- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Category: Biomedical Informatics
Unveiling the Mysteries of Epidemiology: The Backbone of Medicine
Introduction
In the vast realm of medicine, epidemiology stands as an unsung hero – the silent sentinel that plays a pivotal role in preventing, controlling, and understanding diseases. While this field may not garner the same attention as groundbreaking medical discoveries, it is the backbone that supports the entire healthcare system. In this article, we delve into the fascinating world of epidemiology, shedding light on what it is, why it matters, and how it shapes the practice of medicine.
What is Epidemiology?
Epidemiology is often described as the science of public health. It is the study of how diseases spread and impact populations, and it seeks to understand the patterns, causes, and consequences of health and disease in human communities. This field employs a variety of research methods to investigate the distribution and determinants of health-related outcomes, with the ultimate goal of improving public health.
Why Does Epidemiology Matter in Medicine?
Disease Prevention and Control:
Epidemiology plays a pivotal role in preventing and controlling diseases. By identifying risk factors, understanding the transmission of diseases, and evaluating interventions, epidemiologists help develop strategies to mitigate the impact of illnesses.
Public Health Policy:
Policymakers rely on epidemiological data to make informed decisions. This information helps shape public health policies, such as vaccination programs, smoking bans, and disaster preparedness, to protect and improve public health.
Outbreak Investigations:
During disease outbreaks, epidemiologists are the first responders. They conduct field investigations to identify the source of the outbreak, understand its transmission, and implement measures to contain it.
Research and Innovation:
Epidemiological studies provide the foundation for medical research. They generate hypotheses, drive clinical trials, and lead to the development of new treatments and therapies.
Key Concepts in Epidemiology
Incidence and Prevalence:
Incidence measures the rate of new cases of a disease within a specific time frame and population. Prevalence, on the other hand, reflects the total number of cases within a population at a given time. These metrics are essential for understanding the burden of diseases.
Risk Factors:
Identifying risk factors, such as genetics, lifestyle choices, and environmental exposures, is crucial in preventing diseases. Epidemiologists help pinpoint these factors, allowing for targeted interventions.
Cohort Studies and Case-Control Studies:
Cohort studies follow a group of individuals over time to assess the development of diseases, while case-control studies compare those with a specific condition to those without it. Both study designs help unravel the causes of diseases.
Outbreak Investigations:
During outbreaks, epidemiologists work swiftly to trace the origins of the disease, identify its transmission patterns, and implement control measures to limit its spread.
Surveillance Systems:
Epidemiologists use surveillance systems to monitor diseases on an ongoing basis. These systems enable early detection of outbreaks, providing a chance for swift intervention.
Challenges in Epidemiology
Epidemiology is not without its challenges. The field faces obstacles such as the difficulty of establishing causation, the ethical concerns surrounding experiments on human populations, and the evolving nature of diseases. With the rise of emerging infectious diseases and the increasing globalization of health threats, epidemiologists must adapt to new challenges continuously.
Conclusion
Epidemiology is the silent force that ensures the well-being of societies by enabling the prevention and control of diseases. In the practice of medicine, this field provides the essential knowledge and tools to understand the spread of illnesses, identify risk factors, and develop effective strategies for disease prevention and treatment. As medicine and healthcare evolve, epidemiology will remain a steadfast ally, contributing to the health and longevity of humanity. It is the unsung hero that keeps us safe, vigilant, and prepared for the health challenges of the future.
Unveiling the Role of ApoB and the Therapeutic Potential of Ketogenic Lifestyle and Intermittent Fasting in Atherosclerosis
By Stephen Fitzmeyer, MD
Introduction:
Atherosclerosis, a major contributor to cardiovascular disease, arises from a complex interplay of various factors. Among them, Apolipoprotein B (ApoB) emerges as the primary driver in the development and progression of this condition. In this article, we delve into the critical role of ApoB in atherosclerosis and shed light on the influence of inflammation in enhancing its effects.
Understanding the Role of ApoB:
ApoB, a protein found in lipoproteins such as low-density lipoprotein (LDL) particles, serves as a key player in atherosclerosis. It acts as a carrier, facilitating the transportation of cholesterol to peripheral tissues, including the arterial walls. In the absence of ApoB, the initiation and progression of atherosclerosis are virtually non-existent.
