- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Month: December 2024
The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
Healthcare is at a pivotal moment in history, where technological innovation is redefining how care is delivered, managed, and optimized. At the core of this revolution are Artificial Intelligence (AI), Clinical Informatics, and Machine Learning (ML), fields that intersect to create a paradigm shift in the way we approach health and wellness. This confluence has the potential to enhance decision-making, streamline operations, and improve patient outcomes.
1. Transforming Healthcare Through
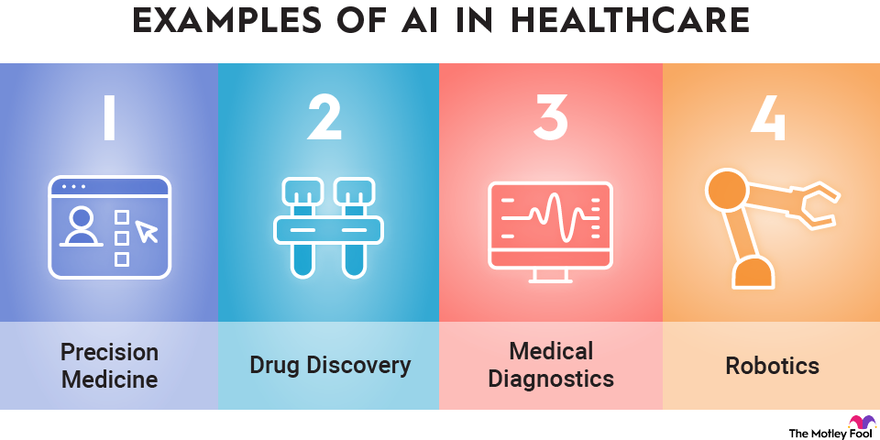
AI brings an unprecedented ability to process and analyze large datasets with speed and accuracy that no human could match. In healthcare, AI is being applied to areas such as:
- Predictive Analytics: AI algorithms can predict patient outcomes based on historical data, enabling proactive intervention. For example, models trained on electronic health record (EHR) data can forecast hospital readmissions or identify patients at risk for chronic diseases.
- Medical Imaging: AI-powered tools can analyze X-rays, MRIs, and CT scans, often detecting anomalies with greater precision than human radiologists.
- Personalized Medicine: AI tailors treatment plans by analyzing genetic, lifestyle, and environmental factors. This ensures therapies are as effective as possible for individual patients.
2. The Role of Clinical Informatics
Clinical Informatics is the backbone of data-driven decision-making in healthcare. It focuses on the optimal use of information and technology to improve patient care and health outcomes. Informatics integrates with AI and ML in several ways:
- Data Integration: Informatics ensures the seamless aggregation and harmonization of diverse healthcare data sources, from EHRs to wearable devices.
- Interoperability: The field promotes standards and protocols that allow AI systems to access and utilize data across different platforms and institutions.
- Clinical Decision Support Systems (CDSS): Informatics integrates AI-driven insights into clinician workflows, enabling smarter, faster, and more accurate decisions at the point of care.
3. Machine Learning as the Engine of Innovation
Machine Learning, a subset of AI, excels at identifying patterns in data and making predictions. In healthcare, ML applications are advancing at a rapid pace:
- Drug Discovery: ML accelerates drug development by predicting how compounds interact with biological systems, reducing the time and cost of bringing new medications to market.
- Operational Efficiency: Hospitals are using ML to optimize staffing, predict supply needs, and improve resource allocation, reducing waste and enhancing patient experiences.
- Natural Language Processing (NLP): ML-powered NLP systems analyze unstructured clinical notes, turning them into actionable insights. This has implications for billing, compliance, and clinical documentation.
4. Ethical and Practical Considerations
While the potential of AI, ML, and Clinical Informatics in healthcare is vast, it is not without challenges:
- Data Privacy and Security: With vast amounts of sensitive health data being processed, ensuring robust cybersecurity measures is critical.
- Bias in Algorithms: AI systems trained on biased datasets can perpetuate disparities in care. Diverse data representation is essential to mitigate this risk.
- Clinician Adoption: Integrating AI tools into clinical practice requires buy-in from healthcare professionals. These tools must be user-friendly and provide clear, actionable insights.
5. The Future of Healthcare
The intersection of AI, Clinical Informatics, and ML is laying the groundwork for a healthcare system that is:
- More Predictive: By identifying health issues before they become critical, we can move from reactive to preventive care.
- More Personalized: Treatments will be increasingly tailored to the unique characteristics of each patient.
