- Home
- About
- Portfolio
Crush the Match – Medical School and Residency Platform
Food¢ense – Curbing Childhood Obesity and Food Waste
HealthStack – Shared and Jailed HIPAA Hosting $50
Marta Care – Let Us Help When You Can’t
MD Idea Lab – We Build Prototypes for Doctors
Nervcell – The Healthcare Web Browser
Patient Keto – Personalized Keto Medicine and Telehealth
SwipeChart – Rapid EMR Interface
Treatment Scores – Quantifying the Science of Medicine
Treatments – Diagnosed. Now What?
VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
- Home
- Warp Core Health
- Blog
- 2023
- August
Month: August 2023
Are You One of the 88% of the the U.S. Adult Population suffering from Chronic Inflammation? Here’s what you should know to find out and fix it.
- August 15, 2023
- Stephen Fitzmeyer, MD
- No Comments
By Stephen Fitzmeyer, MD
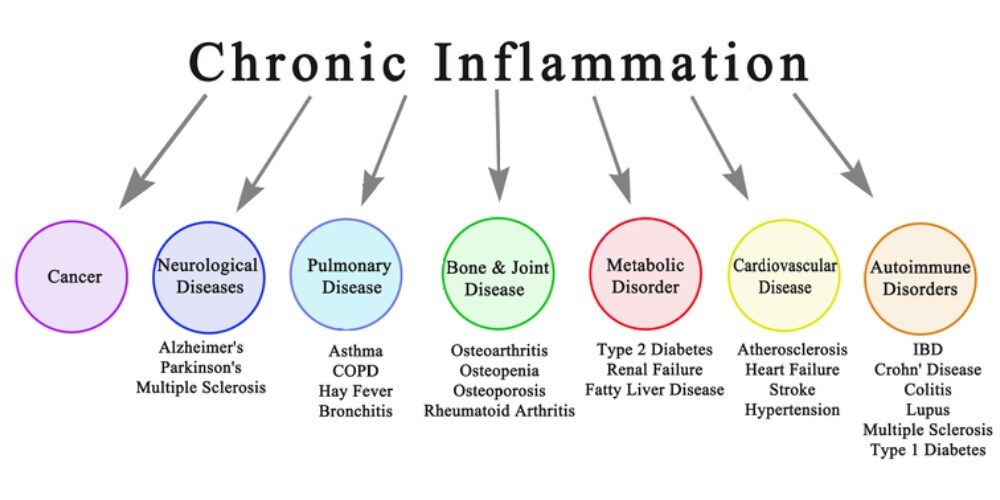
Introduction: Chronic inflammation is a silent yet powerful contributor to various health problems. It serves as a warning sign of underlying conditions such as metabolic syndrome, poor diet, and other chronic diseases. In this article, we aim to shed light on the detrimental effects of chronic inflammation and emphasize the significance of making positive lifestyle changes to prevent its progression and the onset of related health issues.
Chronic inflammation has been linked to the development of several chronic diseases, including cardiovascular disease, type 2 diabetes, autoimmune disorders, obesity, cancer, neurodegenerative diseases, and respiratory diseases. Understanding the significant impact of chronic inflammation on these chronic diseases highlights the urgency of addressing inflammation through lifestyle modifications.
Part 1: Chronic Inflammation and its Link to Metabolic Syndrome
Chronic inflammation is closely intertwined with metabolic syndrome, a cluster of conditions that includes obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels. This syndrome sets the stage for chronic inflammation, fueling a vicious cycle. As chronic inflammation persists, it further promotes the development of metabolic abnormalities, increasing the risk of cardiovascular disease, type 2 diabetes, and other chronic illnesses.
Part 2: The Role of Diet in Chronic Inflammation
A poor diet plays a significant role in chronic inflammation. Consuming processed foods high in refined carbohydrates, added sugars, unhealthy fats, and artificial additives triggers an inflammatory response within the body. Moreover, the excessive intake of omega-6 fatty acids found in seed oils, commonly used in processed foods, promotes an imbalance in the omega-6 to omega-3 ratio, further exacerbating inflammation. To reduce chronic inflammation, it is important to avoid seed oils such as soybean oil, corn oil, sunflower oil, and cottonseed oil, and instead opt for healthier alternatives like olive oil, avocado oil, and coconut oil.
