics
The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
Healthcare is at a pivotal moment in history, where technological innovation is redefining how care is delivered, managed, and optimized. At the core of this revolution are Artificial Intelligence (AI), Clinical Informatics, and Machine Learning (ML), fields that intersect to create a paradigm shift in the way we approach health and wellness. This confluence has the potential to enhance decision-making, streamline operations, and improve patient outcomes.
1. Transforming Healthcare Through
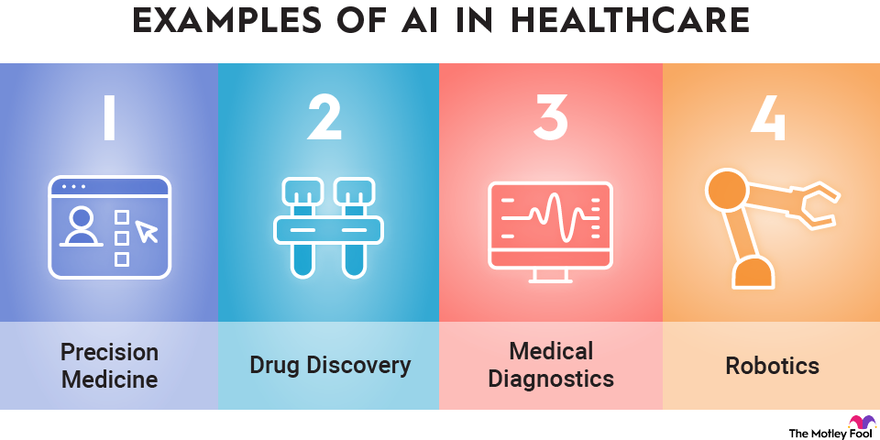
AI brings an unprecedented ability to process and analyze large datasets with speed and accuracy that no human could match. In healthcare, AI is being applied to areas such as:
- Predictive Analytics: AI algorithms can predict patient outcomes based on historical data, enabling proactive intervention. For example, models trained on electronic health record (EHR) data can forecast hospital readmissions or identify patients at risk for chronic diseases.
- Medical Imaging: AI-powered tools can analyze X-rays, MRIs, and CT scans, often detecting anomalies with greater precision than human radiologists.
- Personalized Medicine: AI tailors treatment plans by analyzing genetic, lifestyle, and environmental factors. This ensures therapies are as effective as possible for individual patients.
2. The Role of Clinical Informatics
Clinical Informatics is the backbone of data-driven decision-making in healthcare. It focuses on the optimal use of information and technology to improve patient care and health outcomes. Informatics integrates with AI and ML in several ways:
- Data Integration: Informatics ensures the seamless aggregation and harmonization of diverse healthcare data sources, from EHRs to wearable devices.
- Interoperability: The field promotes standards and protocols that allow AI systems to access and utilize data across different platforms and institutions.
- Clinical Decision Support Systems (CDSS): Informatics integrates AI-driven insights into clinician workflows, enabling smarter, faster, and more accurate decisions at the point of care.
3. Machine Learning as the Engine of Innovation
Machine Learning, a subset of AI, excels at identifying patterns in data and making predictions. In healthcare, ML applications are advancing at a rapid pace:
- Drug Discovery: ML accelerates drug development by predicting how compounds interact with biological systems, reducing the time and cost of bringing new medications to market.
- Operational Efficiency: Hospitals are using ML to optimize staffing, predict supply needs, and improve resource allocation, reducing waste and enhancing patient experiences.
- Natural Language Processing (NLP): ML-powered NLP systems analyze unstructured clinical notes, turning them into actionable insights. This has implications for billing, compliance, and clinical documentation.
4. Ethical and Practical Considerations
While the potential of AI, ML, and Clinical Informatics in healthcare is vast, it is not without challenges:
- Data Privacy and Security: With vast amounts of sensitive health data being processed, ensuring robust cybersecurity measures is critical.
- Bias in Algorithms: AI systems trained on biased datasets can perpetuate disparities in care. Diverse data representation is essential to mitigate this risk.
- Clinician Adoption: Integrating AI tools into clinical practice requires buy-in from healthcare professionals. These tools must be user-friendly and provide clear, actionable insights.
