- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Year: 2023
Navigating the Ketogenic Diet with Intermittent Fasting for Type 1 Diabetics: A Safe Approach to Managing Blood Sugar with Modern Technology
Introduction: Embracing a ketogenic diet, characterized by low carbohydrate intake and high fat consumption, along with intermittent fasting (IF), holds potential health benefits. But what about individuals with Type 1 Diabetes who rely on insulin for blood sugar management? Can they safely adopt a ketogenic lifestyle? In this article, we will explore how individuals with Type 1 Diabetes can safely navigate a ketogenic diet with the inclusion of intermittent fasting, ensuring stable blood sugar control and optimized health outcomes. With modern technology, such as the t:slim X2 Insulin Pump, monitoring blood sugars has become easier than ever.
Understanding Type 1 Diabetes and the Ketogenic Diet: Type 1 Diabetes is an autoimmune condition where the pancreas fails to produce sufficient insulin, resulting in high blood sugar levels. Traditionally, carbohydrate counting and insulin dosing have been vital for managing blood sugar. However, the ketogenic diet offers an alternative approach by minimizing carbohydrate intake, which can help stabilize blood sugar levels and reduce the need for large insulin doses.
Safely Adopting the Ketogenic Diet:
- Consult with Healthcare Professionals: Seek guidance from your healthcare team, including a registered dietitian and endocrinologist, to ensure a safe and effective transition to a ketogenic diet with intermittent fasting. They can provide personalized advice and help adjust insulin doses accordingly.
- Utilize Modern Technology: Take advantage of modern technology, such as the t:slim X2 Insulin Pump, which makes monitoring blood sugars easier than ever. This pump offers advanced features like continuous glucose monitoring (CGM) integration, insulin delivery adjustments, and data tracking, allowing for better management of blood sugar levels.
- Monitor Blood Sugar: Regularly monitor your blood sugar levels, especially during the initial stages of transitioning to a ketogenic diet. Frequent testing, combined with the convenience of devices like the t:slim X2 Insulin Pump, helps identify trends, make necessary insulin dose adjustments, and modify your diet accordingly.
- Individualized Carbohydrate Intake: Work with a registered dietitian experienced in managing diabetes to determine the appropriate carbohydrate limit for your specific needs, considering factors such as insulin sensitivity, activity levels, and overall health.
- Timing of Meals and Insulin: Intermittent fasting can be incorporated into the ketogenic diet, but it requires careful planning. Collaborate closely with your healthcare team to determine the best fasting and eating windows while considering insulin requirements and blood sugar control.
Benefits of Ketogenic Diet with IF for Type 1 Diabetics:
- Blood Sugar Stability: By reducing carbohydrate intake, individuals with Type 1 Diabetes may experience more stable blood sugar levels, reducing the risk of extreme highs and lows.
- Improved Insulin Sensitivity: The combination of a ketogenic diet and intermittent fasting may improve insulin sensitivity, making it easier to manage blood sugar levels and potentially reducing the need for high insulin doses.
- Weight Management: The ketogenic diet, coupled with intermittent fasting, may aid in weight management, which is beneficial for individuals with Type 1 Diabetes who may be at a higher risk of weight fluctuations.
- Potential for Fewer Complications: Maintaining stable blood sugar levels and reducing the need for high insulin doses may lower the risk of long-term complications associated with Type 1 Diabetes.
Conclusion: While the ketogenic diet and intermittent fasting hold potential benefits for individuals with Type 1 Diabetes, it is crucial to approach them with caution and under the guidance of healthcare professionals. With modern technology, such as the t:slim X2 Insulin Pump, monitoring blood sugars has become easier than ever, allowing for better control and management. Working closely with your healthcare team, including a registered dietitian and endocrinologist, will ensure a safe and effective transition to a ketogenic diet with intermittent fasting. Together, you can develop an individualized plan that considers your insulin requirements, blood sugar levels, and overall health goals. With the right support and modern tools at your disposal, it is possible for individuals with Type 1 Diabetes to safely embrace a ketogenic lifestyle and experience the potential benefits it offers in blood sugar management and overall well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Ketogenic Diet Cheat Sheet
The ketogenic diet is a low-carbohydrate, high-fat diet that can help you achieve various health benefits, including weight loss, improved mental clarity, and increased energy levels. To make it easier for you to follow the ketogenic lifestyle, we have prepared a handy cheat sheet with essential guidelines and food recommendations. Keep this cheat sheet handy to stay on track and make informed choices while following a ketogenic diet.