- More Efficient: Automation of administrative tasks will allow clinicians to focus more on patient care.
Conclusion
The synergy between AI, Clinical Informatics, and Machine Learning is transforming healthcare into a smarter, more adaptive system. These technologies are not merely tools but catalysts for innovation, enabling a future where healthcare is not only more efficient but also more human.
As we navigate this new frontier, the focus must remain on ensuring ethical implementation, fostering trust among stakeholders, and keeping the patient at the center of every innovation.
Accessing Siloed EMR Systems with FHIR: Connecting to Multiple EMRs
In today’s healthcare landscape, the ability to connect to multiple EMRs (Electronic Medical Records) seamlessly has become crucial for improving patient care, reducing administrative overhead, and driving innovation. However, the diversity in EMR systems, proprietary data formats, and communication protocols has historically made integration a daunting challenge. Enter FHIR (Fast Healthcare Interoperability Resources), the game-changing standard developed by HL7 (Health Level Seven International), which is paving the way for interoperability in healthcare.
The Problem: Siloed EMR Systems
Healthcare providers often use different EMR systems, each designed with unique data structures, interfaces, and workflows. While these systems are essential for managing patient information, they don’t “talk” to each other natively. This lack of interoperability creates data silos, leading to:
- Inefficiencies: Manual data entry and reconciliation slow down workflows.
- Fragmented Care: Providers may not have access to a complete patient history.
- Missed Opportunities: Innovations like patient-facing apps and decision-support tools struggle to integrate across multiple platforms.
The Solution: FHIR as a Universal Language
FHIR offers a standardized framework for accessing and exchanging healthcare information. By leveraging its RESTful API architecture and well-defined data models (resources), FHIR enables seamless integration across multiple EMRs. Here’s how:
- Unified Data Access via FHIR APIs Modern EMR systems like Epic, Cerner, and Allscripts have adopted FHIR APIs as part of their platforms. This standardization allows external applications to retrieve and interact with data like patient demographics, medications, and lab results without requiring custom integration for each EMR.
- Standardized Resources FHIR resources—such as Patient, Observation, Encounter, and Medication—act as reusable data models. These resources provide a consistent structure across systems, making it easier for developers to query and update data in a predictable way, regardless of the underlying EMR.
- SMART on FHIR for Authentication The SMART on FHIR framework adds an additional layer by standardizing the way apps authenticate and gain authorized access to EMR data using OAuth 2.0. This ensures secure, scalable integration while respecting patient privacy and data security regulations like HIPAA.
Benefits of Connecting to Multiple EMRs
- Streamlined Care Coordination FHIR enables providers to access and share patient data across different healthcare systems. A specialist in one hospital can view relevant records from another provider’s EMR, ensuring continuity of care.
- Simplified Integration for Developers Developers can create third-party applications, such as telehealth platforms or chronic disease management tools, that work with multiple EMRs out of the box. Instead of writing custom connectors for each system, developers interact with a single FHIR-based API.
- Empowering Patients Patient-facing apps can use FHIR to aggregate data from multiple EMRs, giving individuals a unified view of their health records. This transparency improves patient engagement and health outcomes.
- Faster Innovation The reduced complexity of integrating with EMRs allows startups and innovators to focus on building features that directly improve care delivery rather than wrestling with legacy integration challenges.
Challenges to Consider
While FHIR greatly simplifies the process of connecting to multiple EMRs, it’s not without challenges:
- Vendor Variability: Not all EMRs implement FHIR in the same way. Developers may encounter slight differences in API behavior across systems.
- Data Gaps: Older EMRs or smaller providers might not support FHIR, requiring fallback mechanisms.
- Access Control: Even with FHIR, gaining authorized access to data involves navigating organizational policies and regulatory requirements.
The Future of EMR Connectivity
As FHIR adoption continues to grow, the dream of a truly interoperable healthcare ecosystem is becoming a reality. Initiatives like the 21st Century Cures Act in the United States mandate that EMR vendors provide FHIR APIs to improve data access and patient empowerment. This regulatory push, combined with advancements in technology, means that healthcare organizations can now leverage FHIR to unlock the full potential of their data.
Conclusion
Connecting to multiple EMRs is no longer an insurmountable challenge. With FHIR as the universal standard, healthcare providers, developers, and patients can break down data silos, enabling seamless information exchange and fostering innovation. Whether you’re building a new application or improving workflows in your organization, FHIR offers the tools to bridge the gaps between EMRs and create a more connected healthcare future.