5. The Future of Healthcare
The intersection of AI, Clinical Informatics, and ML is laying the groundwork for a healthcare system that is:
- More Predictive: By identifying health issues before they become critical, we can move from reactive to preventive care.
- More Personalized: Treatments will be increasingly tailored to the unique characteristics of each patient.
- More Efficient: Automation of administrative tasks will allow clinicians to focus more on patient care.
Conclusion
The synergy between AI, Clinical Informatics, and Machine Learning is transforming healthcare into a smarter, more adaptive system. These technologies are not merely tools but catalysts for innovation, enabling a future where healthcare is not only more efficient but also more human.
As we navigate this new frontier, the focus must remain on ensuring ethical implementation, fostering trust among stakeholders, and keeping the patient at the center of every innovation.
How AI Can Transform Healthcare Applications
How AI Can Transform Healthcare Applications
As a developer of healthcare applications, you’re constantly looking for ways to improve functionality, efficiency, and user experience. Artificial Intelligence (AI) offers a transformative opportunity to enhance healthcare apps, making them smarter, more user-friendly, and impactful. Here’s how AI can elevate your healthcare applications to the next level.
1. Enhancing Patient Care and Management
- Personalized Treatment Recommendations: AI algorithms analyze patient data like lab results, genetic information, and medical history to suggest tailored treatment plans.
- Virtual Assistants: Chatbots powered by natural language processing (NLP) can answer common patient questions, help schedule appointments, and remind patients about medications.
- Predictive Analytics: AI models predict potential health issues, such as diabetes or cardiovascular disease, allowing for early intervention and better patient outcomes.
2. Supporting Clinical Decision-Making
- AI Diagnosis Tools: Machine learning can analyze medical images, lab tests, or patient-reported symptoms to help identify conditions quickly and accurately.
- Drug Interaction Alerts: AI systems can flag potential drug interactions or contraindications based on a patient’s medication history.
- Risk Assessment Models: Predictive models assess patient risks for conditions like stroke or sepsis, enabling proactive care.
3. Optimizing Workflow
- Automated Documentation: NLP tools transcribe and summarize doctor-patient conversations, reducing administrative burdens.
- Intelligent Scheduling: AI-powered tools optimize staff and appointment scheduling, minimizing wait times and maximizing resource utilization.
- Claims Automation: Automate insurance claim reviews with AI, reducing errors and speeding up reimbursement processes.
4. Enhancing Telemedicine and Remote Monitoring
- AI Diagnostics: Enhance telehealth platforms with tools that analyze patient-reported data or uploaded images during virtual consultations.
- Wearable Data Integration: Develop AI algorithms to process data from wearables, offering actionable insights into patient health.
- Symptom Checkers: AI-driven tools allow patients to input symptoms and receive preliminary assessments, streamlining triage.
5. Delivering Data Insights and Analytics
- Patient Cohort Analysis: AI identifies patterns in patient populations, improving treatment strategies and research.
- Health Trend Forecasting: Analyze big data to predict public health trends or disease outbreaks.
- Operational Efficiency: Use AI to optimize inventory, staffing, and resource allocation in clinical settings.
6. Improving Patient Engagement
- Conversational Interfaces: Enable patients to interact with your app through natural language queries, making healthcare more accessible.
- Gamification: Use AI to personalize gamified elements, encouraging adherence to treatment plans or healthy behaviors.
- Educational Content: Deliver tailored educational materials based on a patient’s condition or interests.
7. Ensuring Compliance and Security
- Data Anonymization: AI can de-identify sensitive patient data for compliance with regulations like HIPAA and GDPR.
- Fraud Detection: AI detects anomalies in billing or prescriptions that may indicate fraud.
- Secure Data Sharing: Facilitate secure and efficient sharing of patient records among healthcare providers.
8. Facilitating Research and Development
- Clinical Trial Matching: Match eligible patients to clinical trials using AI-driven analysis of their medical profiles.
- Drug Discovery: Use AI models to simulate and analyze potential drug compounds.
- Real-World Evidence: Generate insights from patient data to support post-market surveillance and drug efficacy studies.
9. Expanding Accessibility
- Language Translation: Offer multilingual support for diverse patient populations with AI translation tools.
- Accessibility Features: Build AI-driven speech-to-text and text-to-speech features for patients with disabilities.