- Macronutrient Ratio:
- Carbohydrates: Limit daily carbohydrate intake to 20-50 grams or less, depending on your individual needs and goals.
- Protein: Consume a moderate amount of protein, typically around 0.6-1 gram per pound of lean body mass.
- Fats: Make healthy fats the primary source of calories in your diet, aiming for approximately 70-75% of your daily caloric intake.
- Foods to Include:
- Healthy Fats: Avocado, coconut oil, olive oil, butter, ghee, nuts and seeds, fatty fish (such as salmon and mackerel).
- Protein Sources: Meat (beef, poultry, pork), eggs, fish, seafood, tofu, tempeh.
- Non-Starchy Vegetables: Leafy greens (spinach, kale, lettuce), broccoli, cauliflower, zucchini, asparagus, peppers.
- Dairy: Full-fat cheese, heavy cream, Greek yogurt (in moderation, as dairy can be higher in carbs).
- Beverages: Water, unsweetened tea or coffee, herbal tea, bone broth.
- Foods to Avoid:
- Grains: Wheat, rice, oats, corn, barley, quinoa, and other grains.
- Legumes: Beans, lentils, chickpeas, and soy-based products.
- Sugar and Sweeteners: Avoid all forms of sugar, including table sugar, honey, maple syrup, agave nectar, and artificial sweeteners.
- High-Carb Fruits: Bananas, grapes, apples, oranges, and other high-sugar fruits. Instead, opt for berries in moderation.
- Processed Foods: Packaged snacks, sugary drinks, processed meats (such as sausages and deli meats), and pre-packaged meals.
- Snack Ideas:
- Hard-boiled eggs
- Nuts and seeds (almonds, walnuts, chia seeds)
- Cheese slices or cubes
- Avocado or guacamole
- Celery sticks with almond butter
- Olives
- Tips for Success:
- Stay Hydrated: Drink plenty of water throughout the day to maintain hydration and support bodily functions.
- Read Labels: Pay attention to food labels and ingredient lists to ensure products are low in carbs and free from hidden sugars.
- Plan and Prep: Plan your meals in advance, batch cook, and have keto-friendly snacks readily available to avoid making impulsive food choices.
- Seek Support: Connect with others following a ketogenic lifestyle for motivation, recipe ideas, and tips.
Remember, everyone’s dietary needs may vary, so it’s essential to listen to your body and make adjustments as necessary. Consult with a healthcare professional or registered dietitian before starting any new diet or making significant changes to your eating habits.
Stay committed, be mindful of your food choices, and enjoy the numerous benefits that the ketogenic diet can offer.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Exploring the Potential of Ketogenic Diet and Intermittent Fasting in Schizoaffective Disorder Management
Introduction:
Schizoaffective disorder is a complex psychiatric condition characterized by a combination of mood disorders, such as bipolar disorder or major depression, and schizophrenia symptoms. While medication and therapy are commonly used in its treatment, emerging research suggests that dietary interventions, specifically the ketogenic diet and intermittent fasting, may hold promise in managing symptoms and improving overall well-being for individuals with schizoaffective disorder. In this article, we will explore the potential efficacy of adopting a ketogenic diet and intermittent fasting in the management of schizoaffective disorder.