The Significance of ApoB in Atherosclerosis:
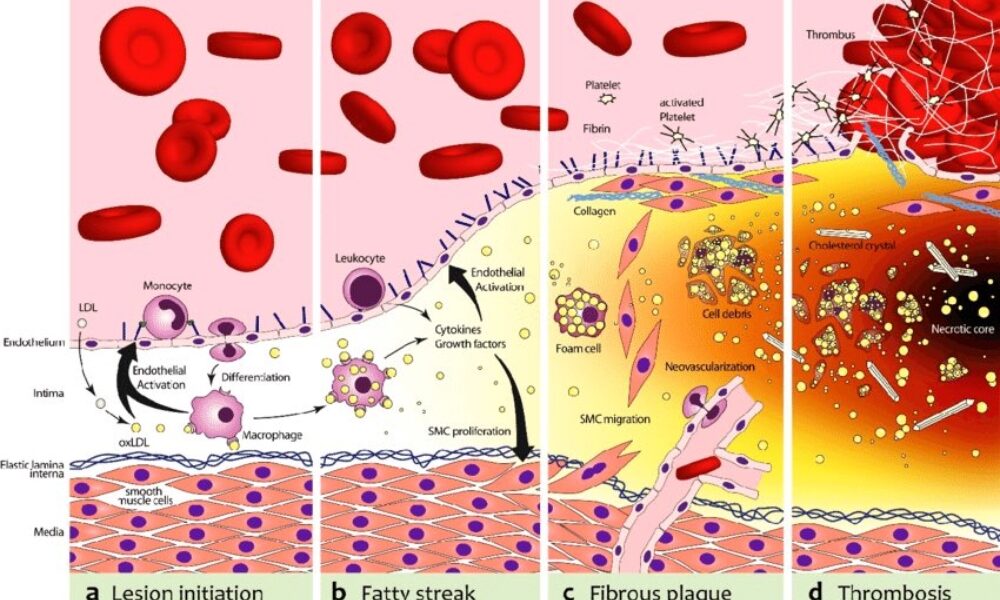
ApoB takes center stage in atherosclerosis, as it is responsible for delivering cholesterol-rich lipoproteins, particularly LDL, to arterial walls. These lipoproteins undergo modifications and become trapped in the arterial intima, initiating the formation of fatty streaks. With time, inflammation is triggered, attracting immune cells and accelerating the transformation of fatty streaks into advanced atherosclerotic plaques.
Inflammation and its Role:
While inflammation is a key player in atherosclerosis, it acts as an enhancer rather than the primary driver. Inflammation exacerbates the process by promoting the retention and modification of ApoB-containing lipoproteins, leading to plaque progression and instability. Thus, controlling inflammation becomes crucial in managing atherosclerosis, but addressing the root cause—ApoB—remains essential.
Implications and Therapeutic Strategies:
Understanding the central role of ApoB opens up avenues for therapeutic interventions in managing atherosclerosis. Addressing ApoB levels and reducing the burden of cholesterol-rich lipoproteins is key. Here, lifestyle modifications such as adopting a low-carbohydrate, high-fat diet (such as a ketogenic diet) and implementing intermittent fasting can prove beneficial. These approaches help regulate ApoB-containing lipoproteins, mitigate their retention in arterial walls, and slow down the progression of atherosclerosis.
Furthermore, lifestyle modifications that target additional risk factors associated with atherosclerosis, such as hypertension and obesity, should be considered. Engaging in regular physical activity, maintaining a healthy weight, and managing other comorbidities can complement the efforts to address ApoB and reduce the overall risk of atherosclerosis.
Conclusion:
ApoB stands as the primary driver in the initiation and progression of atherosclerosis, while inflammation serves to enhance and accelerate the process. Recognizing the pivotal role of ApoB provides insights into therapeutic strategies that can mitigate its effects. By adopting lifestyle modifications, such as a low-carbohydrate, high-fat diet and intermittent fasting, individuals can positively influence ApoB levels and manage atherosclerosis. Combining these interventions with measures to address other risk factors offers a comprehensive approach to reducing the burden of atherosclerosis and promoting cardiovascular health.
The biochemical pathway of plaque formation involving ApoB can be described as follows:
- ApoB synthesis: ApoB is a protein synthesized in the liver and intestines. It is a major component of very low-density lipoprotein (VLDL) and LDL particles.
