- Home
- About
- Portfolio
- Crush the Match – Medical School and Residency Platform
- Food¢ense – Curbing Childhood Obesity and Food Waste
- HealthStack – Shared and Jailed HIPAA Hosting $50
- Marta Care – Let Us Help When You Can’t
- MD Idea Lab – We Build Prototypes for Doctors
- Nervcell – The Healthcare Web Browser
- Patient Keto – Personalized Keto Medicine and Telehealth
- SwipeChart – Rapid EMR Interface
- Treatment Scores – Quantifying the Science of Medicine
- Treatments – Diagnosed. Now What?
- VIDRIO – Google Glass and EMR Interface
- Blog
- Contact
Year: 2022
Understanding the Continuity of Care Document (CCD) in Healthcare
Stephen Fitzmeyer, MD
In healthcare, it is crucial to have an accurate and complete medical history for patients in order to provide the best possible care. The Continuity of Care Document (CCD) is a standard format for summarizing a patient’s medical history and care plan. It contains a concise summary of the patient’s health status, including medical conditions, medications, allergies, and other relevant information. In this article, we will explore the CCD in more detail, including its structure and use cases.
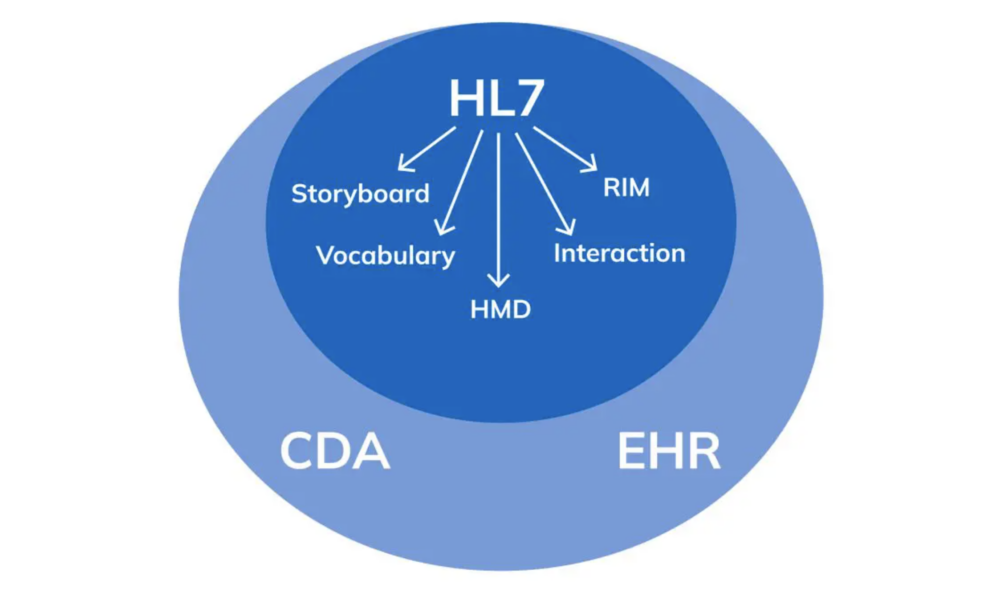
The CCD is based on the HL7 Clinical Document Architecture (CDA) standard, which provides a framework for structuring clinical documents. The CCD is designed to be a concise, easy-to-read summary of a patient’s health status that can be shared among healthcare providers. It includes information about the patient’s medical conditions, medications, allergies, immunizations, procedures, and laboratory results. The CCD also includes information about the patient’s care plan, such as goals, instructions, and recommended follow-up visits.
The CCD can be used in a variety of settings to improve care coordination and continuity. For example, a patient might be referred from a primary care physician to a specialist. By sharing the CCD, the specialist can quickly get up to speed on the patient’s medical history and current care plan, which can improve the quality of care and reduce the risk of medical errors. The CCD can also be used in emergency situations, where a patient might not be able to provide a complete medical history.