10. Elevating User Experience
- Predictive Navigation: Anticipate user actions to streamline navigation and improve usability.
- Behavioral Nudges: Deliver proactive reminders or nudges, such as medication adherence prompts, based on user behavior.
- Dynamic Interfaces: Personalize app interfaces based on user preferences and engagement patterns.
Example: Implementing an AI-Powered Symptom Checker
Here’s an example of how you might structure an app to include a symptom checker using AI:
- Input Collection: The app asks users to input symptoms via text or voice.
- Natural Language Processing (NLP): AI processes the input to extract relevant medical terms and symptoms.
- Symptom Analysis: The app uses a machine learning model trained on a medical dataset to compare the user’s symptoms with known patterns of illnesses.
- Recommendation Engine: Based on the analysis, the app provides possible conditions and suggests whether the user should seek immediate care, consult a doctor, or try home remedies.
- Continuous Learning: The app collects anonymized feedback from user interactions to improve the accuracy of the model over time.
Example Code for NLP Symptom Processing:
from transformers import pipeline
# Load a pre-trained NLP model for healthcare applications
nlp_model = pipeline("text-classification", model="bert-base-healthcare")
# Example user input
user_input = "I have a persistent cough and shortness of breath."
# Process the input
analysis = nlp_model(user_input)
# Output AI-generated insights
print("Potential conditions:", analysis)
This code snippet demonstrates how to use a pre-trained NLP (Natural Language Processing) model from the Hugging Face transformers library to classify text related to healthcare applications. Here’s a breakdown of what each part of the code does:
1. Importing pipeline from the transformers library
from transformers import pipelineThe pipeline function provides an easy interface to use pre-trained models for various NLP tasks like text classification, question answering, translation, etc.
2. Loading a Pre-trained NLP Model
nlp_model = pipeline("text-classification", model="bert-base-healthcare")pipeline("text-classification"): This specifies that the task is text classification, where input text will be categorized into predefined classes or labels.model="bert-base-healthcare": Refers to a pre-trained BERT (Bidirectional Encoder Representations from Transformers) model fine-tuned for healthcare-related text classification. This specific model would likely be trained to understand healthcare vocabulary and contexts.
3. Processing User Input
user_input = "I have a persistent cough and shortness of breath."
analysis = nlp_model(user_input)The pipeline processes the input text using the loaded model to predict potential conditions or categories related to the input.
4. Outputting Results
print("Potential conditions:", analysis)The analysis variable contains the model’s predictions, such as potential health conditions or relevant categories for the provided symptoms.
Example Output
Potential conditions: [{'label': 'Respiratory Issue', 'score': 0.95}]- label: The predicted category (e.g., “Respiratory Issue”).
- score: The confidence score for this prediction (e.g., 0.95, indicating 95% confidence).
Use Case
This code can be part of a healthcare chatbot, clinical decision support system, or any application designed to provide preliminary insights based on patient symptoms. However, these AI-generated insights should not replace professional medical advice.
Getting Started with AI Integration
To start incorporating AI into your healthcare applications:
- Start Small: Begin with a single AI feature, such as a chatbot or predictive analytics, to test feasibility and user acceptance.
- Prioritize Data Quality: Ensure clean, accurate data to power your AI models effectively.
- Focus on Ethics: Build trust by maintaining transparency, privacy, and fairness in AI algorithms.
- Iterate and Scale: Use feedback to refine AI functionalities and expand capabilities over time.
AI is reshaping healthcare, offering exciting opportunities to create more impactful applications. By leveraging AI, you can provide better care, improve efficiency, and drive innovation in healthcare technology.
Unlocking the Power of Health Informatics: Why It Matters
Introduction
Health informatics is a rapidly growing field that combines healthcare, information technology, and data science to transform the way we manage and utilize health-related information. In the digital age, health informatics plays a pivotal role in enhancing patient care, improving healthcare processes, and driving medical research. In this article, we delve into the importance of health informatics and the manifold ways in which it positively impacts the healthcare industry.
Enhanced Patient Care
Health informatics improves patient care by providing healthcare professionals with instant access to accurate and up-to-date patient information. Electronic Health Records (EHRs) store patient histories, test results, medications, and treatment plans, reducing the risk of medical errors and ensuring that the right treatment is delivered to the right patient.
