- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Author: Stephen Fitzmeyer, MD
M.D. with two postdocs in Clinical Informatics, one as the Ruth L. Kirschstein NIH NRSA Informatics Fellows at Boston Medical Center and the other as an Advanced Medical Informatics Fellow at the Boston VA Healthcare system. Dr. Fitzmeyer is the founder of Warp Core Health and Jax Code Academy.
Harnessing the Power of Nutritional Neurology: A Ketogenic Lifestyle and Intermittent Fasting Approach
By Stephen Fitzmeyer, MD
Introduction:
In recent years, the field of nutritional neurology has gained significant attention as a promising approach to enhance brain health and treat various neurological disorders. By combining the principles of a ketogenic lifestyle and intermittent fasting, researchers and healthcare professionals are exploring new avenues for improving and potentially even curing certain neurological conditions. This article aims to shed light on the concept of nutritional neurology and its potential impact on ten neurological disorders.
Understanding Nutritional Neurology:
Nutritional neurology focuses on the relationship between diet and brain health. It recognizes that the food we consume can directly impact the structure and function of our nervous system. A ketogenic lifestyle involves consuming a high-fat, low-carbohydrate diet that induces a state of ketosis. Intermittent fasting, on the other hand, refers to periods of time when food intake is restricted, alternating with periods of regular eating.
Neurological Disorders and the Role of Nutritional Neurology:
Epilepsy: Studies have shown that a ketogenic diet can significantly reduce seizure frequency in individuals with epilepsy, particularly in children whose seizures are drug-resistant.
Alzheimer’s Disease: A ketogenic diet and intermittent fasting have shown potential in enhancing brain function and reducing cognitive decline in individuals with Alzheimer’s disease.
Parkinson’s Disease: Nutritional neurology, particularly the ketogenic diet, may help improve motor symptoms and overall quality of life in individuals with Parkinson’s disease.
Multiple Sclerosis (MS): Some evidence suggests that a ketogenic diet may alleviate symptoms and slow down the progression of MS by reducing inflammation and oxidative stress.
Migraine: The ketogenic diet, combined with intermittent fasting, may reduce the frequency and intensity of migraines by modulating brain energy metabolism and reducing neuroinflammation.
Autism Spectrum Disorders (ASD): Nutritional interventions, including a ketogenic diet and intermittent fasting, have shown promise in managing symptoms associated with ASD, such as behavioral issues and cognitive impairments.
Depression: Emerging research suggests that a ketogenic diet and intermittent fasting may have antidepressant effects by modulating neurotransmitter activity and reducing inflammation.
Traumatic Brain Injury (TBI): Nutritional neurology approaches, such as a ketogenic diet and intermittent fasting, have shown potential in promoting neuroprotection and supporting recovery following TBI.
Amyotrophic Lateral Sclerosis (ALS): While further research is needed, preliminary studies indicate that a ketogenic diet may improve mitochondrial function and potentially slow the progression of ALS.
Attention Deficit Hyperactivity Disorder (ADHD): Nutritional interventions, including a ketogenic diet and intermittent fasting, may help manage symptoms of ADHD by improving focus, attention, and behavior.
Conclusion:
Nutritional neurology offers a fascinating perspective on brain health and the treatment of neurological disorders. By embracing a ketogenic lifestyle and incorporating intermittent fasting, individuals may potentially experience improvements in various neurological conditions. However, it is important to note that nutritional interventions should be pursued under the guidance of healthcare professionals and tailored to each individual’s specific needs. As research continues to unfold, nutritional neurology holds the promise of transforming the way we approach neurological disorders and enhancing the lives of countless individuals.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Leveraging Fiber for Blood Sugar Control in a Ketogenic Diet: A Guide for Type 1 and Type 2 Diabetics
By Stephen Fitzmeyer, MD
For individuals living with Type 1 or Type 2 diabetes, maintaining stable blood sugar levels is of utmost importance. While a ketogenic diet can be a beneficial approach for managing diabetes, it requires careful consideration of nutrient intake, including fiber. Incorporating fiber-rich foods into each meal can play a crucial role in controlling and stabilizing blood sugar levels. In this article, we will explore the scientific evidence supporting the use of fiber for blood sugar control in a ketogenic diet and provide practical recommendations for individuals with diabetes.
Introduction
For years, health-conscious individuals have been advised to consume fruit as part of a balanced diet due to its nutritional value and potential health benefits. However, recent studies have shed light on an important distinction between whole fruit and fruit juice regarding their effect on blood sugar levels. It turns out that the presence of fiber in whole fruit plays a significant role in slowing down the absorption of fructose, the natural sugar found in fruit. In contrast, fruit juice lacks the same fiber content, leading to a more rapid rise in blood sugar levels. Let’s delve deeper into the research and uncover the implications of these findings.
The Role of Fiber
Fiber is a key component of whole fruits that is absent in fruit juice. This dietary component consists of soluble and insoluble fibers, both of which contribute to a slower and more controlled release of sugars into the bloodstream. When consuming whole fruit, the fibrous structure acts as a physical barrier, reducing the speed at which sugars, including fructose, are absorbed. As a result, blood sugar levels rise more gradually, minimizing the risk of blood sugar spikes.
The Role of Fiber in Blood Sugar Control
Fiber-rich foods have a significant impact on blood sugar control. Fiber consists of indigestible carbohydrates that cannot be broken down by human enzymes. Instead, fiber passes through the digestive system relatively intact. There are two main types of fiber: soluble fiber and insoluble fiber. Both types contribute to blood sugar control in different ways.
Soluble fiber forms a gel-like substance in the digestive tract, slowing down the digestion and absorption of carbohydrates, including sugars. This results in a more gradual release of glucose into the bloodstream, preventing sudden spikes in blood sugar levels. Insoluble fiber, on the other hand, adds bulk to the stool, promoting regular bowel movements and preventing constipation, a common issue for individuals with diabetes.
Scientific Studies on Fiber and Blood Sugar Control
Numerous studies have investigated the effects of fiber on blood sugar control, including its impact on postprandial glucose levels (blood sugar levels after a meal) and glycemic control over the long term.