- Lipoprotein assembly: VLDL particles are assembled in the liver and contain ApoB-100. They transport triglycerides and cholesterol from the liver to peripheral tissues. During circulation, VLDL particles undergo enzymatic changes, resulting in the conversion of triglycerides into free fatty acids and glycerol.
- LDL formation: As VLDL particles lose triglycerides, they become smaller and denser, transforming into LDL particles. LDL contains a single molecule of ApoB-100 and is the primary carrier of cholesterol in the bloodstream.
- LDL uptake: LDL particles bind to LDL receptors on cell surfaces, allowing the cells to take up cholesterol. These receptors are present in various tissues, including the arterial walls.
- Retention and modification: In the arterial walls, LDL particles can undergo modifications, such as oxidation and glycation, making them more prone to retention. These modified LDL particles interact with extracellular matrix proteins and proteoglycans in the arterial intima, leading to their entrapment within the vessel walls.
- Inflammation and foam cell formation: The retained LDL particles, along with their cholesterol content, trigger an inflammatory response. Immune cells, particularly macrophages, migrate to the site of inflammation. They engulf the cholesterol-rich LDL particles, transforming into foam cells, which are characterized by their lipid-filled cytoplasm.
- Fatty streak formation: The accumulation of foam cells and other immune cells results in the formation of fatty streaks, which are the initial visible signs of plaque development. Fatty streaks consist of foam cells, lipids, inflammatory cells, and smooth muscle cells.
- Advanced plaque formation: Over time, the fatty streaks can progress into more advanced atherosclerotic plaques. These plaques are characterized by a fibrous cap composed of smooth muscle cells and collagen, a lipid-rich core containing foam cells and cholesterol, and a necrotic center.
Throughout this biochemical pathway, ApoB plays a crucial role in the transport of cholesterol to peripheral tissues, including the arterial walls. It facilitates the delivery of cholesterol-rich LDL particles, which, under certain conditions, contribute to the formation of atherosclerotic plaques. Understanding this pathway provides valuable insights into potential therapeutic targets for preventing and managing plaque formation and related cardiovascular diseases.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unlocking the Power of Health Informatics: Why It Matters
Introduction
Health informatics is a rapidly growing field that combines healthcare, information technology, and data science to transform the way we manage and utilize health-related information. In the digital age, health informatics plays a pivotal role in enhancing patient care, improving healthcare processes, and driving medical research. In this article, we delve into the importance of health informatics and the manifold ways in which it positively impacts the healthcare industry.
Enhanced Patient Care
Health informatics improves patient care by providing healthcare professionals with instant access to accurate and up-to-date patient information. Electronic Health Records (EHRs) store patient histories, test results, medications, and treatment plans, reducing the risk of medical errors and ensuring that the right treatment is delivered to the right patient.
Efficient Healthcare Processes
Health informatics streamlines administrative and clinical processes in healthcare. It reduces paperwork, automates scheduling and billing, and facilitates communication among healthcare providers. This efficiency not only saves time but also reduces costs, making healthcare more accessible.
Data-Driven Decision-Making
Health informatics leverages data analysis to inform healthcare decisions. By analyzing trends and patterns, healthcare providers can make more informed choices about patient care and resource allocation, ultimately improving patient outcomes.
Telemedicine and Remote Monitoring
The integration of health informatics in telemedicine enables remote consultations and monitoring of patients. This is particularly crucial in reaching patients in underserved or remote areas, providing access to quality healthcare that might otherwise be unattainable.
Public Health Surveillance
Health informatics supports public health initiatives by monitoring the spread of diseases and identifying potential outbreaks. Surveillance systems can help health agencies respond swiftly to emerging health threats.
Medical Research and Innovation
Health informatics aids medical research by facilitating access to vast pools of patient data. Researchers can analyze this data to discover new treatments, study disease trends, and develop innovative medical technologies.
Patient Engagement and Empowerment
Health informatics encourages patients to take an active role in their health. Patient portals allow individuals to access their own health records, communicate with healthcare providers, and make informed decisions about their care.
Interoperability and Data Sharing
Standardized data formats and interoperability among healthcare systems enable seamless sharing of patient information across different healthcare providers. This ensures continuity of care and prevents duplication of tests and procedures.