Efficient Healthcare Processes
Health informatics streamlines administrative and clinical processes in healthcare. It reduces paperwork, automates scheduling and billing, and facilitates communication among healthcare providers. This efficiency not only saves time but also reduces costs, making healthcare more accessible.
Data-Driven Decision-Making
Health informatics leverages data analysis to inform healthcare decisions. By analyzing trends and patterns, healthcare providers can make more informed choices about patient care and resource allocation, ultimately improving patient outcomes.
Telemedicine and Remote Monitoring
The integration of health informatics in telemedicine enables remote consultations and monitoring of patients. This is particularly crucial in reaching patients in underserved or remote areas, providing access to quality healthcare that might otherwise be unattainable.
Public Health Surveillance
Health informatics supports public health initiatives by monitoring the spread of diseases and identifying potential outbreaks. Surveillance systems can help health agencies respond swiftly to emerging health threats.
Medical Research and Innovation
Health informatics aids medical research by facilitating access to vast pools of patient data. Researchers can analyze this data to discover new treatments, study disease trends, and develop innovative medical technologies.
Patient Engagement and Empowerment
Health informatics encourages patients to take an active role in their health. Patient portals allow individuals to access their own health records, communicate with healthcare providers, and make informed decisions about their care.
Interoperability and Data Sharing
Standardized data formats and interoperability among healthcare systems enable seamless sharing of patient information across different healthcare providers. This ensures continuity of care and prevents duplication of tests and procedures.
Healthcare Quality Improvement
Health informatics enables healthcare providers to assess and enhance the quality of care they deliver. By tracking outcomes, patient satisfaction, and compliance with best practices, providers can make data-driven improvements.
Cost Reduction and Resource Management
Health informatics helps healthcare institutions optimize resource allocation and reduce costs. By identifying inefficiencies and areas of improvement, healthcare organizations can direct their resources more effectively.
Conclusion
In an era where data is often referred to as the “new oil,” health informatics is the vehicle through which the healthcare industry taps into the vast potential of health-related information. It empowers healthcare professionals with tools and insights to provide more efficient, cost-effective, and patient-centric care. With the ability to save lives, reduce healthcare costs, and drive medical innovations, health informatics is more than a trend; it is the future of healthcare. Its importance continues to grow as technology evolves and as the healthcare industry strives to provide the best possible care to patients around the world.
Pillars of Excellence: Key Standards in the Healthcare Industry
Introduction
The healthcare industry is marked by its unwavering commitment to patient care, safety, and the pursuit of excellence. To maintain the highest standards in patient treatment, healthcare professionals adhere to a set of well-defined guidelines and standards. In this article, we explore the key standards in the healthcare industry that serve as the foundation for quality care and patient safety.
HIPAA (Health Insurance Portability and Accountability Act)
HIPAA, which we discussed in a previous article, is a cornerstone of healthcare standards. Its Privacy and Security Rules ensure the confidentiality, integrity, and availability of protected health information. HIPAA also facilitates secure electronic data exchange, safeguarding patient privacy.
Patient-Centered Care
Patient-centered care focuses on the individual’s needs, preferences, and values. It encourages active patient involvement in healthcare decisions, considering their physical and emotional well-being. Effective communication and shared decision-making are key components of this standard.
Clinical Practice Guidelines
Clinical practice guidelines are evidence-based recommendations for healthcare professionals to provide high-quality care for specific medical conditions. These guidelines are continually updated to reflect the latest research, ensuring that patients receive the best possible care.
Infection Control
Infection control standards are crucial for maintaining patient safety. Healthcare facilities strictly adhere to practices designed to prevent the spread of infections. Hand hygiene, sterilization, and sanitation procedures are key components of infection control.
Accreditation and Certification
Healthcare institutions often seek accreditation and certification from organizations like The Joint Commission, which set high standards for patient care and safety. Compliance with these standards demonstrates an organization’s commitment to quality healthcare delivery.
EHR (Electronic Health Record) Standards
With the transition to electronic health records, interoperability and data standards are essential. These standards ensure that patient information can be accurately and securely exchanged between healthcare systems, promoting continuity of care.