A study published in the journal “Diabetes Care” examined the effects of a high-fiber diet on glycemic control in individuals with Type 2 diabetes. The researchers found that participants who consumed a diet rich in fiber experienced significant improvements in glycemic control, including reduced HbA1c levels (a marker of long-term blood sugar control) and lower postprandial glucose levels.
Another study published in the “Journal of Clinical Nutrition” compared the effects of two different breakfast meals on blood sugar control in individuals with Type 2 diabetes. One meal contained high-fiber foods such as oats and fruits, while the other meal contained low-fiber foods. The researchers found that the high-fiber breakfast led to significantly lower postprandial glucose levels and improved overall glycemic control compared to the low-fiber breakfast.
Slower Absorption and Glycemic Index
The glycemic index (GI) is a measure of how quickly a particular food raises blood sugar levels. Foods with a low GI are digested and absorbed more slowly, leading to a gradual increase in blood sugar levels. Several studies have compared the glycemic index of whole fruit and fruit juice, consistently finding that whole fruit has a lower GI than its juice counterpart.
One study published in the journal “Diabetes Care” compared the effects of consuming whole apples versus apple juice in a group of participants. The researchers found that whole apples had a lower glycemic response, resulting in a more gradual increase in blood sugar levels, compared to apple juice. These findings highlight the role of fiber in moderating the absorption of fructose and its impact on blood sugar.
Long-Term Health Implications
The differential effect of whole fruit and fruit juice on blood sugar levels has significant implications for long-term health. Rapid spikes in blood sugar can strain the body’s ability to produce enough insulin to regulate glucose levels effectively. Over time, this may lead to insulin resistance, an underlying factor in the development of type 2 diabetes.
Furthermore, the consumption of whole fruits provides additional health benefits beyond blood sugar regulation. Fruits are rich in vitamins, minerals, antioxidants, and other phytochemicals that contribute to overall well-being and the prevention of chronic diseases such as heart disease and certain cancers. By choosing whole fruits over fruit juice, individuals can harness the combined benefits of fiber and essential nutrients.
The Importance of Including Fiber in Every Meal
For individuals with diabetes following a ketogenic diet, it is crucial to include a source of fiber in every meal. Here are some reasons why:
Blood Sugar Regulation: Including fiber in each meal helps regulate blood sugar levels by slowing down the absorption of glucose. This can minimize the risk of blood sugar spikes and promote better overall glucose control.
Satiety and Weight Management: Fiber-rich foods are generally more filling and can contribute to a sense of satiety after a meal. This can aid in appetite management and weight control, which is particularly important for individuals with diabetes. Maintaining a healthy weight helps improve insulin sensitivity and supports blood sugar management.
Digestive Health: Fiber plays a vital role in maintaining a healthy digestive system. It adds bulk to the stool, promotes regular bowel movements, and helps prevent gastrointestinal issues such as constipation. This is particularly relevant for individuals with diabetes, as they are more prone to digestive complications.
How can you supplement fiber in your ketogenic diet without grains or carbs?
If you’re looking to supplement fiber in your diet without relying on grains or carbs, there are several options you can consider. Here are some fiber-rich foods that are low in grains and carbohydrates:
- Vegetables: Non-starchy vegetables like broccoli, cauliflower, Brussels sprouts, kale, spinach, and asparagus are excellent sources of fiber. You can include these in your meals and snacks.
- Berries: Berries such as raspberries, blackberries, and strawberries are relatively low in carbs and high in fiber. They can be consumed fresh or frozen and added to yogurt or smoothies.
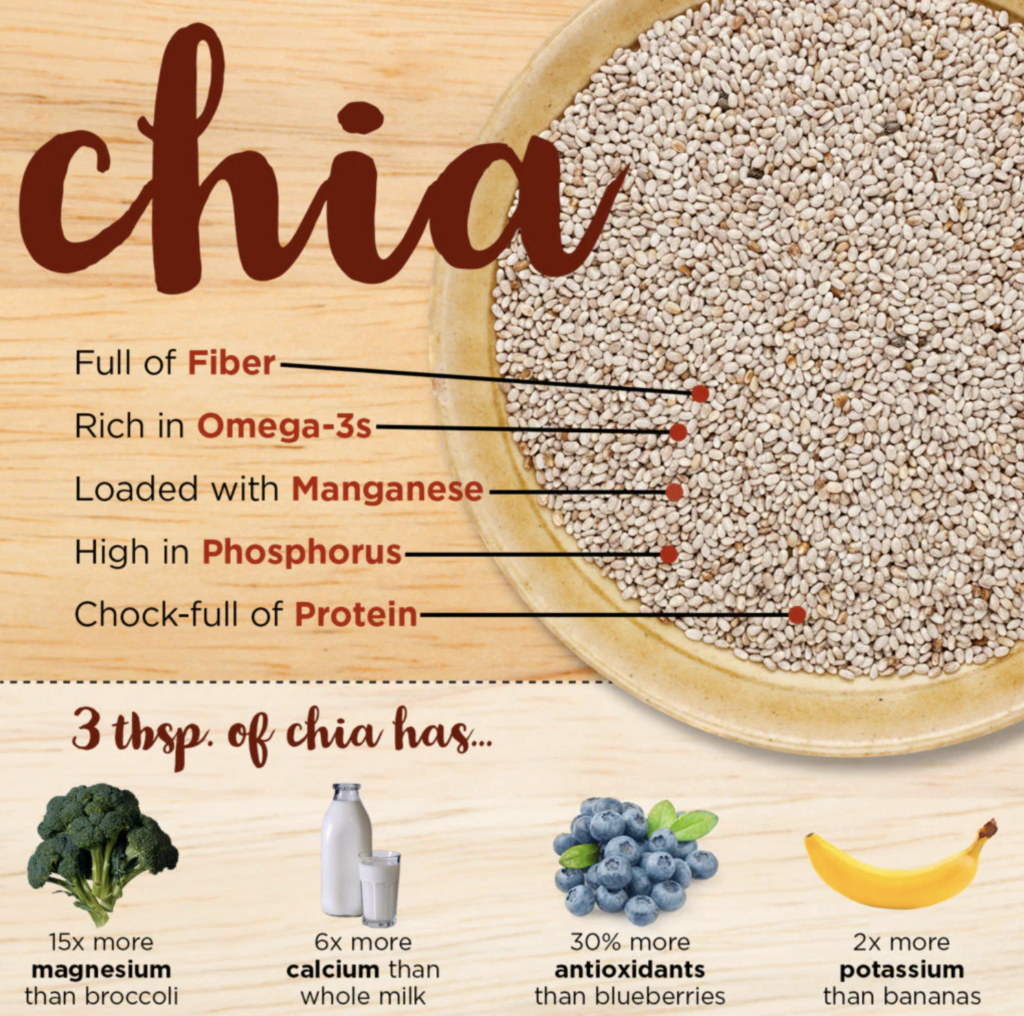
- Chia seeds: Chia seeds are packed with fiber and can be easily incorporated into your diet. They can be added to smoothies, yogurt, or used as a topping for salads or oatmeal.