How AI Can Transform Healthcare Applications
How AI Can Transform Healthcare Applications
As a developer of healthcare applications, you’re constantly looking for ways to improve functionality, efficiency, and user experience. Artificial Intelligence (AI) offers a transformative opportunity to enhance healthcare apps, making them smarter, more user-friendly, and impactful. Here’s how AI can elevate your healthcare applications to the next level.
1. Enhancing Patient Care and Management
- Personalized Treatment Recommendations: AI algorithms analyze patient data like lab results, genetic information, and medical history to suggest tailored treatment plans.
- Virtual Assistants: Chatbots powered by natural language processing (NLP) can answer common patient questions, help schedule appointments, and remind patients about medications.
- Predictive Analytics: AI models predict potential health issues, such as diabetes or cardiovascular disease, allowing for early intervention and better patient outcomes.
2. Supporting Clinical Decision-Making
- AI Diagnosis Tools: Machine learning can analyze medical images, lab tests, or patient-reported symptoms to help identify conditions quickly and accurately.
- Drug Interaction Alerts: AI systems can flag potential drug interactions or contraindications based on a patient’s medication history.
- Risk Assessment Models: Predictive models assess patient risks for conditions like stroke or sepsis, enabling proactive care.
3. Optimizing Workflow
- Automated Documentation: NLP tools transcribe and summarize doctor-patient conversations, reducing administrative burdens.
- Intelligent Scheduling: AI-powered tools optimize staff and appointment scheduling, minimizing wait times and maximizing resource utilization.
- Claims Automation: Automate insurance claim reviews with AI, reducing errors and speeding up reimbursement processes.
4. Enhancing Telemedicine and Remote Monitoring
- AI Diagnostics: Enhance telehealth platforms with tools that analyze patient-reported data or uploaded images during virtual consultations.
- Wearable Data Integration: Develop AI algorithms to process data from wearables, offering actionable insights into patient health.
- Symptom Checkers: AI-driven tools allow patients to input symptoms and receive preliminary assessments, streamlining triage.
5. Delivering Data Insights and Analytics
- Patient Cohort Analysis: AI identifies patterns in patient populations, improving treatment strategies and research.
- Health Trend Forecasting: Analyze big data to predict public health trends or disease outbreaks.
- Operational Efficiency: Use AI to optimize inventory, staffing, and resource allocation in clinical settings.
6. Improving Patient Engagement
- Conversational Interfaces: Enable patients to interact with your app through natural language queries, making healthcare more accessible.
- Gamification: Use AI to personalize gamified elements, encouraging adherence to treatment plans or healthy behaviors.
- Educational Content: Deliver tailored educational materials based on a patient’s condition or interests.
7. Ensuring Compliance and Security
- Data Anonymization: AI can de-identify sensitive patient data for compliance with regulations like HIPAA and GDPR.
- Fraud Detection: AI detects anomalies in billing or prescriptions that may indicate fraud.
- Secure Data Sharing: Facilitate secure and efficient sharing of patient records among healthcare providers.
8. Facilitating Research and Development
- Clinical Trial Matching: Match eligible patients to clinical trials using AI-driven analysis of their medical profiles.
- Drug Discovery: Use AI models to simulate and analyze potential drug compounds.
- Real-World Evidence: Generate insights from patient data to support post-market surveillance and drug efficacy studies.
9. Expanding Accessibility
- Language Translation: Offer multilingual support for diverse patient populations with AI translation tools.
- Accessibility Features: Build AI-driven speech-to-text and text-to-speech features for patients with disabilities.
10. Elevating User Experience
- Predictive Navigation: Anticipate user actions to streamline navigation and improve usability.
- Behavioral Nudges: Deliver proactive reminders or nudges, such as medication adherence prompts, based on user behavior.
- Dynamic Interfaces: Personalize app interfaces based on user preferences and engagement patterns.