Part 3: Inflammatory Markers to Assess Chronic Inflammation
If you suspect chronic inflammation, your physician may order specific blood tests to assess inflammatory markers in your body. These markers can provide valuable insights into the presence and extent of inflammation. Common inflammatory markers include:
- C-reactive Protein (CRP): Elevated CRP levels indicate systemic inflammation and can be indicative of various diseases.
- Erythrocyte Sedimentation Rate (ESR): ESR measures the rate at which red blood cells settle in a tube, which can be elevated during inflammation.
- Interleukin-6 (IL-6): IL-6 is a cytokine involved in the inflammatory response, and increased levels may indicate ongoing inflammation.
- Tumor Necrosis Factor-alpha (TNF-α): TNF-α is another cytokine associated with inflammation, and elevated levels are observed in chronic inflammatory conditions.
- Fasting Insulin: Insulin resistance, often associated with chronic inflammation, can be assessed through fasting insulin levels.
Part 4: Taking Control: Lifestyle Changes to Combat Chronic Inflammation
The good news is that chronic inflammation is not entirely beyond our control. By making positive lifestyle changes, we can reduce its impact and mitigate the risks associated with it. Here are some key steps to consider:
- Adopting a Healthy Diet: By adopting a high-fat, low-carb diet rich in healthy fats, adequate protein, and non-starchy vegetables, you can reduce chronic inflammation, enhance your overall well-being, and enjoy a healthier and more vibrant life. Emphasize foods such as fatty fish, grass-fed meats, eggs, nuts, seeds, avocados, olive oil, and non-starchy vegetables. Avoid processed foods, sugary beverages, and seed oils high in omega-6 fatty acids, as they contribute to inflammation.
- Regular Exercise: Engage in regular physical activity to combat obesity, improve insulin sensitivity, and reduce systemic inflammation.
- Stress Management: Chronic stress contributes to inflammation. Incorporate stress management techniques such as meditation, mindfulness, and relaxation exercises into your routine.
Conclusion: Chronic inflammation is a red flag indicating underlying health issues and the potential development of chronic diseases. Metabolic syndrome, poor diet, and other factors contribute to its persistence. By recognizing the role of chronic inflammation in these conditions, we can take proactive steps to address it through lifestyle modifications. Adopting a healthy diet, engaging in regular exercise, managing stress, and avoiding seed oils are crucial in combating chronic inflammation and reducing the risk of associated chronic diseases.
If you suspect chronic inflammation, it is essential to consult with your healthcare provider. They can order specific blood tests to assess inflammatory markers in your body, such as C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and fasting insulin. These tests provide valuable insights into the presence and extent of inflammation, helping your physician develop an appropriate treatment plan.
Don’t wait until chronic inflammation leads to more serious health complications. Take action now to protect your well-being and prevent the development of chronic diseases. Your health is your most valuable asset, and addressing chronic inflammation is a vital step in safeguarding it.
Remember, you are in control of your health. By making conscious choices and adopting a proactive approach, you can reduce chronic inflammation, improve your well-being, and lead a vibrant life. Prioritize your health, make informed choices, and embrace a lifestyle that promotes well-being. Understanding the connection between chronic inflammation, metabolic syndrome, poor diet, and chronic diseases empowers you to break free from this harmful cycle and achieve better health and vitality. Start today and enjoy the long-term benefits of a life free from chronic inflammation. Your body will thank you for it.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
Exonerating Salt: Metabolic Syndrome Unveiled as the Underlying Culprit of Hypertension
- August 1, 2023
- Dr. Stephen Fitzmeyer, Dr. Sharon Lojun
- No Comments
By Stephen Fitzmeyer, MD
Introduction:
Hypertension, commonly known as high blood pressure, has long been associated with excessive salt intake. However, emerging research challenges this widely accepted belief, suggesting that hypertension is primarily a result of metabolic syndrome rather than a direct consequence of salt consumption. Metabolic syndrome, characterized by a cluster of metabolic abnormalities, including obesity, insulin resistance, and dyslipidemia, plays a pivotal role in salt retention and the development of hypertension. In this article, we will explore the misconceptions surrounding the salt hypothesis and delve into the intricate connection between metabolic syndrome and hypertension.
The Salt Paradox:
For decades, medical professionals and public health campaigns have emphasized reducing salt intake as a means to prevent and manage hypertension. However, the relationship between salt consumption and hypertension is not as straightforward as once believed. Numerous studies have failed to establish a consistent link between salt intake and blood pressure elevation. Furthermore, populations consuming low-salt diets have not demonstrated significant reductions in hypertension rates. This paradox raises questions about the true nature of the relationship between salt and hypertension.