- Flaxseeds: Flaxseeds are another great source of fiber. You can sprinkle ground flaxseeds on your meals, add them to smoothies, or use them in baking recipes.
- Avocado: Avocado is a nutrient-dense fruit that is high in healthy fats and fiber. You can enjoy avocado as a topping, in salads, or as a guacamole dip.
- Nuts and seeds: Almonds, walnuts, and sunflower seeds are examples of nuts and seeds that provide both fiber and healthy fats. They can be eaten as a snack or added to various dishes.
- Legumes: While legumes like beans and lentils contain carbohydrates, they are also excellent sources of fiber and protein. Including moderate amounts of legumes in your diet can be beneficial.
- Psyllium husk: Psyllium husk is a fiber supplement derived from the seeds of the Plantago ovata plant. It is low in carbs and can be mixed with water or added to recipes as a thickening agent.
- Coconut: Coconut is rich in fiber and healthy fats. You can incorporate shredded coconut into your meals, use coconut flour for baking, or enjoy coconut milk in smoothies or curries.
- Cabbage: Cabbage is a low-carb vegetable that provides a good amount of fiber. You can use it in salads, stir-fries, or even make cabbage wraps instead of grain-based wraps.
- Mushrooms: Mushrooms are low in carbs and contain fiber. They can be used in a variety of dishes, such as stir-fries, soups, or stuffed mushroom caps.
- Cauliflower rice: Cauliflower can be grated or processed into rice-like grains, providing a low-carb alternative to traditional grains. You can use cauliflower rice as a base for stir-fries, salads, or side dishes.
- Seaweed: Various types of seaweed, such as nori or kelp, are low in carbs and high in fiber. You can enjoy them in sushi rolls, salads, or as a crunchy snack.
- Artichokes: Artichokes are a good source of fiber and can be enjoyed steamed, grilled, or added to dips like spinach artichoke dip.
- Green leafy vegetables: Leafy greens like spinach, Swiss chard, and kale are low in carbs and rich in fiber. They can be used in salads, smoothies, or sautéed as a side dish.
Consulting a Healthcare Professional
It is crucial to consult with a healthcare professional or registered dietitian experienced in diabetes management before making any significant changes to your diet, especially if you have diabetes. They can provide personalized guidance based on your specific needs and help you create a well-balanced meal plan that incorporates fiber-rich foods while adhering to a ketogenic approach.
Conclusion
Incorporating fiber into a ketogenic diet is essential for individuals with Type 1 or Type 2 diabetes aiming to maintain stable blood sugar levels. Scientific studies have consistently demonstrated the positive impact of fiber on glycemic control and blood sugar management. By prioritizing fiber-rich foods such as non-starchy vegetables, berries, seeds, and nuts, individuals with diabetes can enhance their overall dietary fiber intake while adhering to a ketogenic eating pattern. By doing so, they can work towards better blood sugar control and improved long-term health outcomes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unraveling the Dawn Phenomenon: Understanding Gluconeogenesis in Type 1 Diabetes
By Stephen Fitzmeyer, MD
Introduction:
The dawn phenomenon is a well-known phenomenon observed in individuals with type 1 diabetes, characterized by an abnormal rise in blood glucose levels during the early morning hours, even in the absence of food intake. It has been a subject of scientific curiosity and investigation for many years. While the exact cause of the dawn phenomenon remains unclear, one hypothesis suggests that overactive gluconeogenesis may play a significant role in its manifestation. In this article, we delve into the relationship between the dawn phenomenon and gluconeogenesis in type 1 diabetes to shed light on this intriguing phenomenon.
Understanding the Dawn Phenomenon:
To comprehend the dawn phenomenon, it is essential to grasp the concept of gluconeogenesis. Gluconeogenesis is a natural process in which the liver produces glucose from non-carbohydrate sources, such as amino acids and glycerol. This metabolic pathway is crucial in maintaining blood glucose levels during periods of fasting or prolonged exercise.
In individuals with type 1 diabetes, who lack insulin production, the dawn phenomenon is believed to occur due to the combined effect of several factors. During the late night and early morning hours, hormones such as cortisol, growth hormone, and glucagon are released in higher amounts. These hormones work together to increase insulin resistance and stimulate hepatic gluconeogenesis. The elevated blood glucose levels observed in the morning are thought to be a consequence of these hormonal changes.
Role of Gluconeogenesis in the Dawn Phenomenon:
Gluconeogenesis is regulated by a complex interplay of hormonal and metabolic factors. Under normal circumstances, insulin suppresses gluconeogenesis, primarily by inhibiting the release of glucagon and promoting glucose uptake in peripheral tissues. However, in type 1 diabetes, the absence of insulin disrupts this balance, resulting in uncontrolled gluconeogenesis.
Research has suggested that the dawn phenomenon may be associated with overactive gluconeogenesis. Studies have shown increased levels of hepatic glucose production during the early morning hours in individuals with type 1 diabetes experiencing the dawn phenomenon. This excessive glucose production can contribute to the elevated blood glucose levels observed upon waking.