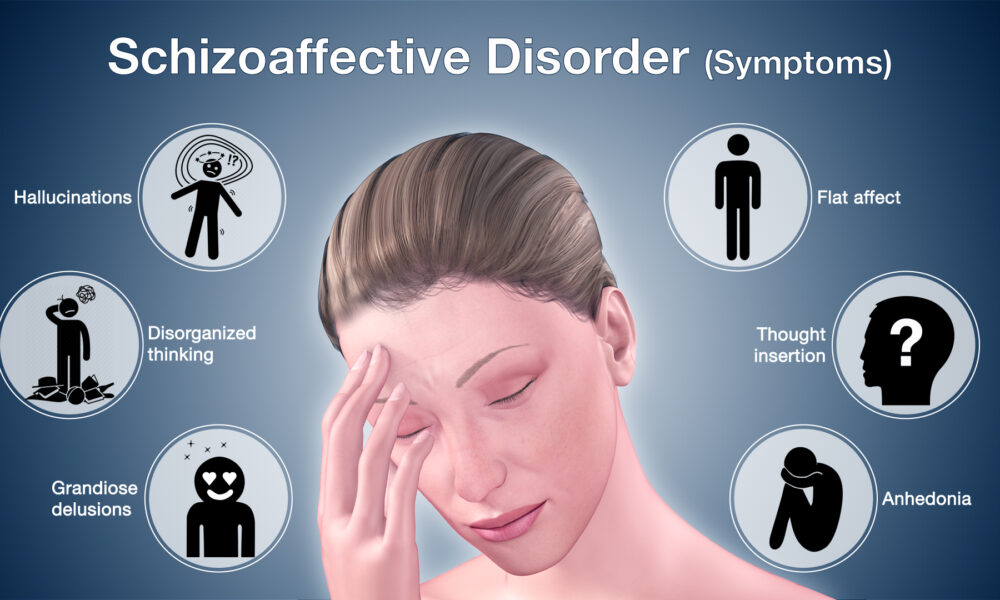
Understanding Schizoaffective Disorder:
Schizoaffective disorder is a challenging mental health condition that often requires a comprehensive approach to treatment. It is characterized by a range of symptoms, including hallucinations, delusions, disorganized thinking, mood disturbances, and cognitive impairments. Conventional treatment typically involves a combination of antipsychotic medications, mood stabilizers, and psychotherapy.
The Potential Benefits of Ketogenic Diet:
- Enhanced Mood Stability: The ketogenic diet has been associated with improved mood regulation and stability. By stabilizing blood sugar levels and providing a steady supply of ketones to the brain, the diet may help mitigate mood swings and promote emotional balance, potentially benefiting individuals with schizoaffective disorder.
- Cognitive Improvements: Cognitive impairments are common in schizoaffective disorder. The ketogenic diet has shown potential in enhancing cognitive function, including memory and attention. The neuroprotective properties of ketones may help support neuronal health and improve cognitive performance in individuals with schizoaffective disorder.
- Reduction in Inflammation: Inflammation has been linked to the development and progression of psychiatric disorders. The ketogenic diet’s anti-inflammatory effects may help mitigate neuroinflammation, potentially contributing to the management of symptoms in schizoaffective disorder.
The Potential Benefits of Intermittent Fasting:
- Neuroprotective Effects: Intermittent fasting has been shown to induce cellular stress responses that promote cellular repair and resilience. This process, known as autophagy, may help clear damaged cells and dysfunctional proteins, potentially improving neuronal health and protecting against the progression of schizoaffective disorder.
- Regulation of Mood: Intermittent fasting has been associated with improvements in mood and mental well-being. The regulation of neurotransmitters and the production of brain-derived neurotrophic factor (BDNF) during fasting periods may contribute to mood stabilization and alleviate depressive symptoms commonly associated with schizoaffective disorder.
- Improved Antipsychotic Medication Efficacy: Some research suggests that intermittent fasting may enhance the effectiveness of antipsychotic medications. Fasting-related changes in metabolic processes and gene expression may influence drug metabolism and efficacy, potentially leading to better symptom management.
Considerations and Consultation:
It is crucial to approach the implementation of a ketogenic diet or intermittent fasting under the guidance of healthcare professionals experienced in these dietary interventions, especially when managing a complex condition like schizoaffective disorder. They can provide individualized recommendations, monitor progress, and ensure nutritional needs are met.
It is important to note that dietary interventions should be integrated into a comprehensive treatment plan that includes regular psychiatric evaluation, medication management, therapy, and other supportive measures tailored to the individual’s needs.
Conclusion:
While research on the specific effects of ketogenic diet and intermittent fasting in schizoaffective disorder is limited, emerging evidence suggests their potential benefits in managing symptoms and improving overall well-being. These dietary interventions have shown promise in mood stabilization, cognitive enhancement, reduction of inflammation, and neuroprotection. As with any treatment approach, it is crucial to consult with healthcare professionals to tailor these interventions to individual needs and ensure comprehensive care. Further research is needed to
further investigate the efficacy, safety, and long-term effects of ketogenic diet and intermittent fasting in schizoaffective disorder.