Patient Safety Goals
Organizations like the World Health Organization (WHO) establish patient safety goals that healthcare providers worldwide must strive to meet. These goals include improving medication safety, reducing healthcare-associated infections, and preventing patient falls.
Nursing Standards
Nursing practice is guided by standards set by organizations like the American Nurses Association (ANA). These standards define the responsibilities and expectations for nursing practice, ensuring the delivery of safe and effective care.
Mental Health Standards
Mental health standards ensure that patients with mental health conditions receive appropriate and compassionate care. These standards include the provision of crisis intervention and psychosocial support.
Ethical Standards
Ethical standards in healthcare encompass a wide range of principles, including patient confidentiality, informed consent, and truth-telling. These standards guide the behavior and decision-making of healthcare professionals, ensuring the highest ethical standards in patient care.
Conclusion
The healthcare industry’s commitment to excellence and patient well-being is evident in the multitude of standards and guidelines that govern its practice. These standards touch on various aspects of healthcare, from privacy and data security to patient safety and ethical conduct. Adherence to these standards is not just a requirement but a reflection of the industry’s dedication to providing the best possible care to patients, ensuring their safety, and upholding the highest standards of professionalism and ethics. In the ever-evolving landscape of healthcare, these standards remain the pillars of excellence that drive the industry forward.
Revolutionizing Patient Forms: Warp Core Health’s AI-Generated Smart Forms
By Stephen Fitzmeyer, MD
Introduction: The repetitive nature of filling out the same forms during each visit to a healthcare provider can be a time-consuming and tedious process for patients. However, Warp Core Health, an innovative healthcare technology company, is leading the charge in transforming the patient form experience. Through their groundbreaking AI-powered solutions, Warp Core Health is developing an AI-generated form that patients fill out once, and subsequently, only relevant information is presented for review and update based on the reason for the visit. This revolution in patient forms aims to streamline the healthcare experience, save time, and improve the overall efficiency of medical visits.
- The Current Challenge: Traditionally, patients are required to provide a comprehensive range of information during each visit, regardless of the reason for their appointment. This results in repetitive and time-consuming form filling, often causing frustration for patients who feel that the process is unnecessary and inefficient. Furthermore, healthcare providers must sift through extensive paperwork to locate the specific details relevant to the visit, creating an additional administrative burden.
- AI-Generated Smart Forms: Warp Core Health’s AI-generated smart forms represent a significant advancement in the patient form process. With the power of artificial intelligence, these forms are designed to be dynamic and tailored to each patient’s specific needs. By leveraging machine learning algorithms, the smart forms intelligently analyze the reason for the visit and present only the relevant sections and questions for review and update.
- Personalized and Streamlined Experience: By eliminating the need to repeat previously provided information, patients can experience a more streamlined and personalized visit. With AI-generated smart forms, patients can focus on updating crucial details related to their current health condition, symptoms, or concerns. This targeted approach ensures that patients’ valuable time is maximized during their appointments, enabling healthcare providers to focus on delivering the most appropriate care.
- Enhanced Accuracy and Efficiency: Warp Core Health’s AI algorithms continually learn from patient data, allowing for improved accuracy and efficiency over time. As patients update their information during subsequent visits, the smart forms intelligently adapt and present new questions or prompts based on previous responses and the reason for the current visit. This iterative process ensures that patient information remains up-to-date and relevant, while minimizing redundant or unnecessary data entry.
- Integration with Electronic Health Records (EHR): Warp Core Health’s AI-generated smart forms seamlessly integrate with existing electronic health record (EHR) systems, creating a powerful synergy between patient information and form customization. As new data is added to the EHR, such as diagnoses, treatments, or test results, it further enhances the customization of smart forms for future visits. The AI algorithms analyze the updated EHR data and dynamically adjust the smart forms to ensure that patients are presented with the most relevant sections and questions specific to their follow-up or next visit. This dynamic customization optimizes the patient form experience, allowing for efficient updates and reviews of pertinent information while eliminating the need to navigate through irrelevant sections. By harnessing the power of EHR integration, Warp Core Health’s smart forms adapt to each patient’s evolving healthcare journey, ensuring a personalized and tailored experience throughout their medical visits.