Alternative Factors:
While overactive gluconeogenesis is one plausible explanation for the dawn phenomenon, it is important to note that other factors may also contribute to its occurrence. The release of counterregulatory hormones, such as cortisol and growth hormone, may promote hepatic glucose output, leading to increased blood glucose levels. Additionally, alterations in circadian rhythms and overnight hypoglycemia followed by a rebound effect might also contribute to the dawn phenomenon.
Clinical Implications:
Understanding the mechanisms underlying the dawn phenomenon is crucial for effective diabetes management. Several strategies can help mitigate its impact. Adjusting insulin regimens, particularly by optimizing basal insulin doses during the early morning hours, can help counteract the excessive hepatic glucose production. Additionally, lifestyle modifications such as regular exercise, a balanced diet, and adequate sleep may aid in maintaining stable blood glucose levels.
Conclusion:
While the dawn phenomenon in individuals with type 1 diabetes remains a subject of ongoing research, overactive gluconeogenesis appears to be one of the contributing factors. The hormonal changes that occur during the early morning hours, coupled with the absence of insulin, disrupt the delicate balance of glucose regulation. Further research is needed to unravel the intricate mechanisms involved in the dawn phenomenon fully. By gaining a deeper understanding of this phenomenon, healthcare professionals can develop more effective strategies to manage blood glucose levels and improve the overall well-being of individuals living with type 1 diabetes.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
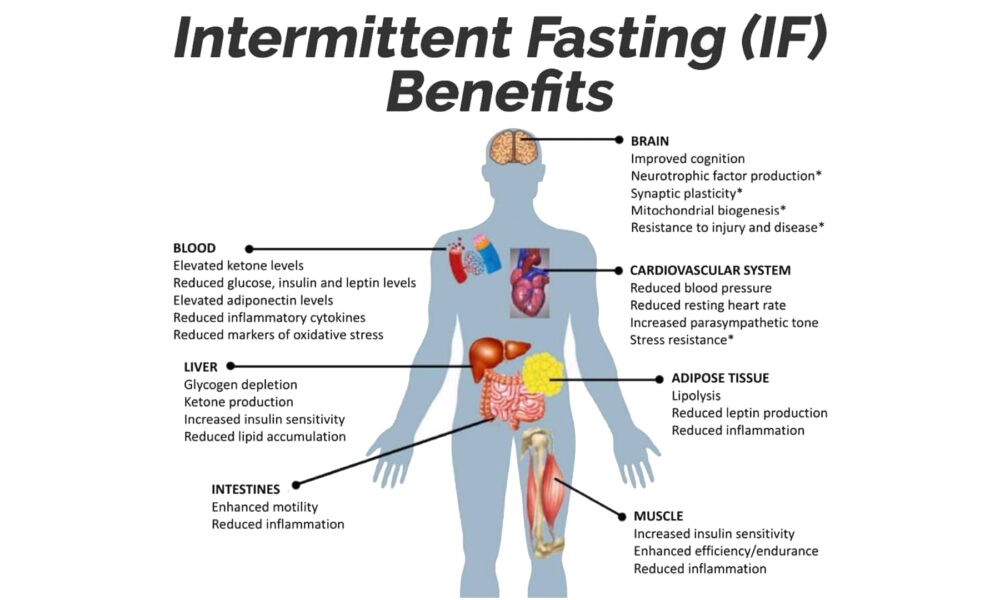
Intermittent Fasting: The Key to Metabolic Health, Empowered by the Ketogenic Diet for Satiety, Hunger Reduction, and Craving Control
By Stephen Fitzmeyer, MD
Introduction
In the realm of metabolic health, one strategy has risen above the rest: Intermittent Fasting (IF). When coupled with the Ketogenic (Keto) diet, IF becomes an unrivaled approach that unlocks the full potential of satiety, hunger reduction, and cravings control. By harnessing the power of fasting, IF paves the way for optimal metabolic function, while the Keto diet amplifies these benefits, leading to improved overall health and well-being.
Intermittent Fasting: A Metabolic Game Changer
Intermittent Fasting has garnered widespread acclaim due to its profound impact on metabolic health. Rather than focusing solely on what you eat, IF centers on when you eat, establishing periods of fasting interspersed with designated eating windows.
At the core of IF lies its ability to promote metabolic flexibility. By depriving your body of constant food intake, it becomes adept at tapping into stored fat as an alternative energy source. This metabolic switch leads to weight loss, increased insulin sensitivity, and reduced inflammation.
Satiety and Hunger Reduction: The Role of IF
One of the key advantages of IF is its capacity to enhance satiety and curb hunger. During fasting periods, your body turns to its fat stores for fuel, facilitating fat burning and weight loss. However, the benefits extend far beyond shedding pounds.
IF effectively regulates hunger and fullness hormones, such as ghrelin and leptin, which influence appetite. With consistent practice, these hormones rebalance, resulting in reduced hunger and decreased cravings. By allowing your body ample time between meals, IF equips you with a newfound sense of control over your eating habits.
The Power of the Ketogenic Diet
Enter the Ketogenic diet, a low-carbohydrate, high-fat approach that synergizes remarkably with IF. By drastically reducing carbohydrate intake and increasing healthy fat consumption, the Keto diet promotes nutritional ketosis—a metabolic state where your body primarily relies on fat for energy.
The Keto diet is a satiety powerhouse. Healthy fats take longer to digest, keeping you feeling full and satisfied for extended periods. This phenomenon effectively curbs hunger, reduces cravings, and prevents the energy crashes associated with high-carbohydrate diets.
IF and Keto: The Dynamic Duo for Metabolic Health
When Intermittent Fasting and the Ketogenic diet join forces, a metabolic transformation occurs. IF acts as the catalyst, priming your body for efficient fat burning, while the Keto diet ensures that fat becomes the primary fuel source.
By following a Ketogenic diet within your designated eating window, you not only maintain a state of ketosis but also heighten the feeling of satiety. The combined approach effectively reduces hunger and cravings, making it easier to adhere to your dietary goals and achieve optimal metabolic health.