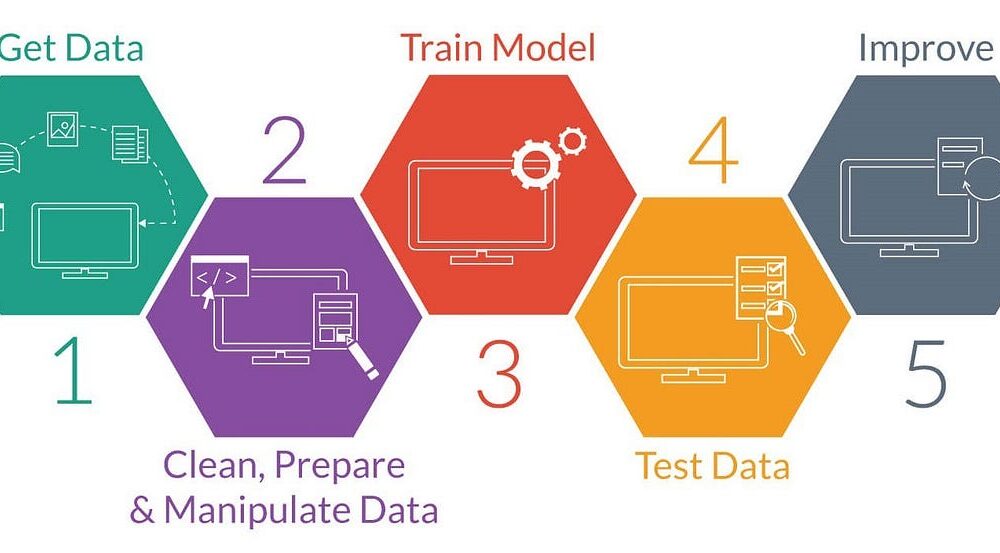
Example: Implementing an AI-Powered Symptom Checker
Here’s an example of how you might structure an app to include a symptom checker using AI:
- Input Collection: The app asks users to input symptoms via text or voice.
- Natural Language Processing (NLP): AI processes the input to extract relevant medical terms and symptoms.
- Symptom Analysis: The app uses a machine learning model trained on a medical dataset to compare the user’s symptoms with known patterns of illnesses.
- Recommendation Engine: Based on the analysis, the app provides possible conditions and suggests whether the user should seek immediate care, consult a doctor, or try home remedies.
- Continuous Learning: The app collects anonymized feedback from user interactions to improve the accuracy of the model over time.
Example Code for NLP Symptom Processing:
from transformers import pipeline
# Load a pre-trained NLP model for healthcare applications
nlp_model = pipeline("text-classification", model="bert-base-healthcare")
# Example user input
user_input = "I have a persistent cough and shortness of breath."
# Process the input
analysis = nlp_model(user_input)
# Output AI-generated insights
print("Potential conditions:", analysis)
This code snippet demonstrates how to use a pre-trained NLP (Natural Language Processing) model from the Hugging Face transformers library to classify text related to healthcare applications. Here’s a breakdown of what each part of the code does:
1. Importing pipeline from the transformers library
from transformers import pipelineThe pipeline function provides an easy interface to use pre-trained models for various NLP tasks like text classification, question answering, translation, etc.
2. Loading a Pre-trained NLP Model
nlp_model = pipeline("text-classification", model="bert-base-healthcare")pipeline("text-classification"): This specifies that the task is text classification, where input text will be categorized into predefined classes or labels.model="bert-base-healthcare": Refers to a pre-trained BERT (Bidirectional Encoder Representations from Transformers) model fine-tuned for healthcare-related text classification. This specific model would likely be trained to understand healthcare vocabulary and contexts.
3. Processing User Input
user_input = "I have a persistent cough and shortness of breath."
analysis = nlp_model(user_input)The pipeline processes the input text using the loaded model to predict potential conditions or categories related to the input.
4. Outputting Results
print("Potential conditions:", analysis)The analysis variable contains the model’s predictions, such as potential health conditions or relevant categories for the provided symptoms.
Example Output
Potential conditions: [{'label': 'Respiratory Issue', 'score': 0.95}]- label: The predicted category (e.g., “Respiratory Issue”).
- score: The confidence score for this prediction (e.g., 0.95, indicating 95% confidence).
Use Case
This code can be part of a healthcare chatbot, clinical decision support system, or any application designed to provide preliminary insights based on patient symptoms. However, these AI-generated insights should not replace professional medical advice.
Getting Started with AI Integration
To start incorporating AI into your healthcare applications:
- Start Small: Begin with a single AI feature, such as a chatbot or predictive analytics, to test feasibility and user acceptance.
- Prioritize Data Quality: Ensure clean, accurate data to power your AI models effectively.
- Focus on Ethics: Build trust by maintaining transparency, privacy, and fairness in AI algorithms.
- Iterate and Scale: Use feedback to refine AI functionalities and expand capabilities over time.
AI is reshaping healthcare, offering exciting opportunities to create more impactful applications. By leveraging AI, you can provide better care, improve efficiency, and drive innovation in healthcare technology.