As the field of nutritional psychiatry continues to evolve, exploring the potential of dietary interventions in the management of schizoaffective disorder is an exciting area of research. The ketogenic diet and intermittent fasting offer unique mechanisms that may complement conventional treatment approaches and improve outcomes for individuals with this complex condition.
However, it is important to approach these interventions with caution and under the supervision of healthcare professionals. Each person’s response to dietary changes can vary, and careful monitoring is necessary to ensure that nutritional needs are met, potential side effects are addressed, and the interventions are integrated effectively into the overall treatment plan.
Future studies should focus on conducting rigorous clinical trials to investigate the specific effects of ketogenic diet and intermittent fasting in schizoaffective disorder. This research should explore optimal dietary protocols, long-term sustainability, potential interactions with medications, and the impact on specific symptoms and functional outcomes.
In conclusion, while the ketogenic diet and intermittent fasting show promise in the management of schizoaffective disorder, further research is needed to establish their efficacy, safety, and long-term effects. By combining the advancements in nutritional psychiatry with conventional treatment approaches, we may unlock new possibilities for improving the lives of individuals with schizoaffective disorder and enhancing their mental well-being.
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Nutritional Psychiatry: Harnessing the Power of Ketogenic Diet and Intermittent Fasting for Mental Well-being
Introduction:
The field of nutritional psychiatry is gaining recognition as research increasingly highlights the profound connection between diet and mental health. Emerging evidence suggests that dietary interventions, such as the ketogenic diet and intermittent fasting, can play a significant role in the treatment of psychiatric disorders. In this article, we will explore the potential benefits of adopting a ketogenic diet and intermittent fasting as therapeutic strategies for improving mental well-being.
The Ketogenic Diet: Nourishing the Brain
The ketogenic diet is a low-carbohydrate, high-fat eating plan that shifts the body’s metabolism into a state of ketosis. This metabolic state prompts the production of ketones, which become the brain’s primary fuel source, replacing glucose. Here’s how the ketogenic diet can positively impact mental health:
- Stabilizing Mood and Mental Clarity: The ketogenic diet has been associated with improved mood stability and mental clarity. By reducing blood sugar fluctuations and providing a steady supply of ketones to the brain, the diet may help regulate neurotransmitters and promote a balanced emotional state.
- Reducing Inflammation: Chronic inflammation is often linked to psychiatric disorders. The ketogenic diet has shown anti-inflammatory effects, potentially alleviating inflammation in the brain and contributing to improved mental health outcomes.
- Enhancing Neuroprotection: Ketones produced during ketosis have neuroprotective properties, potentially shielding the brain from oxidative stress and supporting neuronal function. This neuroprotective effect may be particularly relevant in the treatment of conditions such as Alzheimer’s disease and epilepsy.
Intermittent Fasting: Resetting the Mind and Body
Intermittent fasting (IF) involves cycling between periods of eating and fasting, which can have profound effects on brain function and mental well-being. Here are some ways IF may benefit mental health:
- Promoting Autophagy: During fasting periods, the body enters a state of autophagy, a process where damaged cells and cellular components are recycled and cleared. Autophagy supports cellular renewal and may play a vital role in clearing protein aggregates associated with neurodegenerative disorders.
- Enhancing Brain-Derived Neurotrophic Factor (BDNF): IF has been shown to increase the production of BDNF, a protein crucial for the growth and survival of neurons. Higher levels of BDNF have been associated with improved mood, cognitive function, and the prevention of mental disorders.
- Regulating Circadian Rhythms: IF helps regulate the body’s internal clock, which governs various physiological processes, including sleep patterns. Proper regulation of circadian rhythms is essential for mental well-being, as disruptions can contribute to mood disorders and cognitive impairments.
Implementing a Nutritional Psychiatry Approach
While the ketogenic diet and intermittent fasting show promise in the treatment of psychiatric disorders, it is essential to approach these interventions with care and under professional guidance. Here are a few considerations:
- Personalization: Nutritional psychiatry interventions should be tailored to individual needs and goals. Consulting with a healthcare professional or registered dietitian experienced in these approaches can help determine the most suitable strategies.