Conclusion
Intermittent Fasting is the key to unlocking metabolic health, and when paired with the Ketogenic diet, it becomes an unbeatable strategy for satiety, hunger reduction, and craving control. IF enhances your body’s ability to tap into stored fat for energy and regulates hunger hormones, while the Keto diet amplifies these effects through increased fat consumption.
Embrace Intermittent Fasting as your metabolic ally and leverage the Ketogenic diet as the perfect complement. Together, they offer a path to sustainable weight loss, improved insulin sensitivity, and enhanced overall well-being. Experience the transformative power of IF and Keto, and embrace a life of metabolic vitality.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Harness the Power of Chia Seeds: Essential Fat Source for Vegans and Vegetarians on a Ketogenic Diet
By Stephen Fitzmeyer
Introduction: Following a ketogenic diet with intermittent fasting can present unique challenges for vegans and vegetarians. However, there is an incredibly versatile and nutrient-dense solution that can help bridge the fat gap in their diets—chia seeds. These tiny powerhouses are abundant in healthy fats, making them an indispensable addition for individuals seeking to maintain a balanced and nourishing meal plan. Let’s explore the vital role chia seeds play in providing essential fats for vegans and vegetarians on a ketogenic diet with intermittent fasting.
Rich in Healthy Fats: Chia seeds are a remarkable source of healthy fats, particularly omega-3 fatty acids. These essential fats are crucial for brain health, reducing inflammation, and supporting cardiovascular well-being. By incorporating chia seeds into their meals, vegans and vegetarians can ensure they are meeting their daily fat requirements, which are essential for overall health and vitality.
Promote Ketosis: In a ketogenic diet, the primary energy source shifts from carbohydrates to fats. Chia seeds, with their high fat content and low carbohydrate profile, contribute to achieving and maintaining a state of ketosis. Including chia seeds in a vegan or vegetarian ketogenic diet provides a reliable and convenient way to increase fat intake while minimizing carb consumption, aiding the body in transitioning to a fat-burning metabolic state.
Satiety and Appetite Control: One of the challenges of intermittent fasting is managing hunger and maintaining satiety during fasting periods. The combination of healthy fats and fiber in chia seeds helps promote a feeling of fullness, making them an effective tool for appetite control. The fats in chia seeds are digested slowly, providing sustained energy and reducing the likelihood of cravings or overeating. By incorporating chia seeds into meals or snacks, vegans and vegetarians can support their efforts in adhering to an intermittent fasting schedule.
Versatile and Easy to Include: Chia seeds offer immense versatility in meal preparation, making them an ideal addition to a vegan or vegetarian ketogenic diet. They can be added to smoothies, sprinkled on salads, used as a thickening agent in sauces, or incorporated into baked goods. Their ability to absorb liquids and form a gel-like consistency allows them to adapt to various culinary creations, enhancing both taste and texture.
Nutrient-Rich Profile: Beyond their healthy fat content, chia seeds boast an impressive nutrient profile. They are a notable source of plant-based protein, essential minerals such as calcium, phosphorus, magnesium, and manganese, and dietary fiber. This nutrient combination is especially valuable for vegans and vegetarians who may face challenges in meeting their daily requirements. By integrating chia seeds into their diet, individuals can enhance their overall nutritional intake and ensure they are obtaining a well-rounded range of essential nutrients.
Conclusion: For vegans and vegetarians on a ketogenic diet with intermittent fasting, chia seeds are a nutritional powerhouse that plays a vital role in meeting the necessary fat intake. With their high healthy fat content, chia seeds support ketosis, enhance satiety, and provide a wide array of essential nutrients. By incorporating chia seeds into their meals, vegans and vegetarians can effectively address the challenge of obtaining adequate fats while adhering to their dietary preferences and maintaining the principles of a ketogenic diet with intermittent fasting. Embrace the extraordinary potential of chia seeds and witness the transformative impact they can have on your vegan or vegetarian ketogenic journey.
—
Here are some keto-friendly examples of how to use chia seeds in your daily meals:
- Keto Chia Pudding:
- In a jar, combine 2 tablespoons of chia seeds, 1 cup of unsweetened almond milk (or any non-dairy milk with no added sugars), and a few drops of liquid stevia (or any keto-approved sweetener) to taste.
- Stir well and let it sit in the refrigerator overnight or for at least 4 hours.
- In the morning, give it a good stir and top with a sprinkle of low-carb berries (such as raspberries or blackberries), chopped nuts, or a dollop of coconut cream for added richness.
- Chia Seed Smoothie Booster:
- Add 1 tablespoon of chia seeds to your favorite keto-friendly smoothie recipe.
- Blend until smooth, and the chia seeds will provide added thickness and a boost of healthy fats to your smoothie.
- Keto Chia Seed Pudding Parfait:
- In a jar or glass, layer chia pudding (made with chia seeds, unsweetened almond milk, and keto-friendly sweetener) with a dollop of full-fat coconut yogurt or unsweetened Greek yogurt.
- Top with a sprinkle of crushed nuts, unsweetened coconut flakes, and a few low-carb berries.
- Repeat the layers and create a beautiful and satisfying chia seed pudding parfait.
- Keto Chia Seed Crackers:
- In a bowl, mix 1/4 cup of chia seeds, 1/4 cup of ground flaxseed, 2 tablespoons of coconut flour, 1/2 teaspoon of garlic powder, 1/2 teaspoon of onion powder, 1/4 teaspoon of sea salt, and 1/4 cup of water.
- Let the mixture sit for a few minutes to allow the chia seeds and flaxseed to absorb the water and form a gel-like consistency.
- Spread the mixture evenly on a parchment-lined baking sheet and bake at 350°F (175°C) for about 15-20 minutes, or until the crackers are golden and crispy.
- Allow them to cool before breaking them into crackers.
- Serve the keto chia seed crackers with your favorite low-carb dip or enjoy them on their own as a crunchy snack.
- Keto Chia Seed Breakfast Porridge:
- In a saucepan, combine 2 tablespoons of chia seeds, 2 tablespoons of unsweetened coconut flakes, 1/2 cup of unsweetened almond milk, 1/2 cup of water, and a pinch of cinnamon.