Metabolic Syndrome: The Underlying Culprit:
Metabolic syndrome, a cluster of interconnected metabolic abnormalities, is now recognized as a significant contributor to hypertension. Obesity, insulin resistance, dyslipidemia, and chronic inflammation characteristic of metabolic syndrome disrupt the body’s delicate balance, leading to salt retention and the subsequent rise in blood pressure. Insulin resistance, a hallmark of metabolic syndrome, impairs sodium excretion by the kidneys, promoting salt retention and fluid accumulation. These metabolic derangements create a vicious cycle, perpetuating hypertension and further exacerbating the effects of salt retention.
Unveiling the Root Causes:
While salt intake may play a minor role in hypertension for a subset of individuals with salt sensitivity, it is crucial to focus on the underlying metabolic dysfunctions. Ultra-processed carbohydrates and fats, prevalent in modern diets, have been identified as primary culprits in the development of metabolic syndrome. These refined and heavily processed food products contribute to obesity, insulin resistance, and chronic inflammation, creating an environment conducive to hypertension and salt retention.
The Role of Lifestyle Interventions:
In addressing the underlying metabolic dysfunctions associated with hypertension, lifestyle interventions take center stage. A ketogenic diet, characterized by low carbohydrate intake and increased fat consumption, has shown promising results in improving metabolic health and blood pressure control. By shifting the body’s primary fuel source from carbohydrates to fats, a ketogenic diet improves insulin sensitivity, promotes weight loss, and mitigates chronic inflammation, thereby tackling the root causes of hypertension.
Intermittent fasting, an eating pattern that cycles between periods of fasting and feeding, has also demonstrated metabolic benefits. Beyond calorie restriction, intermittent fasting enhances insulin sensitivity, promotes autophagy, and regulates blood pressure, making it a valuable tool in the management of hypertension associated with metabolic syndrome.
Conclusion:
Contrary to the long-standing belief that salt intake is the primary driver of hypertension, the emerging evidence suggests that metabolic syndrome, with its associated metabolic dysfunctions, is the root cause of salt retention and subsequent development of hypertension. While salt sensitivity may play a role in some individuals, it is essential to address the broader metabolic context to effectively manage hypertension. Lifestyle interventions, such as adopting a ketogenic diet and incorporating intermittent fasting, offer promising strategies to reverse metabolic syndrome, improve metabolic health, and alleviate hypertension. By shifting the focus from salt intake to metabolic health, we can reframe our approach to hypertension management and pave the way for more effective prevention and treatment strategies.
Recent Posts
- Protected: Warp Core Health: Building a Custom AI Model for Transforming Healthcare
- The Intersection of Healthcare, AI, Clinical Informatics, and Machine Learning
- Accessing Siloed EMR Systems with FHIR: Connecting to Multiple EMRs
- How AI and Informatics Are Transforming Healthcare
- How AI Can Transform Healthcare Applications
Categories
- ApoB
- Artificial Intelligence
- Autophagy
- Biochemistry
- Biomedical Informatics
- Biostatistics
- Blood Glucose
- CAC
- Carbs
- CCD
- CDA
- Clinical Informatics
- Coding Bootcamp
- Coronary Artery Disease
- COVID-19
- Cybersecurity
- Data Science
- Diabetes
- Diet
- EHS
- EMR
- Epidemiology
- Evidence Based Medicine
- Fats
- FHIR
- Fiber
- Generative AI
- Global Health
- Health Administration
- Health Informatics
- Health IT
- HIPAA
- HL7
- Hyperglycemia
- Hypoglycemia
- ICD 10
- Intermittent Fasting
- Ketogenic Diet
- Machine Learning
- Macronutrients
- MCT Oil
- Metabolic Health
- Metabolic Syndrome
- Minerals
- Mitochondria
- MySQL
- Neurology
- Nutritional Ketosis
- Nutritional Neurology
- Nutritional Psychiatry
- PHP
- PHR
- Programming
- Prompt Engineering
- Proteins
- Prototypes
- Public Health
- Python
- Recipes
- Sleep Health
- Stroke
- Uric Acid
- Vegan and Vegetarians
- Vitamin D
- Vitamin K2
- Vitamins