- Monitoring and Evaluation: Regular monitoring of mental health symptoms and overall well-being is crucial during dietary interventions. Adjustments to the diet or fasting protocols may be necessary to optimize outcomes.
- Comprehensive Approach: Nutritional psychiatry should be considered as part of a holistic approach to mental health. It is essential to address other aspects such as exercise, sleep, stress management, and social support to achieve optimal outcomes.
Conclusion:
The emerging field of nutritional psychiatry highlights the powerful impact of diet on mental well-being. The ketogenic diet and intermittent fasting offer promising strategies for treating psychiatric disorders by nourishing the brain, reducing inflammation, promoting
Author: Dr. Stephen Fitzmeyer, M.D.
Physician Informaticist and Founder of Warp Core Health
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Understanding the Distinctions: Biomedical Informatics, Clinical Informatics, and Health Informatics
By Stephen Fitzmeyer, MD
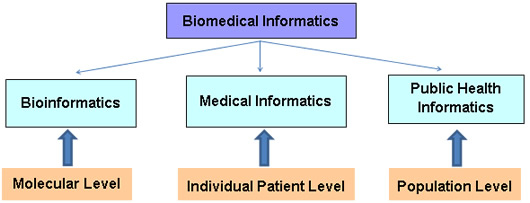
In today’s digital age, the field of informatics plays a crucial role in transforming healthcare by harnessing the power of technology and data. Within this expansive field, three distinct disciplines often come into play: biomedical informatics, clinical informatics, and health informatics. While these terms may seem interchangeable at first glance, they each encompass unique areas of focus and expertise. Let’s delve into the differences between these three disciplines to gain a clearer understanding.
Biomedical Informatics:
Biomedical informatics, sometimes referred to as bioinformatics, revolves around the intersection of biology, medicine, and computational sciences. It focuses on leveraging technology, data analysis, and information systems to advance biomedical research, discovery, and understanding. Biomedical informatics professionals work on developing tools and methodologies to store, manage, analyze, and interpret vast amounts of biological and clinical data.
The scope of biomedical informatics spans genomics, proteomics, imaging data, clinical trials, and more. By employing computational and analytical approaches, experts in this field can identify patterns, discover new insights, and enhance our understanding of complex biological processes. Biomedical informatics plays a vital role in areas such as personalized medicine, drug discovery, and precision healthcare.
Clinical Informatics:
Clinical informatics centers on the effective use of information and communication technologies in healthcare settings, with a primary focus on improving patient care and outcomes. It encompasses the application of informatics principles and methods to facilitate clinical decision-making, enhance workflow efficiencies, and optimize healthcare delivery.
Clinical informatics professionals bridge the gap between healthcare providers and technology. They ensure the successful implementation and utilization of electronic health records (EHRs), clinical decision support systems, computerized physician order entry (CPOE), and other healthcare information systems. They work to streamline data capture, facilitate interoperability between systems, and promote data-driven approaches to patient care.
Health Informatics:
Health informatics takes a broader perspective, encompassing both biomedical and clinical informatics while extending its reach to population health, public health, and healthcare management. Health informatics focuses on the collection, management, and analysis of health-related data to improve healthcare delivery, policy-making, and population health outcomes.
Professionals in health informatics leverage technology and information systems to monitor and assess population health trends, support public health initiatives, and facilitate data-driven decision-making. They play a crucial role in developing and implementing health information exchanges, health analytics, telemedicine, and health data standards to ensure seamless data exchange and enhance healthcare delivery on a larger scale.
In essence, while biomedical informatics concentrates on advancing scientific research through data analysis, clinical informatics focuses on optimizing clinical workflows and patient care delivery. Health informatics takes a broader perspective, incorporating both biomedical and clinical informatics while extending its scope to population health and healthcare management.
By understanding the distinctions between biomedical informatics, clinical informatics, and health informatics, we gain a deeper appreciation for the specialized roles each discipline plays in shaping the future of healthcare. Together, they contribute to the advancement of medical knowledge, optimization of clinical processes, and improvement of overall healthcare outcomes for individuals and populations alike.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
- ‹ Previous
- 1
- …
- 3
- 4
- 5