- Cook over medium heat, stirring occasionally, until the mixture thickens and reaches your desired porridge consistency.
- Remove from heat and let it cool for a few minutes.
- Top with sliced almonds, a drizzle of sugar-free syrup or melted coconut oil, and a sprinkle of ground flaxseed or hemp hearts for added crunch and healthy fats.
Remember to adjust the portion sizes and ingredients based on your specific dietary needs and goals on the keto diet. Enjoy these keto-friendly chia seed recipes and explore more possibilities to incorporate this nutritious superfood into your daily keto meal plan.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Unveiling the Role of ApoB and the Therapeutic Potential of Ketogenic Lifestyle and Intermittent Fasting in Atherosclerosis
By Stephen Fitzmeyer, MD
Introduction:
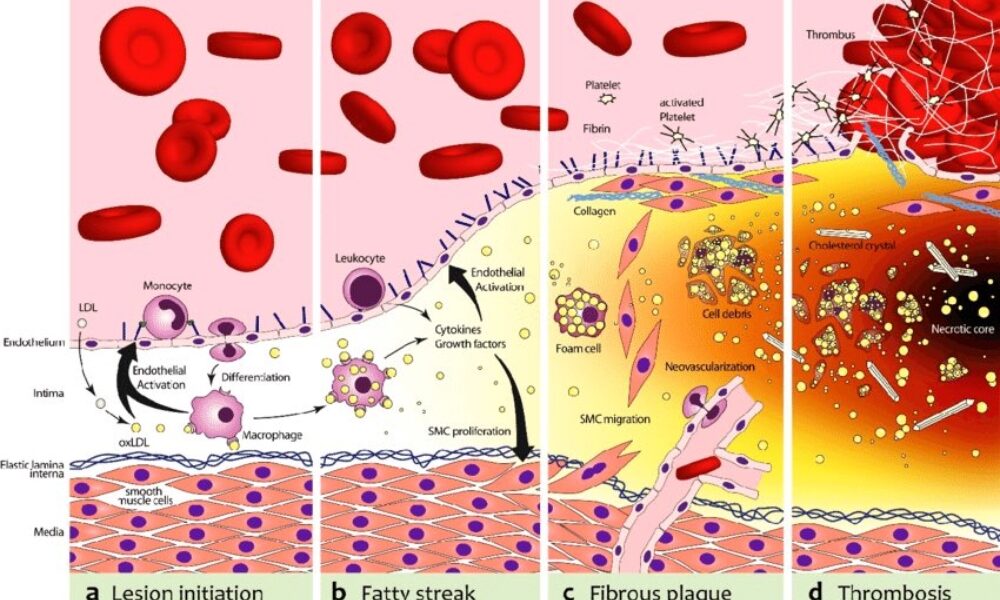
Atherosclerosis, a major contributor to cardiovascular disease, arises from a complex interplay of various factors. Among them, Apolipoprotein B (ApoB) emerges as the primary driver in the development and progression of this condition. In this article, we delve into the critical role of ApoB in atherosclerosis and shed light on the influence of inflammation in enhancing its effects.
Understanding the Role of ApoB:
ApoB, a protein found in lipoproteins such as low-density lipoprotein (LDL) particles, serves as a key player in atherosclerosis. It acts as a carrier, facilitating the transportation of cholesterol to peripheral tissues, including the arterial walls. In the absence of ApoB, the initiation and progression of atherosclerosis are virtually non-existent.
The Significance of ApoB in Atherosclerosis:
ApoB takes center stage in atherosclerosis, as it is responsible for delivering cholesterol-rich lipoproteins, particularly LDL, to arterial walls. These lipoproteins undergo modifications and become trapped in the arterial intima, initiating the formation of fatty streaks. With time, inflammation is triggered, attracting immune cells and accelerating the transformation of fatty streaks into advanced atherosclerotic plaques.
Inflammation and its Role:
While inflammation is a key player in atherosclerosis, it acts as an enhancer rather than the primary driver. Inflammation exacerbates the process by promoting the retention and modification of ApoB-containing lipoproteins, leading to plaque progression and instability. Thus, controlling inflammation becomes crucial in managing atherosclerosis, but addressing the root cause—ApoB—remains essential.
Implications and Therapeutic Strategies:
Understanding the central role of ApoB opens up avenues for therapeutic interventions in managing atherosclerosis. Addressing ApoB levels and reducing the burden of cholesterol-rich lipoproteins is key. Here, lifestyle modifications such as adopting a low-carbohydrate, high-fat diet (such as a ketogenic diet) and implementing intermittent fasting can prove beneficial. These approaches help regulate ApoB-containing lipoproteins, mitigate their retention in arterial walls, and slow down the progression of atherosclerosis.
Furthermore, lifestyle modifications that target additional risk factors associated with atherosclerosis, such as hypertension and obesity, should be considered. Engaging in regular physical activity, maintaining a healthy weight, and managing other comorbidities can complement the efforts to address ApoB and reduce the overall risk of atherosclerosis.
Conclusion:
ApoB stands as the primary driver in the initiation and progression of atherosclerosis, while inflammation serves to enhance and accelerate the process. Recognizing the pivotal role of ApoB provides insights into therapeutic strategies that can mitigate its effects. By adopting lifestyle modifications, such as a low-carbohydrate, high-fat diet and intermittent fasting, individuals can positively influence ApoB levels and manage atherosclerosis. Combining these interventions with measures to address other risk factors offers a comprehensive approach to reducing the burden of atherosclerosis and promoting cardiovascular health.
The biochemical pathway of plaque formation involving ApoB can be described as follows:
- ApoB synthesis: ApoB is a protein synthesized in the liver and intestines. It is a major component of very low-density lipoprotein (VLDL) and LDL particles.
- Lipoprotein assembly: VLDL particles are assembled in the liver and contain ApoB-100. They transport triglycerides and cholesterol from the liver to peripheral tissues. During circulation, VLDL particles undergo enzymatic changes, resulting in the conversion of triglycerides into free fatty acids and glycerol.
- LDL formation: As VLDL particles lose triglycerides, they become smaller and denser, transforming into LDL particles. LDL contains a single molecule of ApoB-100 and is the primary carrier of cholesterol in the bloodstream.