Here are some examples of how the CCD can be used:
Referrals: When a patient is referred from one healthcare provider to another, the referring provider can send a CCD to the receiving provider. This ensures that the receiving provider has all the necessary information to provide appropriate care.
Transitions of Care: When a patient is discharged from a hospital or other healthcare facility, a CCD can be sent to the patient’s primary care provider. This ensures that the primary care provider has all the necessary information to manage the patient’s care after discharge.
Emergency Situations: When a patient is brought to an emergency department, a CCD can be used to provide important medical information to the emergency department staff. This can help ensure that the patient receives appropriate care and treatment.
Patient Portals: Some healthcare organizations offer patient portals that allow patients to access their medical records online. The CCD can be used to provide a summary of the patient’s medical history and care plan in a format that is easy for patients to understand.
In conclusion, the CCD is a standard format for summarizing a patient’s medical history and care plan. It includes information about the patient’s medical conditions, medications, allergies, immunizations, procedures, and laboratory results. The CCD can be used in a variety of settings to improve care coordination and continuity, including referrals, transitions of care, emergency situations, and patient portals. By using the CCD, healthcare providers can improve the quality of care and reduce the risk of medical errors.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/
HL7: The Technicalities and Use Cases in Healthcare
By Stephen Fitzmeyer, MD
HL7 (Health Level Seven) is a widely adopted standard in healthcare for exchanging information between various healthcare applications, such as electronic health record systems, laboratory information systems, and radiology information systems. The standard defines a set of rules and formats for the exchange of clinical and administrative data. In this article, we will explore the technicalities of HL7 and provide examples of how it can be used in healthcare.
HL7 is composed of several messages, each containing one or more segments. Segments are made up of fields, and fields can contain subfields. Each segment contains information about a specific aspect of a patient’s clinical or administrative data. The most common message types in HL7 are the ADT (Admit, Discharge, Transfer), ORM (Order), and ORU (Observation Result) messages.
For example, an ADT message might contain information about a patient’s admission to the hospital, including their demographic information, admission date and time, and the admitting physician’s name. An ORM message might contain information about a laboratory test order, including the test name, patient’s name, and date and time the test was ordered. An ORU message might contain information about the results of a laboratory test, including the test name, patient’s name, and the actual test results.
HL7 can be used in a variety of ways to exchange data between healthcare applications. For example, a laboratory information system might send an ORU message to an electronic health record system when the results of a laboratory test are ready. The electronic health record system can then display the results to the provider, allowing them to make informed decisions about the patient’s care.
Another example is the use of HL7 in medical billing. A hospital’s billing system might receive ADT messages from an electronic health record system when a patient is admitted, transferred, or discharged. The billing system can then use this information to generate a claim for payment from the patient’s insurance company.
In addition to facilitating data exchange between healthcare applications, HL7 can also be used to integrate clinical decision support systems (CDSS) into electronic health record systems. CDSS systems can analyze patient data and provide recommendations to providers, such as suggesting alternative medications or highlighting potential drug interactions. By integrating CDSS systems with electronic health record systems using HL7, providers can make more informed decisions and improve patient outcomes.
In conclusion, HL7 is a widely adopted standard in healthcare for exchanging clinical and administrative data between various healthcare applications. HL7 messages contain segments and fields that contain patient data, and there are several message types used for different purposes. HL7 can be used to exchange data between applications, integrate CDSS systems into electronic health record systems, and facilitate medical billing. By adopting HL7, healthcare providers can improve patient outcomes and streamline administrative processes.
Author: Stephen Fitzmeyer, M.D.
Physician Informaticist
Founder of Patient Keto
Founder of Warp Core Health
Founder of Jax Code Academy, jaxcode.com
Connect with Dr. Stephen Fitzmeyer:
Twitter: @PatientKeto
LinkedIn: linkedin.com/in/sfitzmeyer/