- Data Security and Privacy: Warp Core Health places a high priority on maintaining the security and privacy of patient data. Their AI-generated smart forms are designed to adhere to stringent data protection regulations, ensuring that sensitive information remains confidential. Robust encryption, access controls, and compliance with industry standards are implemented to safeguard patient privacy throughout the form-filling and data storage processes.
Conclusion: Warp Core Health’s pioneering efforts in developing AI-generated smart forms are set to revolutionize the patient form experience in healthcare. By leveraging artificial intelligence, these forms minimize repetitive data entry, present only relevant information for review and update, and enhance the accuracy and efficiency of medical visits. With seamless integration into electronic health record systems, Warp Core Health ensures that patient information remains up-to-date, contributing to improved continuity of care. As the healthcare industry embraces the power of AI technology, Warp Core Health’s innovative approach to patient forms promises to transform the patient experience, saving time, and improving the overall efficiency of healthcare delivery.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Author: Sharon Lojun, M.D., M.S.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Understanding the Distinctions: Biomedical Informatics, Clinical Informatics, and Health Informatics
By Stephen Fitzmeyer, MD
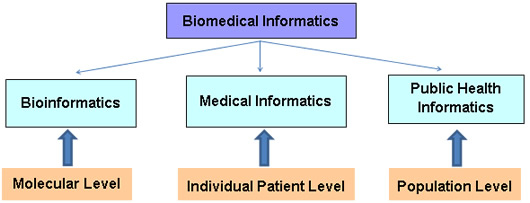
In today’s digital age, the field of informatics plays a crucial role in transforming healthcare by harnessing the power of technology and data. Within this expansive field, three distinct disciplines often come into play: biomedical informatics, clinical informatics, and health informatics. While these terms may seem interchangeable at first glance, they each encompass unique areas of focus and expertise. Let’s delve into the differences between these three disciplines to gain a clearer understanding.
Biomedical Informatics:
Biomedical informatics, sometimes referred to as bioinformatics, revolves around the intersection of biology, medicine, and computational sciences. It focuses on leveraging technology, data analysis, and information systems to advance biomedical research, discovery, and understanding. Biomedical informatics professionals work on developing tools and methodologies to store, manage, analyze, and interpret vast amounts of biological and clinical data.
The scope of biomedical informatics spans genomics, proteomics, imaging data, clinical trials, and more. By employing computational and analytical approaches, experts in this field can identify patterns, discover new insights, and enhance our understanding of complex biological processes. Biomedical informatics plays a vital role in areas such as personalized medicine, drug discovery, and precision healthcare.
Clinical Informatics:
Clinical informatics centers on the effective use of information and communication technologies in healthcare settings, with a primary focus on improving patient care and outcomes. It encompasses the application of informatics principles and methods to facilitate clinical decision-making, enhance workflow efficiencies, and optimize healthcare delivery.
Clinical informatics professionals bridge the gap between healthcare providers and technology. They ensure the successful implementation and utilization of electronic health records (EHRs), clinical decision support systems, computerized physician order entry (CPOE), and other healthcare information systems. They work to streamline data capture, facilitate interoperability between systems, and promote data-driven approaches to patient care.
Health Informatics:
Health informatics takes a broader perspective, encompassing both biomedical and clinical informatics while extending its reach to population health, public health, and healthcare management. Health informatics focuses on the collection, management, and analysis of health-related data to improve healthcare delivery, policy-making, and population health outcomes.
Professionals in health informatics leverage technology and information systems to monitor and assess population health trends, support public health initiatives, and facilitate data-driven decision-making. They play a crucial role in developing and implementing health information exchanges, health analytics, telemedicine, and health data standards to ensure seamless data exchange and enhance healthcare delivery on a larger scale.
In essence, while biomedical informatics concentrates on advancing scientific research through data analysis, clinical informatics focuses on optimizing clinical workflows and patient care delivery. Health informatics takes a broader perspective, incorporating both biomedical and clinical informatics while extending its scope to population health and healthcare management.
By understanding the distinctions between biomedical informatics, clinical informatics, and health informatics, we gain a deeper appreciation for the specialized roles each discipline plays in shaping the future of healthcare. Together, they contribute to the advancement of medical knowledge, optimization of clinical processes, and improvement of overall healthcare outcomes for individuals and populations alike.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/