- LDL uptake: LDL particles bind to LDL receptors on cell surfaces, allowing the cells to take up cholesterol. These receptors are present in various tissues, including the arterial walls.
- Retention and modification: In the arterial walls, LDL particles can undergo modifications, such as oxidation and glycation, making them more prone to retention. These modified LDL particles interact with extracellular matrix proteins and proteoglycans in the arterial intima, leading to their entrapment within the vessel walls.
- Inflammation and foam cell formation: The retained LDL particles, along with their cholesterol content, trigger an inflammatory response. Immune cells, particularly macrophages, migrate to the site of inflammation. They engulf the cholesterol-rich LDL particles, transforming into foam cells, which are characterized by their lipid-filled cytoplasm.
- Fatty streak formation: The accumulation of foam cells and other immune cells results in the formation of fatty streaks, which are the initial visible signs of plaque development. Fatty streaks consist of foam cells, lipids, inflammatory cells, and smooth muscle cells.
- Advanced plaque formation: Over time, the fatty streaks can progress into more advanced atherosclerotic plaques. These plaques are characterized by a fibrous cap composed of smooth muscle cells and collagen, a lipid-rich core containing foam cells and cholesterol, and a necrotic center.
Throughout this biochemical pathway, ApoB plays a crucial role in the transport of cholesterol to peripheral tissues, including the arterial walls. It facilitates the delivery of cholesterol-rich LDL particles, which, under certain conditions, contribute to the formation of atherosclerotic plaques. Understanding this pathway provides valuable insights into potential therapeutic targets for preventing and managing plaque formation and related cardiovascular diseases.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
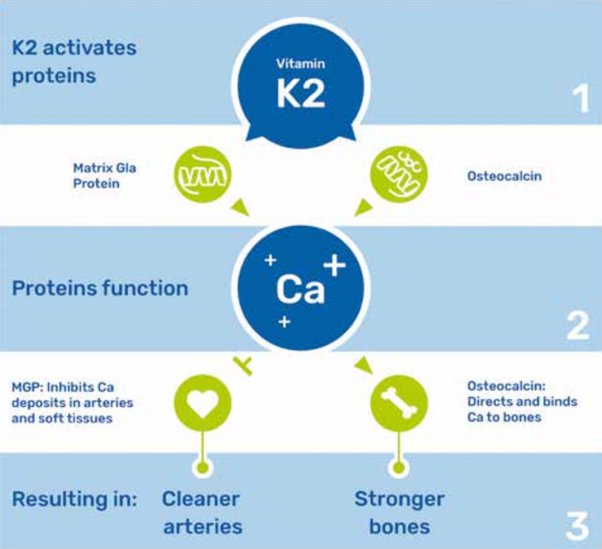
Unlocking the Benefits of Vitamin K2: Clearing Arterial Calcium and Achieving a CAC Score of Zero
by Stephen Fitzmeyer
Introduction: Maintaining cardiovascular health is a top priority for many individuals seeking to lead a long and vibrant life. While regular exercise, a balanced diet, and a healthy lifestyle are crucial elements, recent research has shed light on the potential benefits of vitamin K2 in promoting arterial health. In this article, we delve into the role of vitamin K2 in clearing calcium from arteries, leading to the desirable achievement of a coronary artery calcium (CAC) score of zero.
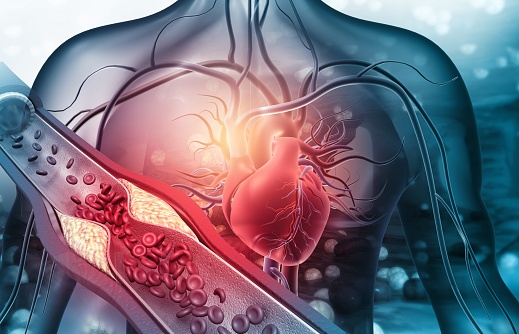
Understanding the Role of Calcium in Arteries: Calcium is an essential mineral for our body, contributing to the formation and strength of bones and teeth. However, when calcium starts accumulating in arterial walls, it can lead to the formation of plaque, narrowing the arteries and hindering blood flow. This process, known as arterial calcification, is a significant risk factor for cardiovascular diseases, including heart attacks and strokes.
Vitamin K2: A Key Player in Arterial Health: Emerging research suggests that vitamin K2 plays a crucial role in maintaining arterial health by effectively managing calcium levels in the body. Vitamin K2 activates proteins that shuttle calcium away from arteries and deposit it in bones, where it is needed. By doing so, vitamin K2 helps to prevent and even reverse arterial calcification.
Clearing Arterial Calcium with Vitamin K2: One of the most remarkable aspects of vitamin K2 is its potential to clear existing arterial calcium deposits. Studies have shown that by ensuring an adequate intake of vitamin K2, individuals with arterial calcification may experience a reduction in the severity of plaque buildup over time. This can lead to improved arterial flexibility and reduced cardiovascular risks.
Achieving a CAC Score of Zero: A coronary artery calcium (CAC) score is a measure of the amount of calcium buildup in the coronary arteries. A score of zero indicates no detectable calcium, which is considered an optimal outcome. While multiple factors contribute to achieving a CAC score of zero, including lifestyle choices and genetics, incorporating vitamin K2 into your routine may play a significant role in promoting arterial health and minimizing calcium deposits.
How to Incorporate Vitamin K2 into Your Routine: To maximize the potential benefits of vitamin K2, it is important to ensure an adequate intake of this nutrient. Vitamin K2 can be found in certain foods, including fermented dairy products, organ meats, and certain cheeses. However, for those who may have limited access to these sources or have dietary restrictions, vitamin K2 supplements are widely available and offer a convenient way to meet the recommended daily intake.
Consult with a Healthcare Professional: As with any dietary change or supplement regimen, it is important to consult with a healthcare professional before incorporating vitamin K2 into your routine. They can assess your individual health needs, provide guidance on appropriate dosages, and help monitor the progress of arterial health through regular check-ups and assessments.