Healthcare Quality Improvement
Health informatics enables healthcare providers to assess and enhance the quality of care they deliver. By tracking outcomes, patient satisfaction, and compliance with best practices, providers can make data-driven improvements.
Cost Reduction and Resource Management
Health informatics helps healthcare institutions optimize resource allocation and reduce costs. By identifying inefficiencies and areas of improvement, healthcare organizations can direct their resources more effectively.
Conclusion
In an era where data is often referred to as the “new oil,” health informatics is the vehicle through which the healthcare industry taps into the vast potential of health-related information. It empowers healthcare professionals with tools and insights to provide more efficient, cost-effective, and patient-centric care. With the ability to save lives, reduce healthcare costs, and drive medical innovations, health informatics is more than a trend; it is the future of healthcare. Its importance continues to grow as technology evolves and as the healthcare industry strives to provide the best possible care to patients around the world.
Understanding the Distinctions: Biomedical Informatics, Clinical Informatics, and Health Informatics
By Stephen Fitzmeyer, MD
In today’s digital age, the field of informatics plays a crucial role in transforming healthcare by harnessing the power of technology and data. Within this expansive field, three distinct disciplines often come into play: biomedical informatics, clinical informatics, and health informatics. While these terms may seem interchangeable at first glance, they each encompass unique areas of focus and expertise. Let’s delve into the differences between these three disciplines to gain a clearer understanding.
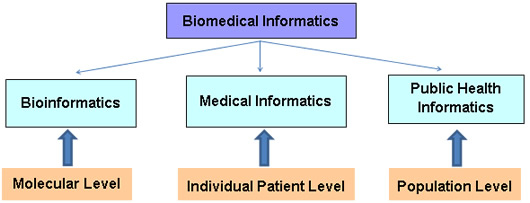
Biomedical Informatics:
Biomedical informatics, sometimes referred to as bioinformatics, revolves around the intersection of biology, medicine, and computational sciences. It focuses on leveraging technology, data analysis, and information systems to advance biomedical research, discovery, and understanding. Biomedical informatics professionals work on developing tools and methodologies to store, manage, analyze, and interpret vast amounts of biological and clinical data.
The scope of biomedical informatics spans genomics, proteomics, imaging data, clinical trials, and more. By employing computational and analytical approaches, experts in this field can identify patterns, discover new insights, and enhance our understanding of complex biological processes. Biomedical informatics plays a vital role in areas such as personalized medicine, drug discovery, and precision healthcare.
Clinical Informatics:
Clinical informatics centers on the effective use of information and communication technologies in healthcare settings, with a primary focus on improving patient care and outcomes. It encompasses the application of informatics principles and methods to facilitate clinical decision-making, enhance workflow efficiencies, and optimize healthcare delivery.
Clinical informatics professionals bridge the gap between healthcare providers and technology. They ensure the successful implementation and utilization of electronic health records (EHRs), clinical decision support systems, computerized physician order entry (CPOE), and other healthcare information systems. They work to streamline data capture, facilitate interoperability between systems, and promote data-driven approaches to patient care.
Health Informatics:
Health informatics takes a broader perspective, encompassing both biomedical and clinical informatics while extending its reach to population health, public health, and healthcare management. Health informatics focuses on the collection, management, and analysis of health-related data to improve healthcare delivery, policy-making, and population health outcomes.
Professionals in health informatics leverage technology and information systems to monitor and assess population health trends, support public health initiatives, and facilitate data-driven decision-making. They play a crucial role in developing and implementing health information exchanges, health analytics, telemedicine, and health data standards to ensure seamless data exchange and enhance healthcare delivery on a larger scale.
In essence, while biomedical informatics concentrates on advancing scientific research through data analysis, clinical informatics focuses on optimizing clinical workflows and patient care delivery. Health informatics takes a broader perspective, incorporating both biomedical and clinical informatics while extending its scope to population health and healthcare management.
By understanding the distinctions between biomedical informatics, clinical informatics, and health informatics, we gain a deeper appreciation for the specialized roles each discipline plays in shaping the future of healthcare. Together, they contribute to the advancement of medical knowledge, optimization of clinical processes, and improvement of overall healthcare outcomes for individuals and populations alike.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/