Conclusion: Achieving optimal arterial health and aiming for a CAC score of zero is a significant goal for cardiovascular well-being. While there are multiple factors at play, emerging research highlights the potential of vitamin K2 in promoting arterial health and clearing arterial calcium. By incorporating vitamin K2 into your routine and consulting with a healthcare professional, you can take proactive steps towards supporting your cardiovascular health and enjoying a life free from the burden of arterial calcification.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
CAC: The Ultimate Test for Assessing Health and Why You Need One Now!
By Stephen Fitzmeyer, MD
Introduction
In the realm of healthcare, staying proactive and prioritizing preventive measures is key to maintaining optimal health. The Coronary Artery Calcium (CAC) scoring test has recently emerged as a groundbreaking tool in health assessment, providing invaluable insights into cardiovascular health. This article highlights the significance of CAC as the ultimate test for assessing health and emphasizes why individuals should consider getting one now to safeguard their well-being. Additionally, we’ll explore how patients can easily obtain a CAC scan for themselves.
Understanding CAC Scoring
The Coronary Artery Calcium (CAC) scoring test employs non-invasive computed tomography (CT) scans to detect the presence and extent of calcified plaque in the coronary arteries. By quantifying the amount of calcium present, it calculates a CAC score, effectively gauging the overall burden of atherosclerosis in the arteries. This score serves as a crucial predictor of cardiovascular disease (CVD), empowering individuals to take preventive action.
The Urgency of CAC as a Health Indicator
- Early Detection of Silent Risks: CAC scoring enables early detection of potential cardiovascular issues, even before symptoms manifest. By identifying calcified plaque deposits, healthcare professionals can determine an individual’s risk of experiencing a heart attack or developing coronary artery disease (CAD). Seeking a CAC test now can help unveil hidden risks and prompt timely interventions to prevent disease progression.
- Personalized Risk Assessment: Unlike traditional risk assessment tools, CAC scoring provides a precise evaluation of atherosclerosis. Through quantitative analysis, it offers a more accurate estimation of an individual’s risk of developing CVD. Obtaining a CAC score now empowers healthcare providers to devise personalized treatment plans tailored to an individual’s level of risk, enabling timely interventions and better health outcomes.
- Empowerment for Lifestyle Changes: CAC scoring serves as a powerful motivator for individuals to adopt healthier lifestyles. Witnessing the presence and extent of calcified plaque acts as a visual reminder of the importance of positive changes in diet, exercise, and stress management. By getting a CAC test now, you can proactively take charge of your health, making informed decisions and fostering long-term adherence to beneficial lifestyle modifications.
- Preventive Measures for Long-Term Health: CAC scoring facilitates proactive preventive measures by categorizing individuals into different risk groups based on their CAC scores. This allows healthcare providers to implement appropriate treatments and interventions to reduce the risk of CVD. Taking action now, based on your CAC score, can significantly improve your long-term cardiovascular health and well-being.
How to Obtain a CAC Scan
To obtain a CAC scan, you can follow these steps:
- Consult Your Healthcare Provider: Schedule an appointment with your healthcare provider to discuss your interest in getting a CAC scan. They will evaluate your medical history, risk factors, and overall health to determine if a CAC scan is appropriate for you.
- Referral and Imaging Facility: If your healthcare provider determines that a CAC scan is necessary, they will provide you with a referral to an imaging facility or radiology center equipped to perform the scan.
- Schedule the Scan: Contact the recommended imaging facility and schedule your CAC scan appointment. They will provide you with any necessary instructions, such as fasting requirements or medication restrictions before the test.
- The CAC Scan Procedure: During the CAC scan, you will lie on a table that moves through a CT scanner. The scan is quick and painless, typically taking only a few minutes to complete.
- Results and Follow-up: Once the scan is complete, the radiologist will analyze the images and calculate your CAC score. Your healthcare provider will then review the results with you. They will explain the implications of your CAC score, discuss any necessary lifestyle modifications or medical interventions, and develop a personalized plan to mitigate your cardiovascular risk.
Conclusion
The Coronary Artery Calcium (CAC) scoring test is a powerful tool for assessing cardiovascular health and preventing future complications. By identifying silent risks, providing personalized risk assessment, motivating lifestyle changes, and enabling proactive preventive measures, CAC scoring empowers individuals to take control of their well-being. To obtain a CAC scan, consult your healthcare provider, obtain a referral to an imaging facility, schedule the scan, and discuss the results and follow-up plan with your healthcare provider. Take the proactive step towards optimizing your health and consider getting a CAC scan now. Your heart and overall well-being will thank you for it.
CAC Score
After undergoing a CAC scan, you will receive a CAC score that falls within a specific range. Here are the general ranges and their corresponding meanings:
- CAC Score of 0: A CAC score of 0 indicates the absence of detectable calcified plaque in the coronary arteries. This suggests a very low risk of cardiovascular events, and individuals in this range often have a favorable prognosis.
- CAC Score of 1-99: A CAC score between 1 and 99 indicates the presence of mild calcification in the coronary arteries. This range signifies a low to moderate risk of cardiovascular disease, and it is an opportunity for individuals to implement preventive measures to reduce the progression of plaque formation.
- CAC Score of 100-399: A CAC score between 100 and 399 represents the presence of moderate calcification in the coronary arteries. This range suggests a significant risk of cardiovascular disease, and it necessitates more aggressive preventive strategies and medical interventions to reduce the risk of future complications.
- CAC Score of 400 or Higher: A CAC score of 400 or higher indicates extensive calcification in the coronary arteries. This range represents a high risk of cardiovascular disease, including heart attacks and strokes. It necessitates immediate and intensive medical interventions, including lifestyle modifications and potential medication therapies, to mitigate the risk and prevent further progression.
By understanding the range of CAC scores and their implications, individuals can work closely with their healthcare providers to develop a personalized plan that addresses their specific risk level.
To obtain a CAC scan, consult your healthcare provider, obtain a referral to an imaging facility, schedule the scan, and discuss the results and follow-up plan with your healthcare provider. Take the proactive step towards optimizing your health and consider getting a CAC scan now. Your heart and overall well-being will thank you for it.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/